The momentum of HeartMate 3: a novel active magnetically levitated centrifugal left ventricular assist device (LVAD)
Introduction
Cardiovascular diseases are the leading cause of death, resulting in the deaths of about 136 out of every 100,000 people in the United States alone (1,2). Chronic heart failure (CHF) is a type of cardiovascular disease, which results in the diminished performance of either or both ventricles. There are over 5 million cardiac failure patients in the US alone, with several thousands of patients awaiting heart transplantation every year (3). Due to the decline in organ donations and limited availability of healthy donor hearts, the treatment of CHF with mechanical circulatory support (MCS) devices such as left ventricular assist devices (LVADs) is gaining momentum. Several LVADs have been developed over the years involving the implantation of blood pumps to hemodynamically support the left ventricle in patients. Blood pumps can be broadly classified as either pulsatile flow/positive displacement or continuous flow/rotary systems. Continuous flow systems have several advantages over pulsatile flow pumps including more compact size, improved surfaces, as well as reduced surgical trauma and thrombotic complications (4-6). Continuous flow pumps can be further classified into centrifugal and axial flow pumps. Compared to axial pumps actually available, centrifugal flow pumps are smaller and with a tubular configuration, due to which they can be implanted faster and even less invasively, and therefore are probably more cost-effective (7,8). The application of third generation implantable continuous-flow LVADs incorporating improved pump technologies has resulted in improved pump performance and patient healthcare (9). The HeartMate 3 LVAD is a novel centrifugal pump designed by Thoratec Corp., which was acquired by St. Jude Medical Inc. (Pleasanton, CA, USA) and later by Abbott (North Chicago, IL, USA), to supply hemodynamic support in left ventricular heart failure patients, either as a bridge to transplant (BTT), myocardial recovery, or as destination therapy (DT). The worldwide first implantation of the HeartMate 3 was performed by Prof. Schmitto and his team at Hannover Medical School, in Germany on June 25th, 2014 (1). Moreover, due to its considerable miniaturization, minimally invasive surgery for the implantation, explantation as well as exchange of the HeartMate 3 is also achievable (10-17). This article highlights and examines characteristics of the HeartMate 3, such as its unique and innovative pump technology, summarizes clinical studies and outlines future technical developments.
Pump technology
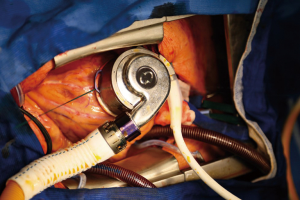
The HeartMate 3 is a novel centrifugal flow pump with a bearingless fully magnetically levitated motor along with active magnetic mounting (18) (Figure 1). The motor technology of this LVAD incorporates a contactless bearing technology and consists of the rotor with passive magnets for drive and bearing, the stator with electromagnetic coils for drive, as well as levitation including hall/distance sensors and microcontroller. The application of rotary blood pumps with magnetically levitated rotors, as opposed to pumps with mechanical bearings (such as in previous versions), improves the feasibility of implanting such LVADs as alternative-to-transplant, applicable for a time span of 10 to 15 years (18). The volume occupied by the HeartMate 3 pump is around one-third of the HeartMate I and less than three times that of the HeartMate II. Similar to the HeartMate II, the HeartMate 3 is capable of pumping up to 10 L/min of blood through the body, which allows patients to engage in multiple stages of physical activity, facilitating weight loss, muscle gain along with an overall improvement in health (9). Compared to previous VAD types, this LVAD is distinguished by features such as its smaller size and pericardial space location. It also does not require the preparation of a pocket space in the chest for implantation. As the device is fully magnetically levitated, the component parts float rather than rub together with wide blood-filled gaps. The presence of a contactless and frictionless rotor makes the device more durable and minimizes shear stress and therefore lowers the risk of post-operative complications. A new feature of this LVAD is its ability to create an ‘artificial pulse’, meaning that the pump speed can periodically increase and decrease, mimicking a pulse rate of 30 beats per minute. The ‘artificial pulse’ ability of the HeartMate 3 distinguishes it from the other FDA-approved LVADs. The pump design is aimed at reducing damage to red blood cells, anticoagulation, thrombus and bleeding. The HeartMate 3 received the approval for the CE mark in 2015 making it one of the latest VADs to receive the CE mark approval.
