Bronchial suction does not facilitate lung collapse when using a double-lumen tube during video-assisted thoracoscopic surgery: a randomized controlled trial
Introduction
Prompt collapse of the lungs is critical for thoracoscopic surgery. Lung collapse consists of two phases: the phase I collapse within approximately the first 1 min of one-lung ventilation (OLV) is due to inherent elastic coil of the lungs and ribcage; then small airway closure, the phase II collapse is due to the uptake of residual lung gases or absorption atelectasis (1).
Nitrous oxide can accelerate phase II collapse, while air may impede it (2). Studies of phase I collapse, such as the disconnection technique (3) and continuous bronchial suction (4), were all performed in the presence of a bronchial blocker. As bronchial suction through the lumen of the bronchial blocker offers an effective means of accelerating lung collapse (4), we hypothesized that bronchial suction could also facilitate lung collapse when using a double-lumen tube (DLT).
Therefore, we carried out a randomized study to examine the effects of bronchial suction on lung collapse in patients intubated with a DLT. Suction was performed at −30 cmH2O during the first minute of OLV. A parallel control arm was left to undergo spontaneous lung collapse.
Methods
The study protocol was approved by the Ethics Committee of Peking Union Medical College Hospital (No. ZS-838) and the authors had followed the applicable Equator guidelines. Written informed consent was obtained from all participants. Clinical trial registration was performed at http://www.chictr.org.cn (identifier: ChiCTR-ICR-15006449) on May 27, 2015. From May 2015 to July 2015, we considered patients for inclusion in our study if they had lung cancer, were scheduled for elective video-assisted thoracoscopic surgery under general anesthesia, underwent OLV using a DLT, had an American Society of Anesthesiologists (ASA) physical status of I–III and were aged 18–75 years. We excluded patients with chronic obstructive pulmonary disease (COPD), pneumothorax, pleural adhesion, early branching of the right upper lobe bronchus (4), anticipated difficult intubation (Mallampatti score ≥3), previous thoracic surgery, or bullae on chest radiographs. Patients were also excluded if their forced expiratory volume in 1 second (FEV1) or forced vital capacity (FVC) were less than 50% of normal values.
Patients were randomly allocated to a bronchial suction or spontaneous lung collapse arm using a computer generated simple randomization sequence by a research associate not involved in subject recruitment and allocation. Concealment was implemented using opaque envelopes that were given to the attending anesthesiologist upon the patient’s arrival in the operating room. The same anesthesiologist provided general anesthesia to all patients. Patients and the operating surgeon, who was the same for all patients, were blinded to group allocation.
Anesthesia was induced with intravenous midazolam 0.03 mg/kg, fentanyl 2 µg/kg, propofol 2 mg/kg and rocuronium 0.9 mg/kg. Anesthesia was maintained with target-controlled infusion (TCI) of propofol at an effect-site concentration (Ce) of 3–4 µg/mL, TCI of remifentanil at a Ce of 3–6 ng/mL and cisatracurium infusion at a rate of 0.1 mg·kg−1·h−1. After tracheal intubation, patients received a mixture of 40% O2 and 60% N2O until the start of OLV (2). Tidal volume was 6–8 mL/kg ideal body weight during mechanical two-lung ventilation (2LV) and OLV without positive end-expiratory pressure (5). Patients were intubated with a DLT of appropriate size (Mallinckrodt™, Covidien LLC, MA, USA) (6). Tube placement was verified by fiberoptic bronchoscopy before and after the patient assumed a lateral decubitus position.
Surgery began when the end tidal N2O Ce reached 55%. At 12 seconds before opening the non-ventilated pleura, inspired gas was switched to 100% O2 at a flow rate of 10 L/min. At 8 seconds before opening the non-ventilated pleura, mechanical 2LV was discontinued with an adjustable pressure limiting (APL) valve at 0 cmH2O. Connection of the DLT to the non-ventilated lung was closed, and the ipsilateral distal port was opened to the atmosphere (7). The suction catheter, supplied with the Mallinckrodt™ DLT package, was placed through the bronchial lumen of the non-ventilated lung in all study subjects. In patients in the bronchial suction group, the gap between the suction catheter and bronchial lumen was closed using an adhesive membrane. The non-ventilated pleura was opened, which was defined as the start of OLV, and suction pressure (−30 cmH2O) was applied for 1 min. In patients in the spontaneous collapse group, the suction device was also used only for making suction noise to keep the surgeon blinded.
After pleurotomy, lungs were visualised using a thoracoscopic camera. The operating surgeon evaluated the degree of lung collapse at 1, 5 and 10 min after the start of OLV using a 10-point visual analogue scale (2). A score of 0 indicates a fully inflated lung; a score of 10 indicates complete lung collapse. The primary endpoint was the degree of lung collapse at 10 min. Secondary outcomes included lung collapse at 1 and 5 min and intraoperative hypoxaemia (defined as a decrease in pulse oxygen saturation to below 90%) at any time during surgery.
