Off- vs. on-pump coronary artery bypass graft surgery on hospital outcomes in 134,117 octogenarians
Introduction
Enhanced life expectancy has confronted cardiac surgery with a rapidly growing population of octogenarians needing coronary artery bypass grafting (CABG) (1). Octogenarians are deemed a high-risk patient population with increased postoperative morbidity and mortality following conventional CABG using cardiopulmonary bypass (CPB) (COCAB) (2). In such patients reducing invasiveness of the surgical procedure by avoiding CPB may be tried in an attempt to improve outcomes (3). The increasing performance of off-pump coronary artery bypass (OPCAB) grafting within certain centers reflects surgeon preference to avoid the inherent risks of CPB and cardioplegic arrest, including hemodilution, non-pulsatile arterial flow, global myocardial ischemia, atherosclerotic embolization from aortic manipulation, and systemic inflammatory response (4). Although OPCAB grafting is a well-established surgical myocardial revascularization strategy, its actual benefits in terms of morbidity and mortality remain questionable in the general population (5,6). In the higher risk octogenarian patients, however, there is a potential for more tangible clinical benefits when CPB is avoided (7). We aimed to investigate whether OPCAB is associated with better operative outcomes in octogenarians when compared to COCAB by analyzing the Nationwide Inpatient Sample (NIS) databases 2003–2011.
Methods
Data sources
Weill Cornell Medical College determined that institutional review board approval and informed consent was not required because this study uses a de-identified administrative database. This protocol conforms the Helsinki Declaration as revised in 2013. The NIS represents a 20% stratified random sample of all hospital discharges in the US, and collection, validation, and maintenance of the datasets are performed by the Agency for Healthcare Research and Quality. The NIS data use national hospital survey strata to weight each of the participating hospitals. Weights are provided for each discharge record, allowing nationally representative study populations to be produced (8).
The present study included discharge records in NIS datasets from 2003 to 2011 that specifically reported unique hospital identifiers for the study time period with selected International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) procedure and diagnostic codes. Discharge records for patients with CABG procedures were identified using the following ICD-9-CM procedure codes: 30.10, 36.11, 36.12, 36.13, 36.14, 36.15, or 36.16. The concomitant use of CPB support was identified by records that also included the following ICD-9-CM procedure codes for bypass support: 39.61 or 39.66. Discharge records for patients with concomitant cardiac valve procedures (ICD-9-CM codes 35.20, 35.21, 35.22, 35.23, 35.24, 35.25, 35.26, 35.27, 35.28, 35.11, 35.12, 35.13, 35.14) or other cardiotomy (ICD-9-CM code 37.11) for purposes other than CPB were excluded.
Patients aged 80 years or more undergoing isolated first time CABG were stratified by the use of CPB into OPCAB and COCAB. Patient-level and hospital-level variables were used as baseline characteristics. Hospital-level data elements were derived from the AHA Annual Survey Database and ownership/control included urban or rural location, teaching status, and hospital bed size. The Agency for Healthcare Research and Quality’s comorbidity measures based on the Elixhauser method (9) were used to identify comorbid conditions.
Outcomes measured
The primary outcome was in-hospital all-cause mortality for the overall cohort of isolated CABG. Secondary outcome measures were stroke, sepsis, wound infection, tracheostomy, postoperative atrial fibrillation, haemodialysis, length of stay and total costs.
Outcome measures were identified by means of ICD-9 codes (details provided in the Supplementary).
Statistical analysis
Weighted values of patient-level observations were generated to produce a nationally representative estimate of the entire US population of hospitalized patients. Categorical variables were tested using the Pearson’s chi-square test (Rao & Scott adjustment), continuous variables were tested using the Student t-test. P value <0.05 was considered significant. The treatment effect on outcomes of interest was estimated using a hierarchical logistic regression model with the unique hospital identification number used to account for clustering effect and adjusting for both clinical and hospital-level variables. Hierarchical linear regression models were used for continuous dependent variables. As sensitivity analysis, stratification on propensity score was used. First, the propensity score to undergo OPCAB was estimated by logistic regression including patient and hospital-level variables. Patients were stratified into five equal-size groups using quintiles. Mantel-Haenszel pooled parameter estimates are then calculated as weighted means of quantile-specific estimates (10). Finally, a fully adjusted weighted analysis was repeated separately for subjects who received a single graft and patients who received two or more grafts. All analyses were conducted using R [R Core Team (2016), https://www.R-project.org/].
