Isolated unilateral absence of pulmonary artery in adulthood: a clinical analysis of 65 cases from a case series and systematic review
Introduction
Unilateral absence of pulmonary artery (UAPA) is a rare congenital abnormally caused by the failure of the sixth aortic arch to connect with the pulmonary trunk during the embryologic development (1). About 350 cases were reported in the world literature between 1868 and 2010 (2-5). In most patients, UAPA is usually associated with other cardiovascular congenital abnormalities such as tetralogy of Fallot, arterial septal defect, truncus arteriosus (6) and are diagnosed in infancy or childhood due to symptoms related to associated cardiovascular abnormalities. Conversely, approximately 30% of patients with UAPA have no associated cardiovascular anomalies, this is termed isolated UAPA, and such cases generally present with a mild clinical course and can go undiagnosed until adulthood (5,7).
Although two studies have analyzed the clinical characteristics of patients with isolated UAPA (4,8), the median age of the patients was 14 years. Many infants and children were included in these studies. However, it was found that clinical symptoms were age-related in patients with isolated UAPA (8). Since 1990, computed tomography (CT), magnetic resonance imaging and echocardiogram have become the major procedures used to diagnose and evaluate UAPA instead of angiography and cardiac catheterization (4). The chest radiograph of patients with UAPA typically shows a small hemithorax, an ipsilateral absent hilar shadow, the absence of ipsilateral pulmonary artery and ipsilateral hemidiaphragm elevation. When suspicious findings are noted on a chest radiograph, the diagnosis of UAPA can be made definitively by contrast-enhanced CT or magnetic resonance angiography showing the absence of right or left pulmonary artery usually terminate within 2 cm of its expected origin from the main PA and variable systemic collateral arteries (6). Apart from these diagnostic features, lung parenchymal findings, which are thought to be related to profound, long-standing pulmonary hypoperfusion and dynamic changes in the pulmonary blood flow (9) have also been described in literature, including bronchiectasis, cystic space, and interstitial changes such as reticular opacities or honeycombing in the affected lung (7,9,10). The blood supply of the affected lung is derived from the systemic collaterals arising from the bronchial, intercostal, internal thoracic or subdiaphragmatic arteries (4). These submucosal collaterals hypertrophy with time and may rupture, causing massive hemoptysis (11). UAPA treatment depends on the patient’s profile, and can vary from lung revascularization in selected pediatric cases to endovascular embolization when possible in adults, ending with pneumonectomy in patients who are not responsive to the previously administered therapies (12). To date, limited data have been presented regarding clinical characteristics of isolated UAPA in adult patients. Moreover, no reviews of treatment of adult patients with isolated UAPA have yet been published. Therefore, we conducted a study of patients in our hospital and reported in literature to elucidate the frequency of clinical symptoms, lung parenchymal features and collateral circulation, explore the relationship between symptoms and lung parenchymal features, and to summarize therapeutic approaches and outcomes in adult patients with isolated UAPA. Addressing these questions may help clinicians improve the understanding and management of this rare congenital condition in adulthood.
Methods
Search strategy and selection criteria
Identification
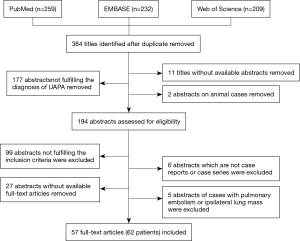
We reviewed the case records of adult patients with isolated UAPA who had been diagnosed at Peking Union Medical College Hospital from 1990. In addition, a search of PubMed, EMBASE, and Web of Science using the key words “unilateral and absence and pulmonary artery” OR “unilateral and pulmonary artery and agenesis” was conducted. Language limits for all searches were set to English and Chinese. Time span for all searches was set from January 1990 to December 2016.The search yielded 259 titles from PubMed, 232 titles from EMBASE, and 209 titles from Web of Science. After remove of duplicates, a total of 384 titles were identified. Ethics approval and consent to participate was waived by the Ethics Committee of Peking Union Medical College Hospital for retrospective analysis of medical records.
