|
References
- CJA Haasbeek, S Senan, EF Smit, MA Paul, BJ Slotman, FJ Lagerwaard.
Critical Review of Non-Surgical Treatment Options for Stage I Non-Small
Cell Lung Cancer. Oncologist 2008;13:309-19.[LinkOut]
- Palma D, Senan S. Stereotactic radiation therapy: changing treatment
paradigms for stage I non-small cell lung cancer. Curr Opin Oncol 2011;23:133-9.[LinkOut]
- Baumann P, Nyman J, Hoyer M, Wennberg B, Gagliardi G, Lax I, et al. Outcome in a prospective phase II trial of medically inoperable stage I nonsmall-cell lung cancer patients treated with stereotactic body radiotherapy.
J Clin Oncol 2009;27:3290-6.[LinkOut]
- Timmerman R, Paulus R, Galvin J, Michalski J, Straube W, Bradley J, et al.
Stereotactic body radiation therapy for inoperable early stage lung cancer.
JAMA 2010;303:1070-6.[LinkOut]
- Grutters JPC, Kessels AGH, Pijls-Johannesma M, De Ruysscher D, Joore
MA, Lambin P. Comparison of the effectiveness of radiotherapy with
photons, protons and carbon-ions for non-small cell lung cancer: A metaanalysis.
Radiother Oncol 2010;95:32-40.[LinkOut]
- Nagata Y, Hiraoka M, Mizowaki T, Narita Y, Matsuo Y, Norihisa Y, et al.
Survey of stereotactic body radiation therapy in Japan by the Japan 3-D
conformal external beam radiotherapy group. Int J Radiat Oncol Biol Phys
2009;75:343-7.[LinkOut]
- Palma D, Visser O, Lagerwaard FJ, Belderbos J, Slotman BJ, Senan S. The
impact of introducing stereotactic lung radiotherapy for elderly patients
with Stage I NSCLC: A population-based time-trend analysis. J Clin Oncol
2010;28:5153-9.[LinkOut]
- Pan H, Simpson DR, Mell LK, Mundt AJ, Lawson JD. A survey of
stereotactic body radiotherapy use in the United States. Cancer. 2011 Mar
15. doi: 10.1002/cncr.26067. [Epub ahead of print][LinkOut]
- Palma D, Lagerwaard FJ, Rodrigues G, Haasbeek CJA, Senan S. Curative
treatment of stage I non-small cell lung cancer in patients with severe
COPD: Outcomes after stereotactic radiotherapy and systematic review of
the literature. Int J Radiat Oncol Biol Phys. Forthcoming.
- Louie AV, Rodrigues G, Hannouf M, Lagerwaard FJ, Palma D, Zaric GS, et
al. Withholding Stereotactic Radiotherapy in Elderly Patients with Stage
I Non-small Cell Lung Cancer and Co-existing COPD is not Justified:
Outcomes of a Markov Model Analysis. Radiother Oncol. Forthcoming.
- Hurkmans CW, Cuijpers JP, Lagerwaard FJ, Widder J, van der Heide UA,
Schuring DD, et al. Recommendations for implementing stereotactic
radiotherapy in peripheral stage IA non-small cell lung cancer: Report from
the Quality Assurance Working Party of the randomized phase III ROSEL
study. Radiat Oncol 2009 4:1.[LinkOut]
- Hurkmans CW, van Lieshout M, Schuring D, van Heumen MJT, Cuijpers JP, Lagerwaard FJ, et al. Quality assurance of 4D-CT scan techniques in a multicenter phase III trial of surgery versus stereotactic radiotherapy (ROSEL). Int J Radiat Oncol Biol Phys Oct 13. [Epub ahead of print][LinkOut]
- Chi A, Liao Z, Nguyen NP, Xu J, Stea B, Komaki R. Systemic review of the
patterns of failure following stereotactic body radiation therapy in earlystage
non-small-cell lung cancer: clinical implications. Radiother Oncol
2010;94:1-11.[LinkOut]
- Ong CL, Palma D, Verbakel WFAR, Slotman BJ, Senan S. Treatment of
large stage I-II lung tumors using stereotactic body radiotherapy: Planning
considerations and early toxicity. Radiother Oncol 2010;97:431-6.[LinkOut]
- Lagerwaard FJ, Haasbeek CJA, Smit EF, Slotman BJ, Senan S. Outcomes of risk-adapted fractionated stereotactic radiotherapy for stage I non-small cell lung cancer. Int J Radiat Oncol Biol Phys 2008;70:685-92.[LinkOut]
- Bral S, Van Parijs H, Soete G, Linthout N, Van Moorter L, Verellen D, et al.
