A powered vascular staple for the application of segmental bronchial closure in thoracoscopic anatomic segmentectomy
Introduction
The stapling instruments are indispensable in thoracoscopic surgery, and contributes to curtailment of operating time and the reduction of postoperative prolonged air leak (1). Among complications, bronchopleural fistula (BPF) contributes to the deterioration of quality of life, and the risk to lose patient’s life in worsen case. Several closure methods such as ligation, powered vascular staple (PVS), and clipping, have been described, and little is complicated regarding BPF in thoracoscopic anatomical segmentectomy (TAS) (2).
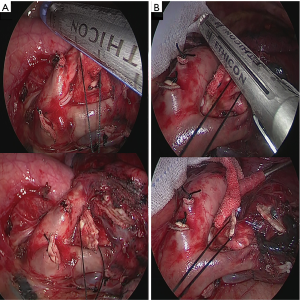
We hypothesized that we might use the PVS in substitution for the powered linier cutter (PLC) for the closure of the segmental bronchi in consideration of passing smoothly and reducing superfluous damage because of the difference in width and configuration of anvil (Figure 1). We use PVS for segmental bronchi which was 10 mm or less in the maximum diameter or lumen 7 mm on computed tomography (CT) after acquisition of informed consent from all eligible patients after ethics committee approval because PVS is mainly warranted to close pulmonary vessels. PVS can be officially available for the subsegmental or segmental bronchi which surgeon can compress by thickness of 1mm in Japan. However, we evade use PVS for segmental bronchi when it is impossible of compression by 1 mm, even if it met our preoperative definition. However, a definitive rule is not regulated in PVS use about the thickness. A novel alternative technique using PVS is suggested to assure its efficacy and feasibility during TAS.
Methods
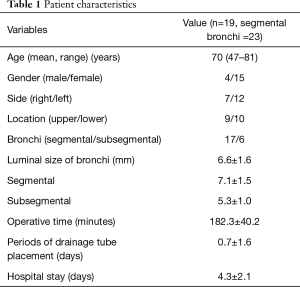
All twenty cases were performed between April 2016 and September 2016 by the same surgeon and thoracic surgery team, and surgical consensus of segmentectomy were prospectively enrolled for non-small cell lung cancer (NSCLC) (n=15, 78.9%) and pulmonary (n=4, 21.1%) metastasis (Table 1). Written informed consent was obtained from the patient for publication of this case series and any accompanying images.
Full table
Patients were scheduled for outpatient control after 2 weeks (X-ray), 1 (X-ray), and 3 months (CT) and follow-up conducted at a median of 72 days (range, 30–165 days). For postoperative air leak, the period after removal of tube drainage was defined as the term “early” when it was performed prior to hospital discharge and as “delayed” when it was performed on outpatient follow-up (3).
Results
The patient characteristics were summarized in Table 1. Nineteen patients underwent TAS. Four (21.1%) were male and 15 (78.9%) were female. The mean ages were approximately 70 years (range, 47–81 years). The mean duration of drainage tube replacement was 0.65±1.6 days (range, 0–7 days).
Total 23 segmental or subsegmental bronchi were transacted by PVS. The mean postoperative resection-planned luminal size was 6.6±1.6 mm (range, 3.7–9.8 mm). Regarding to the location, right upper lobe (n=2, 10.5%), right lower (n=5, 26.3%), left upper (n=7, 36.8%), and left lower (n=5, 26.3%) were carried out. When the responsible bronchi are free from the mediastinal structure, the PVS is applied and fired (Figure 1). Segmental bronchial resection was successful in all cases. No early and delayed air leak including BPF was observed during postoperative follow up observation.
Discussion
This is to our knowledge the first experimental study described in the literature describing intraoperative usage of PVS for the segmental bronchi during TAS. Stapler techniques are the prescribed method of management with both thoracotomy or thoracoscopic approach proving to have similar efficacies for bronchus (4); Oizumi et al. experienced over 297 stumps closure and one BPF was observed at 6 months postoperatively in upper division segmentectomy of the left upper lobe using a stapler (2). While, the mean diameter of the segmental bronchi which we handled using PVS, was 6.6±1.6 mm, and that size was equivalent to their described segmental bronchial diameter (6.6 mm), which they handled using either staple or ligation (2). There are two following ameliorations of PVS: (I) the shortening of width of anvil (18 mm), which is smaller compared with PLC (22 mm), shows easy to pass (Figure 1); and (II) tip is designed to provide an additional 10° of total articulation.
In conclusion, our results suggested that the availability of the PVS represents a novel advance in the armamentarium during TAS and may have a possibility of being pervasive widely however, more observative periods and further sample accumulation are needed. The safe and feasible use of PVS for a small bronchus is not well known. We consider that article announcement will contribute towards to the further development of staple by accumulation of use experience.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images
References
- McKenna RJ Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg 2006;81:421-5; discussion 425-6. [Crossref] [PubMed]
- Oizumi H, Kato H, Endoh M, et al. Management of bronchial stumps in anatomic lung segmentectomy. Ann Thorac Surg 2016;101:2120-4. [Crossref] [PubMed]
- Kuroda H, Dejima H, Mizumo T, et al. A new LigaSure technique for the formation of segmental plane by intravenous indocyanine green fluorescence during thoracoscopic anatomical segmentectomy. J Thorac Dis 2016;8:1210-6. [Crossref] [PubMed]
- Sardelli P, Barrettara B, Cisternino ML, et al. Curved cutter stapler for the application of bronchial sutures in anatomic pulmonary resections: the clinical experience of 139 cases. Eur J Cardiothorac Surg 2012;41:653-6. [Crossref] [PubMed]