Screening
Titles and abstracts were reviewed independently by two authors (Ping Wang and Ling Yuan). All uncertainties were resolved through discussion between two reviewers. Eleven titles without available abstracts for review were excluded. Two abstracts on animal cases were excluded. Cases were considered after they met the minimal requirement of the diagnosis of UAPA based on radiographic confirmation of absent left or right pulmonary artery (LPA or RPA). Thus, 177 abstracts that did not fulfill the diagnosis of UAPA were excluded. Finally, 194 abstracts were assessed for eligibility.
Eligibility
To be considered eligible, the cases required (I) to be older than 14 years, and (II) no accompanying congenital cardiovascular anomalies except for right-sided aortic arch, and (III) no accompanying congenital agenesis of lung or bronchus. Then, 99 abstracts not fulfilling the inclusion criteria were excluded. Next, 6 abstracts which are not case reports or case series were excluded. The number of abstracts was reduced to 89 abstracts. Finally, 27 abstracts without available full-text articles for data extraction were removed. Five abstracts in which isolated UAPA patients with comorbid pulmonary embolism or ipsilateral lung mass were reported were also removed. Thus, 57 full-text articles on a total of 62 patients were included. Figure 1 illustrates the procedure of publication retrieval and the inclusion and exclusion of cases in a flow chart.
Data extraction
The following data were extracted from eligible cases and recorded on a standard data extraction form: age at initial diagnosis, gender, absent side of pulmonary artery and the presence of right-sided aortic arch, symptoms, duration between onset of symptoms and final diagnosis, lung parenchymal abnormalities, hypertrophic collateral arteries, the presence of pulmonary hypertension (PHT) and systolic pulmonary artery pressure, therapeutic strategies and treatment effect on symptoms.
Statistical analysis
All data analyses were carried out with Statistical Package for the Social Sciences, version 17.0 for Windows (SPSS Inc., Chicago, IL, USA). Continuous data were compared using the independent samples t test. Categorical variables were compared using the chi-squared test. A P value of <0.05 was considered statistically significant.
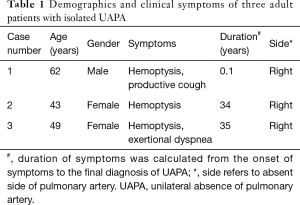
Case series
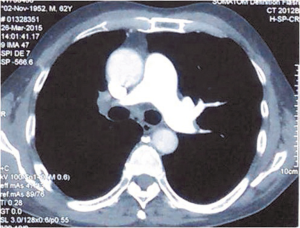
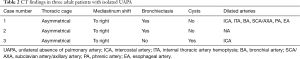
Three adult patients with isolated UAPA were diagnosed at Peking Union Medical College Hospital from 1990. Table 1 lists the age, gender, symptoms, the duration of symptoms from the onset of symptoms to the final diagnosis and absent side of pulmonary artery. Case 1 presented with one episode of massive hemoptysis (about 1,000 mL of fresh blood). Case 2 and case 3 suffered from recurrent hemoptysis. Case 1 was initially misdiagnosed with pulmonary vasculitis and case 2 was misdiagnosed with old tuberculosis. Contrast-enhanced CT was performed in all patients and confirmed the diagnosis of UAPA by showing complete defect of right branch of pulmonary artery, small ipsilateral hemithorax and deviation of mediastinum to the affected side (Figure 2). Table 2 summarized CT findings in all patients. All patients underwent echocardiography, which confirmed no signs of cardiac malformations. Mild pulmonary artery hypertension was demonstrated in case 2 and case 3 with a calculated pulmonary artery pressure of 41 and 45 mmHg respectively. Case 1 underwent embolization of intercostal arteries because of massive hemoptysis. He is relieved of hemoptysis at 21-month follow up. Cases 2 and 3 was observed with close follow up and reported no change of symptoms at 15- and 2-month follow up respectively.
Full table
Full table
Results
We identified a total of 65 adult patients with a diagnosis of isolated UAPA. Three cases were from Peking Union College Hospital and 62 cases were described in 57 articles extracted from PubMed, EMBASE and Web of Science (for detail see Table S1). Table 3 presents the demographic information and clinical symptoms. Median duration between onset of symptoms and final diagnosis was 5 years. In 10 patients with chest pain, 4 patients presented with exercise-induced retrosternal chest pain and 6 patients presented with occasional chest pain. PHT was present in 14 cases (30.4%) of 46 cases with available data of pulmonary artery pressure. The mean pulmonary artery systolic pressure of these patients was 65 (range, 41–85) mmHg. In 13 PHT patients with available data of right-sided heart function, 4 patients (30.8%) present with symptoms and signs of right-sided heart failure and/or showed right-sided heart structural abnormalities and/or dysfunction on echocardiography.