Clinical studies
The worldwide first implantation of a HeartMate 3 was performed at the Hannover Medical School, Hannover, Germany by a team lead by Prof. JD Schmitto on June 25th, 2014 (1). The HeartMate 3 received CE Mark approval based on data from a clinical trial performed on 50 BTT and destination patients with New York Hospital Association Class IIIb or IV heart failure classification, at 10 centers worldwide (1,15-17,19). A year later the first less-invasive implantation of a HeartMate 3 was mutually performed by surgical colleagues Prof. Ivan Netuka and Prof. Jan D. Schmitto at IKEM Institute in Prague, Czech Republic. The CE Mark trial follow up results of HeartMate 3 implantation showed high patient survival rates of 98%, 92%, 81% and 74% at 1 month, 6 months, 1 year and 2 years post-implantation respectively (1,15-17,19). The trial period showed low post-operative complications such as thrombosis, bleeding, stroke and infection. No pump thrombosis or malfunction was detected during the follow up. Gastrointestinal bleeding was found to be 12% and 20% at 1 and 2 years post-implantation respectively. Total overall stroke rates were 18% and 24% at 1 and 2 years’ time points respectively. VAD implantation associated infection rates were 48% and 52% at 1 year and 2 years post-implantation. Preservation of von Willebrand factor and aortic valve opening have been proposed as mechanisms to alleviate gastrointestinal bleeding (20,21). Stroke events arising from procedural causes may be addressed by improvement of anticoagulation protocols (22). Driveline infections may be treated by timely detection, aggressive surgery, in-patient education and outpatient management (23,24).
The investigational device exemption (IDE) trial (MOMENTUM 3) on HeartMate 3 implantation in 1,028 patients is currently being carried out across 60 centers in the US (25). The trial was set up as a randomized study to compare the performances of HeartMate 3 (centrifugal) and HeartMate II (axial) pumps. Preliminary results showed comparable survival rates in both pump types along with no stroke incidences or pump thromboses as well as reduced pump malfunction.
Most of the results of the MOMENTUM trial are supported by existing literature on the performance of centrifugal pumps with the exception of high incidences of right heart failure in the study (10,12,19). Right heart failure is associated with increased bleeding, mortality and duration of hospital stay. It may be effectively treated by applying less invasive surgical techniques for VAD implantation (26,27).
Minimally invasive techniques are currently being developed for the HeartMate 3 implantation at the Hannover Medical School, Hannover, Germany by a team lead by Prof. Jan D. Schmitto. Such minimized HeartMate 3 implantation involves a surgical approach combining upper hemisternotomy and anterolateral thoracotomy, which may be advantageous due its less invasiveness allowing the reduction of incision necessary for operation.
Conclusions
The HeartMate 3-LVAD is a centrifugal pump with full magnetic levitation, which has been designed to enable optimized hemocompatibility and surgical procedures with reduced incisions. The compactness of the HeartMate 3 components enables efficient device management and improved patient quality of life. This device is well suited for bridge to transplantation and destination therapy patients. HeartMate 3 implantation in humans, involving upper hemi-sternotomy combined with anterior-lateral thoracotomy, was performed for the first time at the Hannover Medical School, Hannover, Germany by a team lead by Prof. Jan D. Schmitto (1). Efforts are ongoing to develop minimally invasive surgical procedures to reduce incision size, blood loss, hospital stays, postoperative pain, complications and need for transfusion products or anticoagulation drugs. Results of the HeartMate 3 implantation as shown by the CE Mark trial have been promising (15,16,19,25). Results of the MOMENTUM trial with a larger patient cohort may provide further evidence of the clinical utility of this pump. Further investigation is necessary to improve pump design in order to improve clinical outcome and reduce adverse surgical complications of VAD implantation.
Acknowledgements
None.
Footnote
Conflicts of Interest: JD Schmitto receives consultation fees from Abbott. The other authors have no conflicts of interest to declare.