A feasibility study of image-guided hypofractionated conformal arc therapy
for inoperable patients with localized non-small cell lung cancer. Radiother Oncol 2007;84:252-6.[LinkOut]
- Bral S, Gevaert T, Linthout N, Versmessen H, Collen C, Engels B, et al. Prospective, risk-adapted strategy of stereotactic body radiotherapy for early-stage non-small-cell lung cancer: Results of a Phase II trial. Int J Radiat Oncol Biol Phys. 2010 Aug 12. [Epub ahead of print][LinkOut]
- Dunlap NE, Larner JM, Read PW, Kozower BD, Lau CL, Sheng K, et al.
Size matters: a comparison of T1 and T2 peripheral non-small-cell lung
cancers treated with stereotactic body radiation therapy (SBRT). J Thorac
Cardiovasc Surg 2010;140:583-9.[LinkOut]
- Onishi H, Shirato H, Nagata Y, Hiraoka M, Fujino M, Gomi K, et al. Hypofractionated stereotactic radiotherapy (HypoFXSRT) for stage I nonsmall cell lung cancer: updated results of 257 patients in a Japanese multiinstitutional study. J Thorac Oncol 2007;2:S94-100.[LinkOut]
- Stephans KL, Djemil T, Tendulkar RD, Robinson CG, Reddy CA, Videtic GM. Prediction of Chest Wall Toxicity From Lung Stereotactic Body Radiotherapy (SBRT). Int J Radiat Oncol Biol Phys 2011 Feb 5. [Epub ahead of print][LinkOut]
- Ong CL, Verbakel WFAR, Cuijpers JP, Slotman BJ, Lagerwaard FJ, Senan
S. Stereotactic radiotherapy for peripheral lung tumors: A comparison
of volumetric modulated arc therapy and 3 other delivery approaches.
Radiother Oncol 2010;97:437-42.[LinkOut]
- Rogers ML, Duffy JP. Surgical aspects of chronic post-thoracotomy pain.
Eur J Cardiothorac Surg 2000;18:711-6.[LinkOut]
- Karmakar MK, Ho AM. Postthoracotomy pain syndrome. Thorac Surg Clin
2004;14:345-52.[LinkOut]
- Sugiura H, Morikawa T, Kaji M, Sasamura Y, Kondo S, Katoh H. Longterm benefits for the quality of life after video-assisted thoracoscopic lobectomy in patients with lung cancer. Surg Laparosc Endosc Percutan Tech 1999;9:403-8.[LinkOut]
- Finlayson E, Fan Z, Birkmeyer JD. Outcomes in octogenarians undergoing
high-risk cancer operation: a national study. J Am Coll Surg 2007;205:729-
34.[LinkOut]
- Sato S, Koike T, Yamato Y, Yoshiya K, Motono N, Takeshige M, et al.
Diagnostic yield of preoperative computed tomography imaging and the
importance of a clinical decision for lung cancer surgery. Gen Thorac
Cardiovasc Surg 2010;58:461-6.[LinkOut]
- Swensen SJ, Silverstein MD, Ilstrup DM, Schleck CD, Edell ES. The
probability of malignancy in solitary pulmonary nodules. Application
to small radiologically indeterminate nodules. Arch Intern Med
1997;157:849-855.[LinkOut]
- Herder GJ, van Tinteren H, Golding RP, Kostense PJ, Comans EF, Smit
EF, et al. Clinical prediction model to characterize pulmonary nodules:
validation and added value of 18F-fluorodeoxyglucose positron emission
tomography. Chest 2005;128:2490-6.[LinkOut]
- Inoue T, Shimizu S, Onimaru R, Takeda A, Onishi H, Nagata Y, et al.