Full table
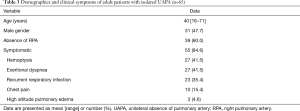
Full table
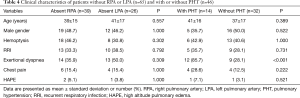
There were no significant differences in age, gender, and prevalence of each symptom between the patients with absent LPA or RPA (Table 4). Exertional dyspnea was more frequent in patients with PHT than in those without PHT (P<0.001; Table 4).
Full table
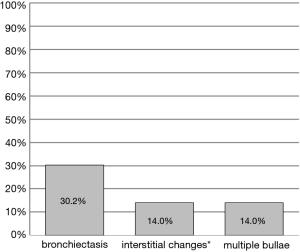
Lung parenchymal manifestation in adult patients with isolated UAPA was described in 43 cases. As shown in Figure 3, from the lung CT scan, bronchiectasis was noted in 13 cases (30.2%), interstitial changes in 6 (14.0%), and multiple bullae in 6 (14.0%). Upon further exploring how the symptoms were related to lung parenchymal abnormalities in adult patients with isolated UAPA, the symptoms of recurrent respiratory infection were found to be more frequent in patients with bronchiectasis than in those without bronchiectasis (P<0.001; Table 5).
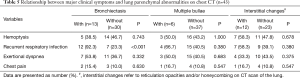
Full table
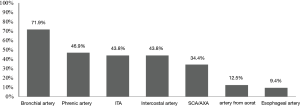
Right-sided aortic arch was found in 12 patients (46.2%) of 26 patients with absent LPA while no patients with absent RPA had a right-sided aortic arch. Variable collateral circulation was shown on contrast-enhanced CT, magnetic resonance angiography, or angiography. In the entire cohort, anomalous coronary collateral circulation was reported in ten cases, four of which presented with exercise-induced retrosternal chest pain. The detail of hypertrophic systemic collateral arteries was available in 32 cases (Figure 4). Bronchial artery was found in 23 cases (71.9%), phrenic artery in 15 cases (46.9%), internal thoracic artery in 14 cases (43.8%), intercostal artery in 14 cases (43.8%), SCA/AXA in 11 cases (34.4%), artery from aorta in 4 cases (12.5%), and esophageal artery in 3 cases (9.4%).
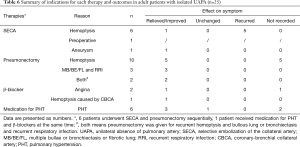
Twenty-five patients received treatment including SECA, right/left pneumonectomy, β-blockers, and anti-PHT medications. Table 6 shows the reasons for using these therapeutic approaches and their effect on patients’ symptoms. Five of six cases (83.3%) in whom SECA was done to treat hemoptysis experienced recurrence of hemoptysis. Of the 12 cases who received pneumonectomy to treat hemoptysis, follow-up data were available for seven and relief of hemoptysis was reported in all seven. Six cases with PHT [mean pulmonary artery systolic pressure, 72.2 (range, 43–85) mmHg] received anti-PHT medication. Three patients who received oral phosphodiesterase inhibitors or endothelin receptor antagonist achieved improvement in exertional dyspnea and/or World Health Organization Functional Class (WHO-FC). However, one case who received oral nifedipine showed no change in symptoms.
Full table
Discussion
We conducted an analysis of 65 adult patients with isolated UAPA to examine their symptomatology, lung parenchymal findings, collateral circulation, therapeutic approaches, and outcomes. Our findings both extend the existing knowledge and provide novel observations regarding the clinical characteristics of isolated UAPA in adulthood.
