Corticosteroid monotherapy in a case of bronchocentric granulomatosis with a two-year follow-up
Bronchocentric granulomatosis (BCG), which was first described by Liebow (1) in 1973, is a rare disease characterized by inflammation that begins within and is centered around the walls of bronchioles and manifests as fever, cough, wheezing, dyspnea, and blood eosinophilia. It is considered to occur primarily in asthmatic patients and to be closely related to fumigatus infection (2-4).
Because of the possibility of fungal infection, BCG is usually treated with corticosteroids and an antifungal agent (5). However, fungi are not detected in all BCG tissues. The question thus arises of whether antifungal agents should be used in addition to corticosteroids in these patients. We here report a case of biopsy-proven BCG without accompanying fungal infection in a woman who was treated with corticosteroids alone and followed-up for two years.
Case presentation
A 43-year-old woman presented with a severe cough, malaise, and frothy sputum containing gray-black particles similar to rice (Figure 1A). The woman did not have a fever or a smoking history. Moreover, she had no prior history suggestive of asthma or atopy. The gray rice-like particles in the sputum were shown by microscopy to be composed of eosinophils and Charcot-Leyden crystals (Figure 1B). A silver methenamine stain revealed that there was no fungal infection, and the Ziehl-Neelsen stain was also negative. Laboratory investigations showed a white cell count of 7.29×109/L and an increased eosinophil ratio of 24.8%. Her erythrocyte sedimentation rate (ESR) was 45 mm/h. In addition, serum total IgE was increased to 150 IU/mL (normal <100 IU/mL). Serum fungal precipitins were found to be negative by an immunodiffusion technique. Serological tests for ANA, RF, ANCA, and HIV antibodies were also negative, as were the sputum cultures. Pulmonary function tests revealed normal lung volumes, flows, and transfer factor.
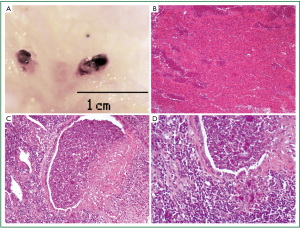
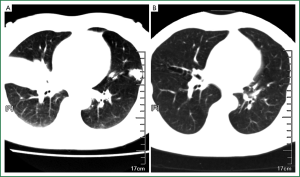
A high-resolution CT scan of the woman’s chest revealed lobar and segmental consolidation and atelectasis (Figure 2A), and bronchoscopic examination with a transbronchial lung biopsy showed non-specific chronic inflammation. The woman underwent an open lung biopsy of the left lung. Heavy consolidation and atelectasis, close-grained lesions, and bronchiectasis were found upon gross inspection. Microscopy revealed dilatation of the bronchiolar lumens which were filled with mucinous material and eosinophils, and characterized by epithelial necrosis and degenerated inflammatory cells. The area surrounding the bronchioles was characterized by eosinophilia and chronic inflammatory cell infiltration. Higher magnification images of the bronchiolar lumens revealed that part of the mucosa had fallen off and had been replaced by epithelioid histiocytes. As mentioned earlier, silver methenamine staining revealed no fungal infection of the airways or tissues and other stains, including the Ziehl-Neelsen stain, were also negative. The pathology was diagnostic of BCG.
The patient was prescribed methylprednisolone 50 mg every morning (1 mg·kg-1 body weight), which was reduced by 4 mg every half month. Half a year later, she was weaned off methylprednisolone. Complete remission of cough and sputum and normalization of ESR (45 to 12 mm/h), blood eosinophilia (24.8% to 4.5%) and total IgE level (150 to 25 IU/mL) occurred within one month. A CT scan performed after one month of treatment showed a marked decrease in both the size and density of the lung masses previously observed. The patient was followed-up for two years and had a CT scan every six months. After one year, her CT scan showed that the lung masses had totally disappeared and only a few signs of bronchiectasis remained (Figure 2B). She continues to do well two years after treatment.
Discussion
Because of the possibility of fungal infection, empiric antifungal therapy and corticosteroids are commonly prescribed for BCG (4). For patients with explicit evidence of fungal infection antifungal agents are beneficial, but in some patients a lung biopsy and other examinations do not detect any evidence of fungal infection. It is difficult to decide whether empiric antifungal therapy is essential for BCG patients without any evidence of fungal infection because of the liver and kidney toxicity associated with the use of antifungal agents. Only a few cases of successfully treatment with corticosteroids alone have been reported to date (6).
In the present case, the patient accepted a protocol involving corticosteroid monotherapy with close follow-up to facilitate treatment of a possibly worsening condition. Fortunately, her condition improved rapidly and she was successfully treated with corticosteroid monotherapy, which was confirmed during the two-year follow-up. The outcome in this case added to the body of evidence indicating that BCG without any signs of a fungal infection can be treated by corticosteroids alone provided they are closely followed-up.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Liebow AA. The J. Burns Amberson lecture--pulmonary angiitis and granulomatosis. Am Rev Respir Dis 1973;108:1-18. [PubMed]
- Goodman DH, Sacca JD. Pulmonary cavitation, allergic aspergillosis, asthma and bronchocentric granulomatosis. Chest 1977;72:368-9. [PubMed]
- Hanson G, Flor N, Wells I, et al. Bronchocentric granulomatosis: a complication of allergic bronchopulmonary aspergillosis. J Allergy Clin Immunol 1977;59:83-90. [PubMed]
- Koss MN, Robinson RG, Hochholzer L. Bronchocentric granulomatosis. Hum Pathol 1981;12:632-8. [PubMed]
- Jelihovsky T. The structure of bronchial plugs in mucoid impaction, bronchocentric granulomatosis and asthma. Histopathology 1983;7:153-67. [PubMed]
- Rossi GP, Pavan E, Chiesura-Corona M, et al. Bronchocentric granulomatosis and central diabetes insipidus successfully treated with corticosteroids. Eur Respir J 1994;7:1893-8. [PubMed]