Clinical outcomes of stereotactic body radiotherapy for small lung lesions
clinically diagnosed as primary lung cancer on radiologic examination. Int J
Radiat Oncol Biol Phys 2009;75:683-7.[LinkOut]
- van Tinteren H, Hoekstra OS, Smit EF, van den Bergh JH, Schreurs AJ, Stallaert RA, et al. Effectiveness of positron emission tomography in the preoperative assessment of patients with suspected non-small-cell lung cancer: the PLUS multicentre randomised trial. Lancet 2002;359:1388-93.[LinkOut]
- Herder GJ, Kramer H, Hoekstra OS, Smit EF, Pruim J, van Tinteren H, et
al. Traditional versus up-front [18F] fluorodeoxyglucose-positron emission
tomography staging of non-small-cell lung cancer: a Dutch cooperative
randomized study. J Clin Oncol 2006;24:1800-6.[LinkOut]
- Belgers EH, Siebenga J, Bosch AM, van Haren EH, Bollen EC. Complete
video-assisted thoracoscopic surgery lobectomy and its learning curve. A
single center study introducing the technique in The Netherlands. Interact
Cardiovasc Thorac Surg 2010;10:176-80.[LinkOut]
- Scott WJ, Howington J, Feigenberg S, Movsas B, Pisters K; American
College of Chest Physicians. Treatment of non-small cell lung cancer stage
I and stage II: ACCP evidence-based clinical practice guidelines (2nd
edition). Chest 2007;132:s234-42.[LinkOut]
- Cerfolio RJ, Bryant AS. Survival of patients with true pathologic stage I non-small cell lung cancer. Ann Thorac Surg 2009;88:917-22.[LinkOut]
- May BJ, Levsky JM, Godelman A, Jain VR, Little BP, Mahadevia PS, et al.
Should CT Play a Greater Role in Preventing the Resection of Granulomas
in the Era of PET? AJR Am J Roentgenol 2011;196:795-800.[LinkOut]
- Wouters MW, Siesling S, Jansen-Landheer ML, Elferink MA, Belderbos J, Coebergh JW, et al. Variation in treatment and outcome in patients with non-small cell lung cancer by region, hospital type and volume in the Netherlands. Eur J Surg Oncol 2010;36:s83-92.[LinkOut]
- Haasbeek CJA, Lagerwaard FJ, Antonisse ME, Slotman BJ, Senan S. Stage
I non-small cell lung cancer in patients aged 75 years and older: Outcomes after stereotactic radiotherapy. Cancer 2010;116:406-14.[LinkOut]
- Grills IS, Mangona VS, Welsh R, Chmielewski G, McInerney E, Martin S,
et al. Outcomes after stereotactic lung radiotherapy or wedge resection for
stage I non-small-cell lung cancer. J Clin Oncol 2010;28:928-35.[LinkOut]
- Crabtree TD, Denlinger CE, Meyers BF, El Naqa I, Zoole J, Krupnick AS, et al. Stereotactic body radiation therapy versus surgical resection for stage I non-small cell lung cancer. J Thorac Cardiovasc Surg 2010;140:377-86.[LinkOut]
- Onishi H, Shirato H, Nagata Y, Hiraoka M, Fujino M, Gomi K, et al. Stereotactic body radiotherapy (SBRT) for operable Stage I non-small-cell lung cancer: Can SBRT be comparable to surgery? Int J Radiat Oncol Biol
Phys. 2010 Jul 15. [Epub ahead of print][LinkOut]
- Louie AV, Rodrigues G, Hannouf M, Zaric GS, Palma DA, Cao JQ, et al. Stereotactic body radiotherapy versus surgery for medically operable Stage I non-small-cell lung cancer: A Markov model-based decision analysis. Int J Radiat Oncol Biol Phys. 2010 Oct 5. [Epub ahead of print][LinkOut]