Almost 85% of adult patients with isolated UAPA in our study were symptomatic, close to 70–87% reported in previous studies (4,13,14). However, the median duration of these symptomatic patients between onset of symptoms and final diagnosis in our study was 5 years. The reason why the diagnoses for these patients were delayed was the nonspecific characteristics of symptoms, failure to recognize this rare congenital disease especially in adult patients, and misdiagnosis of this condition as bronchiectasis, old tuberculosis, chronic pulmonary embolism, pulmonary vasculitis, or Swyer-James-Macleod syndrome (SJMS). SJMS is a rare syndrome of obliterative bronchiolitis following an early childhood infective insult to the lungs which is characterized by a history of pulmonary infection during childhood and persistent cough. High-resolution CT demonstrates unilateral hyperlucent lung with small ipsilateral pulmonary artery with air-trapping on expiration. Diffused decrease in ventilation of affected lung is noted in the lung V/Q scan. Angiography shows smaller pulmonary artery and its branches on the affected side (15).
Our study showed that hemoptysis was the most common symptom in the isolated UAPA patients in adulthood. Conversely, previous studies reported that recurrent respiratory infections and exertional dyspnea are the most common symptoms, while hemoptysis is less frequent, and occurs only in 18–25% of patients with isolated UAPA (4). This discrepancy may be caused by the difference in age of study cohorts. It was shown that collateral vessel formation becomes increasingly common with advancing age (8). Therefore, high clinical suspicion and awareness of isolated UAPA are essential in all adult patients with unexplained hemoptysis.
Our review allowed us to examine how clinical symptoms were related to lung parenchymal features and PHT, in order to explore the possible mechanisms of clinical symptoms. We found that exertional dyspnea was related to the presence of PHT. Several mechanisms have been proposed to explain the dyspnea in UAPA in literature, including cardiac shunting, an increase in resting and/or exercise, physiological dead space, or pulmonary hypertension (16). Our finding confirmed the significance of PHT in explaining exercise limitation in adult patients with isolated UAPA. Recurrent respiratory infection is found to be related to bronchiectasis in the affected lung. However, how absent pulmonary perfusion results in bronchial inflammation and bronchiectasis remains to be understood. Proposed mechanisms include bronchoconstriction secondary to alveolar hypocapnia and impairment of bronchial mucociliary clearance due to impaired delivery of bloodborne inflammatory cells, which in turn leads to mucus trapping, chronic bronchitis, and bronchiectasis (17). In our study, interstitial fibrosing changes such as reticular opacities or honeycombing and multiple bullae were noted in the affected lung in 14% of adult patients with UAPA respectively. A possible explanation for this finding in literature is that hypoperfusion could affect lung parenchymal development and growth and may be responsible for the interstitial fibrosing and cystic changes (10,18).
Excessive collateral circulation results in hemoptysis in patients with UAPA (19). We found that the common collateral arteries in adult patients were the bronchial, phrenic, internal thoracic and intercostal arteries. The overall mortality rate of patients with UAPA has been previously reported to be 7%. Massive hemoptysis can have a devastating effect on long-term survival (4). Therefore, treatment is indicated in symptomatic patients with massive or recurrent hemoptysis (20). In our study, two of five patients who had recurrent hemoptysis after embolization rebleed within a week. The high recurrence rate after SECA may imply that SECA is less successful in controlling hemoptysis in adult patients with isolated UAPA. It was found that in patients who had repeated hemoptysis within a few days after embolization, rebleeding is thought to be due to failure to have all abnormal vessels occluded during embolization (21).
No consensus currently exists on the management of adult patients with isolated UAPA. In our study we encountered various treatment options for adult patients with isolated UAPA including SECA, pneumonectomy, and anti-PHT medication. Pneumonectomy may be helpful in relieving recurrent or massive hemoptysis and refractory respiratory infection in fit patients with isolated UAPA. Early revascularization may allow the affected lung to develop more normally and improve PHT. In older patients, revascularization is not encouraged or even feasible because the intrapulmonary arteries have been found to be severely narrowed or even completely obstructed by fibrosis (6). None of the patients received surgical revascularization for PHT treatment in our study. In adult patients with isolated UAPA who have severe PHT, anti-PHT treatment with oral phosphodiesterase inhibitors or endothelin receptor antagonist was reported to improve dyspnea and the WHO-FC.