After evaluation at 1 min, the suction catheter was withdrawn. After evaluation of lung collapse, the intrathoracic procedure was started and, the fraction of inspired oxygen (FiO2) was decreased from 1.0 to 0.5. If SpO2 at ≤90%, decrease of FiO2 would be discontinued. Data were collected on OLV duration, surgery duration and occurrence of any clinically significant events during surgery, e.g., lung injury, pulmonary oedema, atelectasis (assessed using video-assisted thoracoscopy and reported arbitrarily by the surgeon) and respiratory failure (defined as PaO2 at <60 mmHg or SpO2 at <90%). The same surgeon performed all procedures and evaluations for all subjects in the study.
Statistical analysis
Data were analysed using the SPSS statistical software package (version 20.0; IBM, Chicago, IL, USA). Minimal sample size was determined using power analysis based on the following assumptions: (I) the mean deflation score at 10 min from the start of OLV would be 7.9±1.5 for patients in the spontaneous collapse arm (3); (II) the minimum clinically meaningful difference in lung collapse score between the suction and spontaneous collapse arms was 1.0; (III) α =0.05 and β =0.2. This analysis yielded a minimum of 36 subjects per group. We anticipated a dropout rate of 10% due to, for example, unexpected airway difficulties, and therefore recruited 80 patients into our study. Degree of lung collapse between the two arms was compared using the Mann-Whitney U test; differences in parametric values, using Student’s t-test; and differences in categorical variables, using the χ2 test. A P value <0.05 was considered statistically significant.
Results
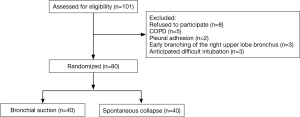
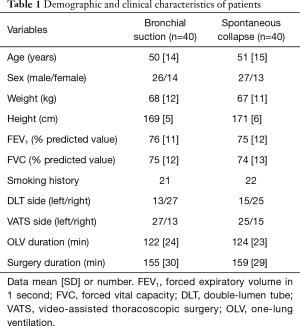
We screened a total of 101 patients for eligibility, of whom 8 refused to participate, 5 were excluded because of COPD, 2 because of pleural adhesion, 3 because intubation was anticipated to be difficult and 3 because of early branching of the right upper lobe bronchus (Figure 1). The remaining 80 subjects were randomized between the bronchial suction and spontaneous collapse arms, which showed generally similar demographic and clinical characteristics (Table 1). Operative complications such as lung injury, pulmonary edema, atelectasis and respiratory failure did not occur in any of the patients.
Full table
The primary endpoint of lung collapse was statistically greater in the bronchial suction group [median (IQR): 9.0 (9.0–9.0)] than in the spontaneous collapse group [8.5 (8.0–9.0); P=0.004, Mann-Whitney U test) (Figure 2). Lung collapse was also statistically greater in the bronchial suction group at 5 min [8.0 (7.0–8.0) vs. 7.0 (6.25–7.0) min; P=0.002] and at 1 min [4.0 (4.0–5.0) vs. 2.0 (2.0–2.0) min; P<0.001) (Figure 2). Intraoperative hypoxaemia did not occur in any patient.

Discussion
The present study showed a statistically greater degree of lung collapse at 10 min in subjects receiving bronchial suction at −30 cmH2O through a DLT during the first minute of OLV than in similarly intubated subjects who were allowed to experience spontaneous collapse. The difference was 0.5 on a 10-point visual analogue scale, which did not meet our predefined minimal difference of 1.0 for clinical significance. The difference did meet this threshold at 1 min, when it was 2.0, as well as at 5 min, when it was 1.0. However, the score at 10 min is more clinically relevant (and was therefore our primary endpoint), since it took approximately 10 min to complete three ports for thoracoscopy. We conclude that bronchial suction does not facilitate lung collapse to a clinically significant extent in patients when using a DLT during video-assisted thoracoscopic surgery. However, greater lung collapse at 1 min could be helpful in reducing accidental injuries, and may be particularly applicable for less-experienced surgeons.
Previous study reported that bronchial suction performed during 93 seconds after start of OLV through a bronchial blocker did shorten the time to complete lung collapse (4). However, they did not observe that this translated to greater degree of collapse overall. The deflation score was similar between the suction and spontaneous collapse arms at 20, 40 and 60 min after the start of OLV.
Our findings of more prominent lung collapse at 1 min than at 5 min after the start of OLV is consistent with the biphasic nature of lung collapse: during the first minute or so, fast collapse occurs, after which small airways close, and a slower second phase occurs as residual lung gases are absorbed (1). Indeed, we planned to perform bronchial suction for only 1 min after the start of OLV in order to coincide with the initial rapid phase of collapse. It may be necessary to optimise the timing of suction for patients with different respiratory conditions, since the timing of small airway closure can be influenced by emphysema, COPD, bronchospasm or pleural adhesions (1). In the current study, fiberoptic bronchoscopy was used to clear bronchus. Whether bronchial suction could facilitate lung collapse in patients with obstructed airways is unknown. Also, lung collapse can be especially challenging in patients with COPD, and using suction might facilitate lung collapse. Further work should verify and extend our results in patients with COPD.
