Predictors of arterial desaturation during intubation: a nested case-control study of airway management—part I
Introduction
Endotracheal intubation (ETI) is one of the most commonly performed procedures in the intensive care unit (ICU), occurring at a rate of 69% in one report (1). ETI can be life-saving for patients presenting with acute respiratory failure from numerous causes. However, if the clinician is not vigilant during the procedure, complications can arise that may impact the overall outcome of patients. In addition, ETI carried out in the ICU, as compared to other environments, can be associated with increased complications, likely resulting from the lack of time for optimization before ETI as well as patient-related factors (1-3). Moreover, the incidence of difficult airway in the ICU compared to the operating room may be as high as 23% (2). Thus, it is of vital importance that this procedure is carried out with utmost attention to detail in the critically ill.
Recognizing the impact of complications experienced during ETI, several institutions have adopted pre-intubation checklists, intubation bundles, and/or other airway monitoring equipment to reduce these complications. Studies suggest that the use of a systematic approach to or protocol for airway management can reduce intubation complications (4-6). This was recently demonstrated in a prospective trial utilizing an intubation management protocol whereby immediate severe life-threatening complications associated with intubation of ICU patients were reduced (7).
In absolute terms, ETI can be viewed from two perspectives: (I) airway management and (II) hemodynamic management. Regarding airway management, failed, difficult or delayed intubation is commonly associated with hypoxia, which in turn, leads to further complications (8). Reported risk factors for an airway complication such as the above include failure to use neuromuscular blockers, increased body mass index, and repeated intubation attempts (9-11). In addition, the use of newer techniques may be protective against difficult tracheal intubation and thus hypoxia as demonstrated in some studies (12,13). Herein, we report the results of a nested case control study identifying predictors of arterial desaturation (hypoxemia) occurring during intubations in the ICU over the last 2 years at Mayo Clinic Rochester by collecting data on airway management in the peri-intubation period. Secondary aims were to report short-term outcomes of those who developed arterial desaturation compared to those who did not. A subsequent report follows identifying predictors of an immediate hemodynamic complication in the peri-intubation period.
Methods
The present study was deemed exempt from the institutional review board at Mayo Clinic Rochester, Minnesota. All patients included in this study gave prior research authorization for the use of their data towards research.
Study design
We conducted a nested case control study on a previously reported cohort of adult (≥18 years) critically ill patients admitted to a medical and/or surgical ICU at Mayo Clinic Rochester, MN, requiring emergent and non-emergent ETI during the time period of January 1st 2013 to December 31st 2014 (14). ETIs performed outside the ICU were excluded. For the primary aim, data on airway management was collected during the peri-intubation period. The peri-intubation period was defined as 60 minutes pre- and post- intubation. We defined arterial desaturation associated with ETI as hypoxemia (pulse oximetry reading <90%) occurring at any time 30 minutes following ETI. Hypoxia was chosen as a surrogate for immediate airway complication rather than failed or difficult tracheal intubation or other causes of airway perturbations as hypoxia was the most common cause of death in the 4th National Audit Project of the Royal College of Anaesthetists and Difficult Airway Society (15,16). Once identified within the cohort, patients were then classified as cases (those who experienced hypoxia) and controls (those who did not experience this complication). We defined a rapid sequence induction as the administration of a short-acting induction agent (propofol, etomidate, ketamine) and succinylcholine or rocuronium (>1.0 mg/kg) to achieve rapid loss of consciousness and paralysis, the application of cricoid pressure (Sellick maneuver), and securing of the airway without insufflation to avoid regurgitation (17). Patients intubated at our institution are routinely provided with bag mask ventilation immediately prior to ETI. Immediately after ETI, we routinely place patients on 100% inspired oxygen concentration and practice lung protective ventilation at our institution with the aim to reduce airway pressures to less than 30 mmHg.
For all data collection, a standardized case report form was utilized. All study personnel were trained on the case report form prior to data entry (Mohamed O. Seisa, Katherine J. Heise, Robert A. Kyle D. Busack, Theodore O. Loftsgard).