There are several limitations to our study. First, we excluded articles that were in languages other than English and Chinese and articles without available full-text version. Therefore, we may have missed some relevant case reports. Second, our study design was a retrospective review of the cases reported in literature. The patients who were investigated tend to be symptomatic patients. Hence a selection bias should be acknowledged in our study. Moreover, not all reports gave sufficient detail regarding the symptoms, image features, collateral circulation, and treatment follow-up data. Third, the mosaic attenuation reported in some case reports was not included in the analysis of lung parenchymal abnormalities on chest CT because mosaic attenuation is difficult to be reliably identified when patients did not receive thin-section lung CT scans.
Conclusions
Clinicians should be aware of undiagnosed cases of isolated UAPA in adults with unexplained hemoptysis. Excessive hypertrophic collateral arteries commonly come from the bronchial artery, phrenic artery, internal thoracic artery, and intercostal artery. Awareness of these systemic collaterals in UAPA patients is important for ensuring the accurate selective embolization of bleeding vessels. Early recognition and management of isolated UAPA in adult patients are crucial to avoid the devastating effect of massive hemoptysis or severe PHT in the long term.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Ethics approval and consent to participate was waived for this study by the Ethics Committee of Peking Union Medical College Hospital.
References
- Pfefferkorn JR, Loser H, Pech G, et al. Absent pulmonary artery: a hint to its embryogenesis. Pediatr Cardiol 1982;3:283-6. [Crossref] [PubMed]
- Pool PE, Vogel JH, Blount SG Jr. Congenital unilateral absence of a pulmonary artery: The importance of flow in pulmonary hypertension. Am J Cardiol 1962;10:706-32. [Crossref] [PubMed]
- Shakibi JG, Rastan H, Nazarian I, et al. Isolated unilateral absence of the pulmonary artery: review of the world literature and guidelines for surgical repair. Jpn Heart J 1978;19:439-51. [Crossref] [PubMed]
- Ten Harkel AD, Blom NA, Ottenkamp J. Isolated unilateral absence of a pulmonary artery: a case report and review of the literature. Chest 2002;122:1471-7. [Crossref] [PubMed]
- Bockeria LA, Makhachev OA, Khiriev T, et al. Congenital isolated unilateral absence of pulmonary artery and variants of collateral blood supply of the ipsilateral lung. Interact Cardiovasc Thorac Surg 2011;12:509-10. [Crossref] [PubMed]
- Kruzliak P, Syamasundar RP, Novak M, et al. Unilateral absence of pulmonary artery: pathophysiology, symptoms, diagnosis and current treatment. Arch Cardiovasc Dis 2013;106:448-54. [Crossref] [PubMed]
- Griffin N, Mansfield L, Redmond KC, et al. Imaging features of isolated unilateral pulmonary artery agenesis presenting in adulthood: a review of four cases. Clin Radiol 2007;62:238-44. [Crossref] [PubMed]
- Koga H, Hidaka T, Miyako K, et al. Age-related clinical characteristics of isolated congenital unilateral absence of a pulmonary artery. Pediatr Cardiol 2010;31:1186-90. [Crossref] [PubMed]
- Sakai S, Murayama S, Soeda H, et al. Unilateral proximal interruption of the pulmonary artery in adults: CT findings in eight patients. J Comput Assist Tomogr 2002;26:777-83. [Crossref] [PubMed]
- Ryu DS, Spirn PW, Trotman-Dickenson B, et al. HRCT findings of proximal interruption of the right pulmonary artery. J Thorac Imaging 2004;19:171-5. [Crossref] [PubMed]
