Thoracoscopic resection of a huge mediastinal cystic lymphangioma
Introduction
Cystic lymphangioma is a rare congenital benign tumor, generally considered as the local proliferation of differentiated lymphoid tissue in the development of the lymphatic system. This disease occurs in various areas of the body, with the most common location at the neck, occasionally the axilla or groin, and rarely in the mediastinum (1). No obvious symptoms are found in patients with mediastinal cystic lymphangioma, so imaging examinations are the main methods to identify the lesion. However, definitive histological diagnosis is difficult to achieve before surgery (2). Malignant transformation of cystic lymphangioma has not been reported, but complete surgical resection is generally recommended. Traditionally, surgical resection was performed via open thoracotomy. Here, we report a rare case of an isolated huge mediastinal cystic lymphangioma in an adult patient that was successfully resected by video-assisted thoracoscopic surgery (VATS).
Case presentation
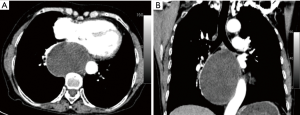
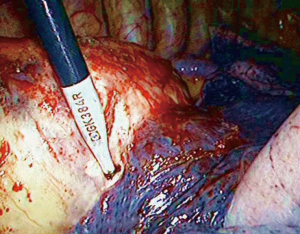
A 69-year-old woman was admitted in the hospital complaining of chest distress for over 1 month. Clinical and family histories were uneventful. It is particularly important to note that the patient had no history of living in endemic areas of the hydatid disease. Physical examination was normal. Contrast-enhanced chest computed tomography (CT) revealed a 10.5 cm × 7.5 cm cystic mass (Figure 1) in the posterior mediastinum adjacent to the left main bronchial wall and the descending thoracic aorta. The mass had regular borders and showed no enhancement after administration of contrast medium. Its preoperative diagnosis was indefinite. Tumor resection was performed via right VATS. Thoracoscopic exploration found that the tumor adhered to the right lung, azygos vein and descending aorta (Figure 2). The pedicle was connected to the thoracic duct. The adhesions between the right lung and the tumor were divided with scissors. The lesion was a 12 cm × 8 cm cyst containing fluid in the posterior mediastinum, that was adherent to the surrounding organs. Due to the large size of the cyst, the whole lesion could not be properly assessed, and decompression of the cyst was performed to allow for maneuverability. About 500 mL of milky liquid was aspirated and then the cyst wall was completely removed. The pedicle and thoracic duct were carefully ligated.
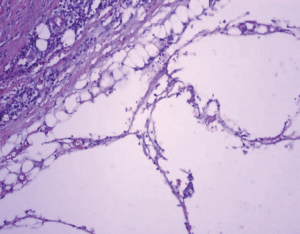
Postoperative pathologic diagnosis of the tumor was confirmed to be cystic lymphangioma (Figure 3). Postoperative course was uneventful. After 2 years of follow-up, there were no signs of recurrence.
Discussion
Cystic lymphangioma is a rare congenital benign tumor with an incidence rate of less than 1% in the mediastinum (2). Patients with mediastinal cystic lymphangioma usually have no specific symptoms. Most cystic lymphangiomas are not diagnosed during childhood until they grow very large. CT and lymphangiography are helpful in determining the extent of the disease, the size of the cyst, and the lymphatic nature of the mass. Magnetic resonance imaging (MRI) is also used to demonstrate the relationship of the mass with the surrounding structures (3). Aspiration biopsy, which is prohibited if pulmonary echinococcosis is suspected, improves the diagnostic rate of the disease, but the final diagnosis requires histopathologic examination of the resected specimen. Thymic cysts, Castleman’s disease, bronchogenic cysts, pericardial cysts, cystic teratomas and pulmonary echinococcosis should be kept in mind in the differential diagnosis of cystic lymphangioma. Special attention should be paid to pulmonary echinococcosis, which is common in endemic areas and patients with pulmonary hydatid disease often have a history of contact with sheep and horses. Casoni test can assist the diagnosis before operation. If pulmonary echinococcosis is suspected, first of all, thoracoscopic surgery should be performed carefully to avoid accidental rupture of the cyst, which may lead to serious consequences, for example, severe allergic reactions and scolex spread. Secondly, 10% hypertonic saline gauze pads could be placed around the puncture point to protect the chest before pricking the cyst for maneuverability during thoracoscopic surgery. Although most patients are asymptomatic, surgical intervention is required to prevent compression of the peripheral tissues by progressive tumor enlargement, chylous mediastinum, chylothorax or secondary infection. In order to obtain an excellent exposure, surgical resection through an open thoracotomy approach is the traditional approach. Proper incisions (posterior-lateral, anterior-lateral and median sternotomy incisions, among others) can be chosen according to tumor location, size, and relationship with the peripheral tissues and organs. However, these open approaches are associated with significant postoperative pain and require long hospital stays. With the development of minimally invasive techniques, several studies have focused on VATS for the treatment of mediastinal cystic lymphangioma (4,5). VATS for treatment of mediastinal lymphangioma remains difficult, and complete excision still remains to be technically problematic because of the peripheral adhesions of the tumor. These should be carefully managed to avoid injuries of azygos vein, aorta, bronchus, recurrent laryngeal nerve, phrenic nerve, etc. The objective of the operation should be the complete resection of the lesion, because incomplete resection can result in recurrence of the cyst.
Although other types of treatment, such as radiotherapy or injection of sclerosing agents, have been proposed, they are still controversial (3). The patient in this case report underwent a thoracoscopic resection. Intraoperative exploration found that the tumor pedicle was connected to the thoracic duct. The pedicle was ligated carefully through thoracoscopic view. The postoperative clinical course was satisfactory, without any complications. No signs of recurrence occurred during the 2-year follow-up.
In conclusion, we encountered a rare case of a huge mediastinal cystic lymphangioma in an adult woman. The tumor was difficult to diagnose before surgery, and complete surgical resection was proposed for therapeutic purposes. This case report shows that resection by VATS is feasible for huge mediastinal cystic lymphangioma in adult patients and that VATS can be a good alternative to open procedures.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Brown LR, Reiman HM, Rosenow EC 3rd, et al. Intrathoracic lymphangioma. Mayo Clin Proc 1986;61:882-92. [Crossref] [PubMed]
- Kanzaki M, Kikkawa T, Obara T, et al. Successful excision of an isolated mediastinal cystic lymphangioma with bilateral thoracoscopic surgery. Ann Thorac Cardiovasc Surg 2011;17:570-2. [Crossref] [PubMed]
- Yildirim E, Dural K, Kaplan T, et al. Cystic lymphangioma: report of two atypical cases. Interact Cardiovasc Thorac Surg 2004;3:63-5. [Crossref] [PubMed]
- Hunt I, Eaton D, Dalal P, et al. Minimally invasive excision of a mediastinal cystic lymphangioma. Can J Surg 2009;52:E201-2. [PubMed]
- Lazopoulos G, Pavlopoulos D, Kambitakis E, et al. Huge cystic lymphangioma of the mediastinum successfully treated with thoracoscopic surgery. Ann Thorac Surg 2014;98:2233. [Crossref] [PubMed]