In addition, short-term outcomes were measured in both groups which included the number of days of mechanical ventilation, the length of stay, and vital status (dead or alive) (Nathan J. Smischney, Daniel A. Diedrich).
Statistical analysis
Continuous measurements are expressed as mean ± standard deviation (SD) or median and interquartile range (IQR) and categorical variables are reported as counts and percentages. Characteristics are compared between those who experienced arterial desaturations versus not using the two-sample t-test, or rank sum test, for continuous variables and the chi-square test for categorical variables. In addition to these univariate comparisons, two multivariable logistic regression analyses were performed. For the initial multivariable analysis, the explanatory variables of interest included acute respiratory failure as the indication for intubation, body weight, emergency procedure, and provider level (consultant, fellow, resident). For the second multivariable analysis, the Acute Physiologic And Chronic Health Evaluation (APACHE) III score and SaO2 prior to intubation were included as additional explanatory variables. The results of the multivariable analyses are summarized using the ORs and corresponding 95% CIs. In all cases, a two-tailed P of ≤0.05 is considered to indicate statistical significance.
Sample size
The sample size for the current investigation (74 cases, 346 controls) is fixed based on the number of arterial desaturations observed in our previously reported cohort (14). In general, when comparing a continuous variable between groups this sample-size provides statistical power (two-tailed, alpha =0.05) of >80% to detect a difference between groups of 0.4 SD units; and for a binary risk factor the minimum detectable OR is 2.25.
Results
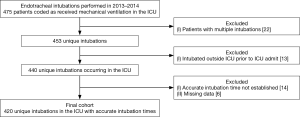
The final cohort included 420 analyzable patients. A total of 74 patients experienced arterial desaturation, representing an incidence rate of 18% with 346 patients not experiencing this event (Figure 1). Patients who experienced arterial desaturation were of lower age (62.1±17.2 vs. 63.0±16.1; P=0.655), male gender [45 (60.8) vs. 199 (57.5); P=0.602], and higher weight (86.2±33.1 vs. 84.5±28.6; P=0.639). Patients with arterial desaturations had significantly higher illness severity [APACHE 3 score at 24 hours of ICU admission (89.6±33.8 vs. 82.6±25.0); P=0.041]. A history of obstructive lung disease did not lead to increased odds of experiencing arterial desaturation (19%—no arterial desaturation vs. 10%—arterial desaturation). However, intubating patients with acute respiratory failure was associated with experiencing arterial desaturation [61 (82.4) vs. 221 (63.9); P=0.002]. On the contrary, intubating for airway protection and/or for a procedure resulted in decreased odds of experiencing arterial desaturation (Table 1).
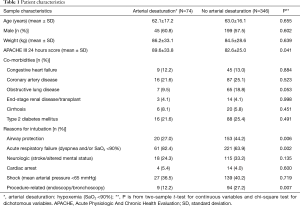
Full table
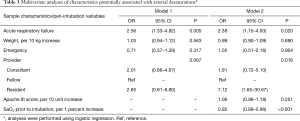
Regarding the peri-intubation variables, patients who had decreased pulse oximetry readings prior to ETI tended to develop arterial desaturation. Thus, higher pulse oximetry readings prior to ETI was protective as shown in the multivariate model (OR 0.92; 95% CI: 0.89–0.96; P<0.01; per one percent increase). The training level of the provider also influenced whether patients developed arterial desaturation with junior trainees leading to the highest odds (OR 7.12; 95% CI: 1.65–30.67; P=0.016) (Tables 2,3). Although not significant, patients who developed arterial desaturation were more likely to be intubated with Miller direct laryngoscopy [21 (28.4)] as compared to those who did not develop arterial desaturation [57 (16.5)] (Table 2).