- Britton J, Sachithanandan A, Srinivasan L, et al. Pneumonectomy for congenital isolated unilateral pulmonary artery agenesis. Med J Malaysia 2011;66:363-4. [PubMed]
- Ohtsuka T, Nomori H, Watanabe K, et al. Isolated unilateral absence of a pulmonary artery treated by pneumonectomy in an adult: report of a case. Surg Today 2006;36:525-7. [Crossref] [PubMed]
- Arriero JM, Gil J, Martín C, et al. Unilateral absence of a pulmonary artery: congenital disease or embolic occlusion? Eur Respir J 1991;4:1299-300. [PubMed]
- Bouros D, Pare P, Panagou P, et al. The varied manifestation of pulmonary artery agenesis in adulthood. Chest 1995;108:670-6. [Crossref] [PubMed]
- Mehra S, Basnayake T, Falhammar H, et al. Swyer-James-Macleod syndrome - a rare diagnosis presented through two adult patients. Respirol Case Rep 2017;5:e00245. [Crossref] [PubMed]
- Brassard JM, Johnson JE. Unilateral absence of a pulmonary artery. Data from cardiopulmonary exercise testing. Chest 1993;103:293-5. [Crossref] [PubMed]
- Sherrick DW, Kincaid OW, DuShane JW. Agenesis of a main branch of the pulmonary artery. Am J Roentgenol Radium Ther Nucl Med 1962;87:917-28. [PubMed]
- Roman J, Jones S. Case report: congenital absence of the left pulmonary artery accompanied by ipsilateral emphysema and adenocarcinoma. Am J Med Sci 1995;309:188-90. [Crossref] [PubMed]
- Scheuch RW, Simon-Gabor M, Weinberg HR, et al. Left pulmonary artery agenesis. N Y State J Med 1988;88:200-1. [PubMed]
- Betigeri VM, Betigeri AV, Saichandran BV, et al. Bullous lung disease and bronchiectasis in unilateral absent right pulmonary artery. Gen Thorac Cardiovasc Surg 2013;61:100-3. [Crossref] [PubMed]
- Yu-Tang Goh P, Lin M, Teo N, et al. Embolization for hemoptysis: a six-year review. Cardiovasc Intervent Radiol 2002;25:17-25. [Crossref] [PubMed]
- Taniguchi H, Saito J, Abo H, et al. Isolated Unilateral Absence of the Pulmonary Artery. Am J Respir Crit Care Med 2015;192:518-9. [Crossref] [PubMed]
- Mohan V, Mohan B, Tandon R, et al. Case report of isolated congenital absence of right pulmonary artery with collaterals from coronary circulation. Indian Heart J 2014;66:220-2. [Crossref] [PubMed]
- Pla-Esperanzi A, Pineda-Sanchez V, Roche S. Unilateral pulmonary artery agenesis, angio-MR findings. Rev Esp Cardiol 2013;66:821. [Crossref] [PubMed]
- Mikaberidze N, Goldberg Y, Khosraviani K, et al. Incidentally detected right pulmonary artery agenesis with right coronary artery collateralization. Interact Cardiovasc Thorac Surg 2014;18:139-40. [Crossref] [PubMed]
- Camera L, Fusari M, Calabrese M, et al. Isolated unilateral absence of pulmonary artery mimicking chronic pulmonary embolism at chest X-ray: multidetector-row CT angiographic findings. Clin Imaging 2012;36:845-9. [Crossref] [PubMed]
- Soliman A, Jelani A, Eid A, et al. Myocardial infarction due to coronary steal caused by a congenital unilateral absence of the right pulmonary artery: a rare case. BMJ Case Rep 2012;2012:bcr0420114108. [PubMed]
- Perez-Pampin E, Campos-Franco J, Alegria AM, et al. Isolated unilateral pulmonary artery agenesis. Intern Med 2012;51:233. [Crossref] [PubMed]
- Sanna S, Dell'Amore A, Monteverde M, et al. Unilateral pulmonary artery agenesia complicated by massive haemoptysis in an adult female. Heart Lung Circ 2012;21:166-8. [Crossref] [PubMed]
- De Dominicis F, Leborgne L, Raymond A, et al. Right pulmonary artery agenesis and coronary-to-bronchial artery aneurysm. Interact Cardiovasc Thorac Surg 2011;12:507-9. [Crossref] [PubMed]
- Ito M, Yamashita Y, Harada H, et al. Unilateral absence of the left pulmonary artery accompanied by right lung cancer. Ann Thorac Surg 2010;90:e6-8. [Crossref] [PubMed]