In the current study, lung collapse was evaluated by a single surgeon in all study subjects. This represents a limitation and a potential source of bias in the current study. The results of the current study are relevant to video-assisted thoracoscopic surgery based on current three-port techniques. Whether the results could be extended to surgeries using other techniques and with varying speed of lung collapse, for example, uniport video-assisted thoracoscopic surgery (8), requires further study.
Applying suction catheter for lung collapse may not only have benefits, but can also increase risk for complications, such as a suction catheter included in the staple line during lung resection (9). In our study, the suction catheter was used during only 1 min after pleura opening, then we withdrew the catheter to avoid this complication.
It is unlikely that the failure to detect a clinically meaningful lung collapse at 5- and 10-min using bronchial suction simply reflects inadequate suction pressure. We applied suction of −30 cmH2O through the DLT because this pressure was previously reported to accelerate lung collapse in patients with a bronchial blocker without causing airway complications (4). In contrast, weaker suction of −10 or −20 cmH2O has been reported to be ineffective (10,11), while stronger suction (e.g., −40 cmH2O) may damage airway mucosa and even lead to severe hypoxaemia and pulmonary oedema (12,13). It is possible that the optimal suction pressure depends on the patient’s respiratory condition, comorbidities and complications, which should be investigated in future work. Considering the radius of bronchial blocker is smaller than suction catheter of the DLT (14), it is also unlikely that our failure is due to small lumen of suction catheter.
Conclusions
In conclusion, our results from this randomized controlled trial provide strong evidence that bronchial suction through a DLT may not facilitate lung collapse to a clinically significant extent in patients scheduled for three-port video-assisted thoracoscopic surgery. However, lung collapse at 1 min could help to prevent accidental injuries.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Ethics Committee of Peking Union Medical College Hospital (No. ZS-838) and written informed consent was obtained from all patients.
References
- Pfitzner J, Peacock MJ, Harris RJ. Speed of collapse of the non-ventilated lung during single-lung ventilation for thoracoscopic surgery: the effect of transient increases in pleural pressure on the venting of gas from the non-ventilated lung. Anaesthesia 2001;56:940-6. [Crossref] [PubMed]
- Ko R, McRae K, Darling G, et al. The use of air in the inspired gas mixture during two-lung ventilation delays lung collapse during one-lung ventilation. Anesth Analg 2009;108:1092-6. [Crossref] [PubMed]
- Yoo JY, Kim DH, Choi H, et al. Disconnection technique with a bronchial blocker for improving lung deflation: a comparison with a double-lumen tube and bronchial blocker without disconnection. J Cardiothorac Vasc Anesth 2014;28:904-7. [Crossref] [PubMed]
- El-Tahan MR. A comparison of the disconnection technique with continuous bronchial suction for lung deflation when using the Arndt endobronchial blocker during video-assisted thoracoscopy: A randomised trial. Eur J Anaesthesiol 2015;32:411-7. [Crossref] [PubMed]
- Brassard CL, Lohser J, Donati F, et al. Step-by-step clinical management of one-lung ventilation: continuing professional development. Can J Anaesth 2014;61:1103-21. [Crossref] [PubMed]
- Seo JH, Bae JY, Kim HJ, et al. Misplacement of left-sided double-lumen tubes into the right mainstem bronchus: incidence, risk factors and blind repositioning techniques. BMC Anesthesiol 2015;15:157. [Crossref] [PubMed]
- Pfitzner J. Facilitating lung collapse during one lung ventilation can be rational. Anesth Analg 2014;119:1002-3. [Crossref] [PubMed]
- Reinersman JM, Passera E, Rocco G. Overview of uniportal video-assisted thoracic surgery (VATS): past and present. Ann Cardiothorac Surg 2016;5:112-7. [Crossref] [PubMed]
- Alvarez N, Fernández AB. Analysis of how an aspiration catheter is included in the bronchial suture during lung resection surgery. Arch Bronconeumol 2012;48:342-3. [Crossref] [PubMed]
- Yoshimura T, Ueda K, Kakinuma A, et al. Bronchial blocker lung collapse technique: nitrous oxide for facilitating lung collapse during one-lung ventilation with a bronchial blocker. Anesth Analg 2014;118:666-70. [Crossref] [PubMed]
- Narayanaswamy M, McRae K, Slinger P, et al. Choosing a lung isolation device for thoracic surgery: a randomized trial of three bronchial blockers versus double-lumen tubes. Anesth Analg 2009;108:1097-101. [Crossref] [PubMed]
- Czarnik RE, Stone KS, Everhart CC Jr, et al. Differential effects of continuous versus intermittent suction on tracheal tissue. Heart Lung 1991;20:144-51. [PubMed]
- Baraka A, Nawfal M, Kawkabani N. Severe hypoxemia after suction of the nonventilated lung via the bronchial blocker lumen of the univent tube. J Cardiothorac Vasc Anesth 1996;10:694-5. [Crossref] [PubMed]
- Yoshimura T, Ueda K. In response. Anesth Analg 2014;119:1003. [Crossref] [PubMed]