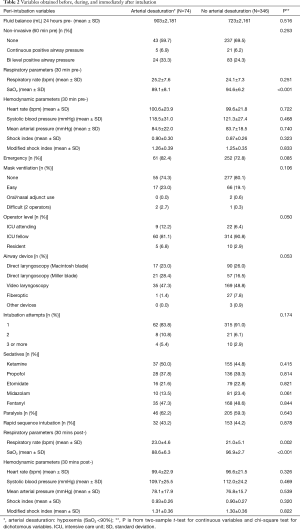
Full table
Full table
We ran two multivariate models. One model included known predictors of difficult airway such as weight, emergent nature of procedure, age, and provider level. We then ran a second multivariate model to include additional significant predictors on univariate analyses. Both models demonstrated that intubating for acute respiratory failure resulted in increased odds of arterial desaturation, in addition to the provider level and lower pulse oximetry readings prior to ETI (Table 3).
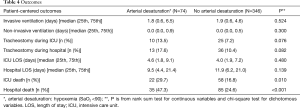
Patients who experienced arterial desaturation were less likely to survive their ICU [22 (29.7) vs. 58 (16.8); P=0.01] and hospital [35 (47.3) vs. 85 (24.6); P<0.01] stay as compared to those who did not experience this complication. There was no difference between the groups for other short-term outcomes analyzed (Table 4).
Full table
Discussion
We investigated potential predictors of arterial desaturation experienced during the peri-intubation period in case-control study nested within a cohort of critically ill patients who received ETI in the ICU. As a surrogate for an airway event, we choose hypoxemia as defined by pulse oximetry readings <90% at any time during the peri-intubation period. Rather than choosing difficult airway as a surrogate, which is prone to subjectiveness, we wanted to be more sensitive and capture a greater number of patients experiencing airway events. Hypoxia is typically associated with difficult airway and thus, our definition would capture this. Difficult airway has an incidence of roughly 12% in the ICU (18). Given the above, we would expect our point estimate to be higher. Not surprisingly, using our definition, we arrived at an incidence of 18%.
Current literature suggests that the use of newer techniques to intubate the trachea such as video laryngoscopy result in better laryngeal view and improved intubation difficulty score when compared with conventional techniques (direct laryngoscopy) with an increase in time to intubate (19-23). In fact, video laryngoscopy maintains its effectiveness in inexperienced personnel as demonstrated by a recent study (24). A recent systematic review and meta-analysis of video laryngoscopy versus direct laryngoscopy demonstrated similar findings with video laryngoscopy reducing the risk of difficult ETI, Cormack 3/4 grades, and esophageal intubation and increased the first-attempt success. No statistically significant difference was found for severe hypoxemia, severe cardiovascular collapse, or airway injury (25). Moreover, video laryngoscopy also shows promise when used emergently (26). However, not all providers who practice in a critical care setting utilize the newer modalities, possibly due to lack of experience and familiarity with the newer techniques or evidence suggesting no benefit (27,28). As an example, a recent survey among Canadian resuscitation physicians (intensive care and emergency medicine physicians) demonstrated that the majority utilize direct laryngoscopy with a MacIntosh blade as a primary device for emergent ETIs. Paralysis for intubation was not used in the majority of cases, but was more likely to be used by emergency medicine physicians (29). A survey of airway management techniques used among ICU physicians in Israel demonstrated that fiberoptic intubation is routine for airway management rather than other devices (30). We did not find that the use of certain airway devices resulted in reduced incidence of arterial desaturation. However, video laryngoscopy was the primary airway modality used in both groups, consistent with our prior investigation (31). Interestingly though, patients who experienced arterial desaturation had a higher use of Miller direct laryngoscopy performed as compared to the group that did not develop this complication. We hypothesize that junior level trainees have an easier time with Macintosh direct laryngoscopy than Miller direct laryngoscopy as video laryngoscopy is essentially a modified Macintosh blade.
We did find that the training level of the operator performing ETI was associated with an increased risk of arterial desaturation. Our finding is consistent with previous literature. For example, Jaber et al. evaluated 253 occurrences of TI in 7 ICUs. ETI performed by a junior physician supervised by a senior (i.e., two operators) was identified as a protective factor. Another study examined 322 patients who required emergent ICU intubation. A total of 115 were intubated with senior level supervision, whereas 207 where intubated by junior level trainees in the absence of senior level supervision. The authors found that supervision by an expert was associated with a significant decrease in complication (18,32).