- Ghanbari H, Feldman D, David S, et al. Unilateral absence of a left pulmonary artery: successful therapeutic response to a combination of bosentan and warfarin. Circ Cardiovasc Imaging 2009;2:e46-8. [Crossref] [PubMed]
- de Mello WT Junior, Coutinho Nogueira JR, Santos M, et al. Isolated absence of the right pulmonary artery as a cause of massive hemoptysis. Interact Cardiovasc Thorac Surg 2008;7:1183-5. [Crossref] [PubMed]
- Kadi H, Kurtoglu N, Karadag B. Congenital absence of the right pulmonary artery with coronary collaterals supplying the affected lung: effect on coronary perfusion. Cardiology 2007;108:314-6. [Crossref] [PubMed]
- Jiang Y, Wain JC, Chang AW, et al. Differential changes of alveolar gas concentrations during anesthetic induction of a patient with an absent right pulmonary artery. Anesth Analg 2006;103:312-5. [Crossref] [PubMed]
- Mokta JK, Mahajan SK, Prashar BS, et al. Life threatening unilateral pulmonary oedema at moderate altitude. Indian J Chest Dis Allied Sci 2004;46:113-6. [PubMed]
- Kadir IS, Thekudan J, Dheodar A, et al. Congenital unilateral pulmonary artery agenesis and aspergilloma. Ann Thorac Surg 2002;74:2169-71. [Crossref] [PubMed]
- Nana-Sinkam P, Bost TW, Sippel JM. Unilateral pulmonary edema in a 29-year-old man visiting high altitude. Chest 2002;122:2230-3. [Crossref] [PubMed]
- Farghly E, Bousamra M 2nd. Hemoptysis resulting from unilateral pulmonary artery agenesis. Ann Thorac Surg 2002;74:255-7. [Crossref] [PubMed]
- Mahnken AH, Wildberger JE, Spüntrup E, et al. Unilateral absence of the left pulmonary artery associated with coronary-to-bronchial artery anastomosis. J Thorac Imaging 2000;15:187-90. [Crossref] [PubMed]
- Lin YM, Liang KW, Ting CT. Unilateral pulmonary artery agenesis with presentation of hemoptysis: a case report. Zhonghua Yi Xue Za Zhi (Taipei) 1999;62:644-7. [PubMed]
- Hirata K, Kyushima M, Asato H. Two adult cases of unilateral absence of the right pulmonary artery with markedly different clinical presentations. Jpn Circ J 1995;59:574-8. [Crossref] [PubMed]
- Bekoe S, Pellegrini RV, DiMarco RF Jr, et al. Pneumonectomy for unremitting hemoptysis in unilateral absence of pulmonary artery. Ann Thorac Surg 1993;55:1553-4. [Crossref] [PubMed]
- Debatin JF, Moon RE, Spritzer CE, et al. MRI of absent left pulmonary artery. J Comput Assist Tomogr 1992;16:641-5. [Crossref] [PubMed]
- Sunavala AJ, Thacker HP, Khann JN. Left pulmonary artery hypoplasia presenting with unilateral hyperluscent lung. J Assoc Physicians India 2011;59:179-81. [PubMed]
- Rafiei P, Roda MS, Patel RB. Isolated unilateral absence of the right pulmonary artery. South Med J 2011;104:276-7. [Crossref] [PubMed]
- Ciura VA, Chen F, Sadler DJ, et al. Case of the Month #134. Unilateral absence of a pulmonary artery. Can Assoc Radiol J 2008;59:148-52. [PubMed]
- Komatsu Y, Hanaoka M, Ito M, et al. Unilateral absence of the pulmonary artery incidentally found after an episode of hemoptysis. Intern Med 2007;46:1805-8. [Crossref] [PubMed]
- Gu W, Sun LH, Fang SR, et al. Clinical analysis of the rare causes of hemoptysis: a report of 4 cases. Zhonghua Jie He He Hu Xi Za Zhi 2007;30:343-6. [PubMed]
- Zhang LZ, Ma WG, Gao SG, et al. Unilateral absence of pulmonary artery associated with contralateral lung cancer. J Thorac Dis 2016;8:E942-6. [Crossref] [PubMed]
- Baştuğ S, Aslan AN, Sarı C, et al. Congenital absence of left pulmonary artery with collateralization from all major coronary arteries. Turk Kardiyol Dern Ars 2016;44:240-3. [PubMed]