References
- Schmitto JD, Hanke JS, Rojas SV, et al. First implantation in man of a new magnetically levitated left ventricular assist device (HeartMate III). J Heart Lung Transplant 2015;34:858-60. [Crossref] [PubMed]
- WHO. NCD mortality and morbidity [Internet]. WHO. [cited 2016 Oct 24]. Available online: http://www.who.int/gho/ncd/mortality_morbidity/en/
- Fang J, Mensah GA, Croft JB, et al. Heart failure-related hospitalization in the U.S., 1979 to 2004. J Am Coll Cardiol 2008;52:428-34. [Crossref] [PubMed]
- Ashton RC, Goldstein DJ, Rose EA, et al. Duration of left ventricular assist device support affects transplant survival. J Heart Lung Transplant 1996;15:1151-7. [PubMed]
- Allen GS, Murray KD, Olsen DB. The importance of pulsatile and nonpulsatile flow in the design of blood pumps. Artif Organs 1997;21:922-8. [Crossref] [PubMed]
- Christensen DM. Physiology of continuous-flow pumps. AACN Adv Crit Care 2012;23:46-54. [Crossref] [PubMed]
- Olsen DB. Rotary blood pumps: a new horizon. Artif Organs 1999;23:695-6. [Crossref] [PubMed]
- Olsen DB. The history of continuous-flow blood pumps. Artif Organs 2000;24:401-4. [Crossref] [PubMed]
- Song X, Throckmorton AL, Untaroiu A, et al. Axial flow blood pumps. ASAIO J 2003;49:355-64. [PubMed]
- Hanke JS, Haverich A, Schmitto JD. Exchange of a HeartWare HVAD to a HeartMate 3 left ventricular assist device. J Heart Lung Transplant 2017;36:480-1. [Crossref] [PubMed]
- Hanke JS, Rojas SV, Dogan G, et al. First series of left ventricular assist device exchanges to HeartMate 3. Eur J Cardiothorac Surg 2017;51:887-92. [Crossref] [PubMed]
- Hanke JS, Dogan G, Rojas SV, et al. First experiences with HeartMate 3 follow-up and adverse events. J Thorac Cardiovasc Surg 2017;154:173-8. [Crossref] [PubMed]
- Schmitto JD, Avsar M, Haverich A. Increase in left ventricular assist device thrombosis. N Engl J Med 2014;370:1463-4. [Crossref] [PubMed]
- Schmitto JD, Rojas SV, Haverich A. Left Ventricular Assist Devices for Advanced Heart Failure. N Engl J Med 2017;376:1894. [PubMed]
- Netuka I, Sood P, Pya Y, et al. Fully Magnetically Levitated Left Ventricular Assist System for Treating Advanced HF: A Multicenter Study. J Am Coll Cardiol 2015;66:2579-89. [Crossref] [PubMed]
- Zimpfer D, Netuka I, Schmitto JD, et al. Multicentre clinical trial experience with the HeartMate 3 left ventricular assist device: 30-day outcomes. Eur J Cardiothorac Surg 2016;50:548-54. [Crossref] [PubMed]
- Krabatsch T, Netuka I, Schmitto JD, et al. Heartmate 3 fully magnetically levitated left ventricular assist device for the treatment of advanced heart failure -1 year results from the Ce mark trial. J Cardiothorac Surg 2017;12:23. [Crossref] [PubMed]
- Loree HM, Bourque K, Gernes DB, et al. The Heartmate III: design and in vivo studies of a maglev centrifugal left ventricular assist device. Artif Organs 2001;25:386-91. [Crossref] [PubMed]
- Schmitto JD, Pya Y, Zimpfer D, et al. HeartMate 3 Fully Magnetically Levitated Left Ventricular Assist Device for the Treatment of Advanced Heart Failure—CE Mark Study 2-Year Results. J Heart Lung Transplant 2017;36:S66. [Crossref]
- Uriel N, Adatya S, Malý J, et al. Clinical hemodynamic evaluation of patients implanted with a fully magnetically levitated left ventricular assist device (HeartMate 3). J Heart Lung Transplant 2017;36:28-35. [Crossref] [PubMed]
- Rao V.. HeartMate 3: Better…but not perfect. J Thorac Cardiovasc Surg 2017;154:179-80. [Crossref] [PubMed]
- Zeitler EP, Eapen ZJ. Anticoagulation in Heart Failure: a Review. J Atr Fibrillation 2015;8:1250. [PubMed]
- Yarboro LT, Bergin JD, Kennedy JLW, et al. Technique for minimizing and treating driveline infections. Ann Cardiothorac Surg 2014;3:557-62. [PubMed]
- Poyanmehr R, Feldmann C, Hanke J, et al. Urgent Driveline Repair Under Catecholamine Support After Total Driveline Cut. Artif Organs 2017;41:686-7. [Crossref] [PubMed]
- Mehra MR, Naka Y, Uriel N, et al. A Fully Magnetically Levitated Circulatory Pump for Advanced Heart Failure. N Engl J Med 2017;376:440-50. [Crossref] [PubMed]
- Hanke JS, Rojas SV, Avsar M, et al. Minimally-invasive LVAD Implantation: State of the Art. Curr Cardiol Rev 2015;11:246-51. [Crossref] [PubMed]
- Schmitto JD, Mokashi SA, Cohn LH. Minimally-invasive valve surgery. J Am Coll Cardiol 2010;56:455-62. [Crossref] [PubMed]