It stands to reason that somebody in acute extremis prior to ETI would likely experience airway related complications. Our results support the above finding. We found that patients who were intubated for acute respiratory failure and those with hypoxia prior to ETI had a higher rate of arterial desaturation. We speculate that these patients were not recognized early enough in their time course to avoid this complication. A number of studies point to the use of non-invasive ventilation to alleviate acute respiratory failure and potentially avoid ETI. For example, Gregoretti et al. found that non-invasive ventilation may decrease morbidity and mortality by reducing complications and infections associated with invasive mechanical ventilation. Other studies examining non-invasive ventilation have shown increased use in last 15 years due to its success rate and an overall decrease in mortality (33,34). Despite a slightly higher use of bi-level positive airway pressure in the cases (33% vs. 24%), we may have underutilized non-invasive ventilation in those in extremis prior to ETI. Thus, early identification of respiratory distress may be important prior to hypoxia and overt respiratory distress with improved mortality.
We included positive predictors noted on univariate analysis in the multivariate model. However, we also included known predictors of difficult airways such as obesity, emergent nature of intubation and operator level (8). Overall, we found that operator level of intubating provider as well as intubating patients for acute respiratory failure (in extremis) was associated with arterial desaturation. Having a higher pre-existing pulse oximetry reading was protective.
We did not find any difference in outcomes with regard to ICU and hospital length of stay or mechanical ventilation days. However, patients experiencing arterial desaturation had higher mortality as compared to controls. Not surprising, hypoxemia results in added stress to an already stressed system, which could result in unwanted consequences as illustrated in the literature (35-37). In addition, it’s been shown that proning patients decreases mortality and the major physiologic impact is an increase in their arterial oxygen. Finally, the hypoxia seen may be a progression of acute lung injury.
The current study has several limitations. First and most important was the use of hypoxemia as a surrogate for an airway event. The use of our definition led to a high incidence of airway events which may be an indicator that we chose a non-specific and overly sensitive definition. Furthermore, one can infer that hypoxia in the operating room setting is more likely a result of airway difficulty versus the ICU setting where hypoxia may pre-exist prior to ETI, as seen in the current study. The pre-existing hypoxia may have confounded the mortality outcomes. Thus, an analysis of a relative decrease in O2 saturations or a comparison of early versus late desaturations in relation to outcomes may have yielded different results. However, rather than using difficult airway as a surrogate, we choose to encompass broader category of patients and thus, we choose to be more sensitive than specific. In addition, this study adds to the current literature by exploring outcomes of pre- and post-intubation hypoxia in critically ill patients. Second, details on supplemental oxygen use prior to ETI were of poor quality in the electronic medical record upon retrospective review. This data was incomplete and thus was not used in the analysis. Third, our sample size was small which led to wide confidence intervals for some point estimates we examined (i.e., operator level). Fourth, data was captured via the electronic health record retrospectively. Thus, missing data and/or inaccurate data may have resulted in some of our findings. Fifth, these findings may not be generalizable to other institutions.
Conclusions
We found a relatively high incidence of arterial desaturations in our cohort. Known risk factors associated with a difficult airway and hence hypoxia (definition used in the current study) did not result in increased risk of experiencing arterial desaturation. Rather, patients not identified earlier in their clinical deterioration are more likely to decompensate as demonstrated in this study (intubation for acute respiratory distress and pre-existing hypoxia). Furthermore, inexperienced intubating providers are more likely to have arterial desaturations as compared to experienced intubating providers. This study sheds light on the fact that early recognition is paramount to preventing arterial desaturations as defined in our study and that possibly early intubation in these patients may improve their trajectory in the course of their critical illness.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: This work was supported by the Division of Critical Care Medicine with no direct financial support.