- Flores M, Letter H, Derrick E, et al. Unilateral absence of the left pulmonary artery with an associated vascular anomaly in adulthood. Cureus 2016;8:e527. [PubMed]
- Emren SV, Tülüce SY, Tülüce K. Isolated congenital unilateral agenesis of the left pulmonary artery with left lung hypoplasia in an asymptomatic adult patient. Acta Cardiol Sin 2015;31:572-5. [PubMed]
- Steiropoulos P, Archontogeorgis K, Tzouvelekis A, et al. Unilateral pulmonary artery agenesis: a case series. Hippokratia 2013;17:73-6. [PubMed]
- Tseng WC, Chen YS, Chiu SN. Coronary artery fistula as major source of right lung circulation in a patient with isolated right pulmonary artery agenesis. Eur Heart J 2010;31:891. [Crossref] [PubMed]
- Mimura S, Kobayashi H, Shinkai M, et al. A case report of congenital isolated absence of the right pulmonary artery: bronchofibrescopic findings and chest radiological tracings over 9 years. Respirology 2005;10:250-3. [Crossref] [PubMed]
- Al Jabbari O, Abu Saleh WK, Ramchandani M, et al. Case Report: Chronic recurrent unilateral pulmonary infection: result of congenital unilateral agenesis of pulmonary artery. Methodist Debakey Cardiovasc J 2016;12:48-50. [Crossref] [PubMed]
- Aiyappan SK, Ranga U, Veeraiyan S. Incidentally detected isolated unilateral pulmonary artery agenesis. J Clin Diagn Res 2013;7:780-1. [PubMed]
- Balcı TA, Koç ZP, Kırkıl G, et al. Isolated left pulmonary artery agenesis: a case report. Mol Imaging Radionucl Ther 2012;21:80-3. [Crossref] [PubMed]
- Smet BS, De Backer A, Cottenie F, et al. Isolated unilateral absence of the right pulmonary artery. JBR-BTR 2012;95:338. [PubMed]
- Reading DW, Oza U. Unilateral absence of a pulmonary artery: a rare disorder with variable presentation. Proc (Bayl Univ Med Cent) 2012;25:115-8. [Crossref] [PubMed]
- Hayek H, Palomino J, Thammasitboon S. Right pulmonary artery agenesis presenting with uncontrolled asthma in an adult: a case report. J Med Case Rep 2011;5:353. [Crossref] [PubMed]
- Muthusami P, Ananthakrishnan R, Elangovan S. Incidentally detected unilateral pulmonary artery agenesis with pulmonary hypoplasia in a 67 year old woman. J Radiol Case Rep 2010;4:32-7. [Crossref] [PubMed]
- Akakabe Y, Kawasaki T, Kuribayashi T, et al. Unilateral absence of pulmonary artery. Clin Cardiol 2009;32:E72. [Crossref] [PubMed]
- Kiss Z, Galuska L, Timár S. Multiplane transesophageal echocardiographic detection and differential diagnosis of isolated right pulmonary artery agenesis. Echocardiography 1996;13:411-4. [Crossref] [PubMed]
- Devulapally KK, Bhatt N, Allen JN. A. 36-year-old woman with a history of dextrocardia and dyspnea. Diagnosis: unilateral absence of a pulmonary artery (UAPA) with right hypoplastic lung. Respiration 2010;79:81-4. [Crossref] [PubMed]
- Sankhla D, Hussein S, George J, et al. Absence of Left Pulmonary Artery: Case report. Sultan Qaboos Univ Med J 2009;9:180-3. [PubMed]
- Takahashi T, Endo H, Ito T, et al. Isolated unilateral absence of the left pulmonary artery: a case report. Ann Vasc Dis 2014;7:178-82. [Crossref] [PubMed]
- Maeda S, Suzuki S, Moriya T, et al. Isolated unilateral absence of a pulmonary artery: influence of systemic circulation on alveolar capillary vessels. Pathol Int 2001;51:649-53. [Crossref] [PubMed]
- Santra A, Padhi R, Dutta P, et al. Left pulmonary artery agenesis with pulmonary hypoplasia in an elderly patient: A rare case report. Bangladesh J Med Sci 2013;12:462-6. [Crossref]
- Basu S, Lapsia S. Something's missing in the chest. Br J Radiol 2010;83:362-3. [Crossref] [PubMed]
- Reddy S, Cao K. Isolated unilateral absence of pulmonary artery: Adult manifestations of a congenital disease. Chest 2016;150:1216A. [Crossref]