- Lee Y, Auh SL, Wang Y, Burnette B, Wang Y, Meng Y, et al. Therapeutic
effects of ablative radiation on local tumor require CD8+ T cells: changing
strategies for cancer treatment. Blood 2009;114:589-95.[LinkOut]
- Felip E, Rosell R, Maestre JA, Rodríguez-Paniagua JM, Morán T, Astudillo
J, et al. Preoperative chemotherapy plus surgery versus surgery plus
adjuvant chemotherapy versus surgery alone in early-stage non-small-cell
lung cancer. J Clin Oncol 2010;28:3138-45.[LinkOut]
- NSCLC Meta-analyses Collaborative Group, Arriagada R, Auperin A,
Burdett S, Higgins JP, Johnson DH, et al. Adjuvant chemotherapy, with or
without postoperative radiotherapy, in operable non-small-cell lung cancer:
two meta-analyses of individual patient data. Lancet 2010;375:1267-77.[LinkOut]
- Pepe C, Hasan B, Winton TL, Seymour L, Graham B, Livingston RB,
et al. Adjuvant vinorelbine and cisplatin in elderly patients: National
Cancer Institute of Canada and Intergroup Study JBR.10. J Clin Oncol
2007;25:1553-61.[LinkOut]
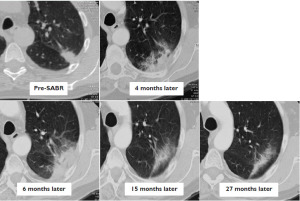
- Dahele M, Palma D, Lagerwaard F, Slotman B, Senan S. Radiological
changes following stereotactic radiotherapy for stage I lung cancer. J Thorac
Oncol. Forthcoming.
- Matsuo Y, Nakamoto Y, Nagata Y, Shibuya K, Takayama K, Norihisa Y, et al. Characterization of FDG-PET images after stereotactic body radiation therapy for lung cancer. Radiother Oncol 2010;97:200-4.[LinkOut]
- Henderson MA, Hoopes DJ, Fletcher JW, Lin PF, Tann M, Yiannoutsos
CT, et al. A pilot trial of serial 18F-fluorodeoxyglucose positron emission
tomography in patients with medically inoperable stage I non-small-cell
lung cancer treated with hypofractionated stereotactic body radiotherapy.
Int J Radiat Oncol Biol Phys 2010;76:789-95.[LinkOut]
- Pasini F, Verlato G, Durante E, de Manzoni G, Valduga F, Accordini S, et al.
Persistent excess mortality from lung cancer in patients with stage I nonsmall-
cell lung cancer, disease-free after 5 years. Br J Cancer 2003;88:1666-
8.[LinkOut]
- Maeda R, Yoshida J, Ishii G, Aokage K, Hishida T, Nishimura M, et al.
Long-term outcome and late recurrence in patients with completely
resected stage IA non-small cell lung cancer. J Thorac Oncol 2010;5:1246-
50.[LinkOut]
- Murthy SC, Reznik SI, Ogwudu UC, Farver CF, Arrossi A, Batizy LH, et al. Winning the battle, losing the war: the noncurative “curative” resection for stage I adenocarcinoma of the lung. Ann Thorac Surg 2010;90:1067-74.[LinkOut]
- Neri S, Takahashi Y, Terashi T, Hamakawa H, Tomii K, Katakami N, et al.
Surgical treatment of local recurrence after stereotactic body radiotherapy
for primary and metastatic lung cancers. J Thorac Oncol 2010;5:2003-7.[LinkOut]
- Chen F, Matsuo Y, Yoshizawa A, Sato T, Sakai H, Bando T, et al. Salvage lung resection for non-small cell lung cancer after stereotactic body radiotherapy in initially operable patients. J Thorac Oncol 2010;5:1999-2002.[LinkOut]
Cite this article as: Senan S, Palma DA, Lagerwaard FJ. Stereotactic ablative radiotherapy for stage I NSCLC: Recent advances and controversies. J Thorac Dis 2011;3(3):189-196. doi: 10.3978/j.issn.2072-1439.2011.05.03
|