References
- Simpson GD, Ross MJ, McKeown DW, et al. Tracheal intubation in the critically ill: a multi-centre national study of practice and complications. Br J Anaesth 2012;108:792-9. [Crossref] [PubMed]
- Heuer JF, Barwing TA, Barwing J, et al. Incidence of difficult intubation in intensive care patients: analysis of contributing factors. Anaesth Intensive Care 2012;40:120-7. [PubMed]
- Griesdale DE, Bosma TL, Kurth T, et al. Complications of endotracheal intubation in the critically ill. Intensive Care Med 2008;34:1835-42. [Crossref] [PubMed]
- Niven AS, Doerschug KC. Techniques for the difficult airway. Curr Opin Crit Care 2013;19:9-15. [Crossref] [PubMed]
- Noppens RR. Airway management in the intensive care unit. Acta Clin Croat 2012;51:511-7. [PubMed]
- Divatia JV. The intubation bundle: Towards safer tracheal intubation in critically ill patients. Critical Care & Shock 2012;15:52.
- Jaber S, Jung B, Corne P, et al. An intervention to decrease complications related to endotracheal intubation in the intensive care unit: a prospective, multiple-center study. Intensive Care Med 2010;36:248-55. [Crossref] [PubMed]
- Cook TM, MacDougall-Davis SR. Complications and failure of airway management. Br J Anaesth 2012;109 Suppl 1:i68-i85. [Crossref] [PubMed]
- Lundstrøm LH, Møller AM, Rosenstock C, et al. Avoidance of neuromuscular blocking agents may increase the risk of difficult tracheal intubation: a cohort study of 103 812 consecutive adult patients recorded in the Danish Anaesthesia Database. Br J Anaesth 2009;103:283-90. [Crossref] [PubMed]
- Lundstrøm LH, Møller AM, Rosenstock C, et al. High body mass index is a weak predictor for difficult and failed tracheal intubation: a cohort study of 91,332 consecutive patients scheduled for direct laryngoscopy registered in the Danish Anesthesia Database. Anesthesiology 2009;110:266-74. [PubMed]
- Mort TC. Emergency tracheal intubation: complications associated with repeated laryngoscopic attempts. Anesth Analg 2004;99:607-13. [Crossref] [PubMed]
- Aziz MF, Healy D, Kheterpal S, et al. Routine clinical practice effectiveness of the Glidescope in difficult airway management: an analysis of 2,004 Glidescope intubations, complications, and failures from two institutions. Anesthesiology 2011;114:34-41. [Crossref] [PubMed]
- Mihai R, Blair E, Kay H, et al. A quantitative review and meta-analysis of performance of non-standard laryngoscopes and rigid fibreoptic intubation aids. Anaesthesia 2008;63:745-60. [Crossref] [PubMed]
- Smischney NJ, Seisa MO, Heise KJ, et al. Practice of intubation of the critically ill at Mayo Clinic. J Intensive Care Med 2017. [Epub ahead of print]. [Crossref] [PubMed]
- Cook TM, Woodall N, Harper J, et al. Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 2: intensive care and emergency departments. Br J Anaesth 2011;106:632-42. [Crossref] [PubMed]
- Cook TM, Woodall N, Frerk C. Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: anaesthesia. Br J Anaesth 2011;106:617-31. [Crossref] [PubMed]
- Sellick BA. Cricoid pressure to control regurgitation of stomach contents during induction of anaesthesia. Lancet 1961;2:404-6. [Crossref] [PubMed]
- Jaber S, Amraoui J, Lefrant JY, et al. Clinical practice and risk factors for immediate complications of endotracheal intubation in the intensive care unit: a prospective, multiple-center study. Crit Care Med 2006;34:2355-61. [Crossref] [PubMed]
- Sandhu H, Gombar S, Kapoor D. A comparative evaluation of glide scope and Macintosh laryngoscope for endotracheal intubation. Indian J Crit Care Med 2014;18:S9.
- Mosier JM, Whitmore SP, Bloom JW, et al. Video laryngoscopy improves intubation success and reduces esophageal intubations compared to direct laryngoscopy in the medical intensive care unit. Crit Care 2013;17:R237. [Crossref] [PubMed]
- Lakticova V, Koenig SJ, Narasimhan M, et al. Video laryngoscopy is associated with increased first pass success and decreased rate of esophageal intubations during urgent endotracheal intubation in a medical intensive care unit when compared to direct laryngoscopy. J Intensive Care Med 2015;30:44-8. [Crossref] [PubMed]
- Noppens RR, Geimer S, Eisel N, et al. Endotracheal intubation using the C-MAC(R) video laryngoscope or the Macintosh laryngoscope: a prospective, comparative study in the ICU. Crit Care 2012;16:R103. [Crossref] [PubMed]
- De Jong A, Clavieras N, Conseil M, et al. Implementation of a combo videolaryngoscope for intubation in critically ill patients: a before-after comparative study. Intensive Care Med 2013;39:2144-52. [Crossref] [PubMed]
- Itai J, Tanabe T, Nishida T, et al. Tracheal intubation for a difficult airway using Airway scope®, KingVision® and McGRATH®: a comparative manikin study of inexperienced personnel. Crit Care 2013;17:159. [PubMed]
- De Jong A, Molinari N, Conseil M, et al. Video laryngoscopy versus direct laryngoscopy for orotracheal intubation in the intensive care unit: a systematic review and meta-analysis. Intensive Care Med 2014;40:629-39. [PubMed]
- Lee DH, Han M, Jung JY, et al. Comparison of tracheal intubation using conventional direct laryngoscope and video laryngoscope during unexpected cardiopulmonary resuscitation. Intensive Care Med 2014;40:S271:A1030.
- Ural K, Subaiya C, Taylor C, et al. Analysis of orotracheal intubation techniques in the intensive care unit. Crit Care Resusc 2011;13:89-96. [PubMed]
- Harper Y, Waheed I, Ehsanullah B, et al. Does it matter who intubates patients? A comparison of endotracheal intubation practice patterns. Crit Care Med 2014;42:A1561. [Crossref]
- Green RS, Fergusson DA, Turgeon AF, et al. Device and Medication Preferences of Canadian Physicians for Emergent Endotracheal Intubation in Critically Ill Patients. CJEM 2017;19:186-97. [Crossref] [PubMed]
- Haviv Y, Ezri T, Boaz M, et al. Airway management practices in adult intensive care units in Israel: a national survey. J Clin Monit Comput 2012;26:415-21. [Crossref] [PubMed]
- Seisa MO, Gondhi V, Demirci O, et al. Survey on the current state of endotracheal intubation among the critically ill: HEMAIR investigators. J Intensive Care Med 2016. [Epub ahead of print]. [Crossref] [PubMed]
- Schmidt UH, Kumwilaisak K, Bittner E, et al. Effects of supervision by attending anesthesiologists on complications of emergency tracheal intubation. Anesthesiology 2008;109:973-7. [Crossref] [PubMed]
- Gregoretti C, Pisani L, Cortegiani A, et al. Noninvasive ventilation in critically ill patients. Crit Care Clin 2015;31:435-57. [Crossref] [PubMed]
- Demoule A, Chevret S, Carlucci A, et al. Changing use of noninvasive ventilation in critically ill patients: trends over 15 years in francophone countries. Intensive Care Med 2016;42:82-92. [Crossref] [PubMed]
- Weingart SD, Trueger NS, Wong N, et al. Delayed sequence intubation: a prospective observational study. Ann Emerg Med 2015;65:349-55. [Crossref] [PubMed]
- Khandelwal N, Khorsand S, Mitchell SH, et al. Head-Elevated Patient Positioning Decreases Complications of Emergent Tracheal Intubation in the Ward and Intensive Care Unit. Anesth Analg 2016;122:1101-7. [Crossref] [PubMed]
- Mosier JM, Joshi R, Hypes C, et al. The Physiologically Difficult Airway. West J Emerg Med 2015;16:1109-17. [Crossref] [PubMed]