Results
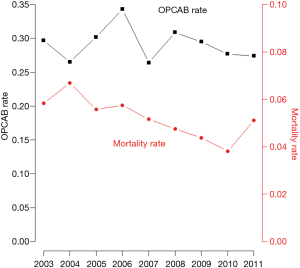
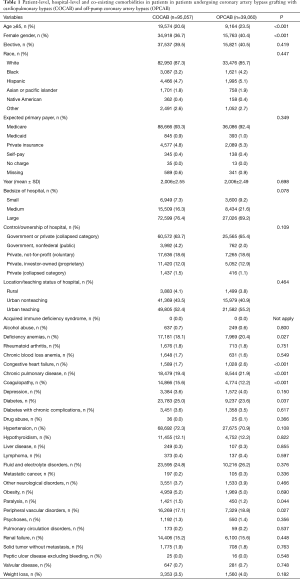
Of the 134,117 discharge records from 797 hospitals analyzed of patients aged ≥80 years undergoing first time isolated CABG from 2003 to 2011, 70.9% (n=95,057) had COCAB and the remaining 29.1% (n=39,060) received OPCAB (Figure 1). Baseline characteristics in the two groups are summarized in Table 1. Patients who underwent OPCAB were more likely to be older than 85 and female. OPCAB patients presented a trend towards a higher prevalence of deficiency anemias, congestive heart failure, chronic pulmonary disease and peripheral vascular disorders. Patients who underwent COCAB presented a trend towards a higher prevalence of diabetes. No significant differences were observed in terms of hospital-level variables.
Full table
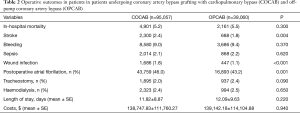
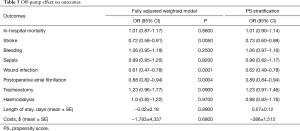
Operative outcomes are summarized in Table 2. COCAB and OPCAB were comparable in terms of operative mortality (5.5% vs. 5.2% respectively, P=0.30). However, the rate of stroke was significantly lower in the OPCAB group (2.4% vs. 1.8% respectively, P=0.004) and this result was confirmed after full adjustment (OR 0.72; 95% CI: 0.58–0.91; P=0.005) and after propensity score stratification (OR 0.73; 95% CI: 0.60–0.89; P=0.005) (Table 3). OPCAB was also associated with a lower risk of wound infection (OR 0.62; 95% CI: 0.49–0.78; P=0.0001) and atrial fibrillation (OR 0.89; 95% CI: 0.84–0.94; P=0.0004). No differences were observed in terms of bleeding, sepsis and need for tracheostomy and haemodialysis. OPCAB was associated with a non-significant marginal trend towards lower costs but did not reduce hospital stay length.
Full table
Full table
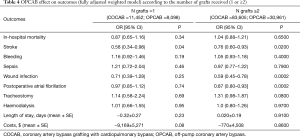
Among subjects who received 1 graft only (n=19,550), 11,452 had COCAB (58.6%) and the remaining 8,098 (41.4%) subjects had OPCAB. Among those who received 2 or more grafts (n=114,566), 83,605 (73.0%) had COCAB and the remaining 30,961 (27.0%) had OPCAB (Table 4). OPCAB was found to be protective in terms of stroke in those who received 1 graft (OR 0.58; 0.34–0.98; P=0.04) and 2 or more grafts (OR 0.76; 0.60–0.93; P=0.02). We also found a marginally non-significant reduction of costs with OPCAB in those who received 1 graft (−9,169$±5,271$; P=0.08) but not 2 or more grafts (−770$±4,508$; P=0.86).
Full table
Discussion
The present analysis of the US Nationwide Inpatient Database is the largest analysis available comparing OPCAB and COCAB in octogenarians. We found that in this high-risk population, OPCAB was associated with a significantly lower incidence of stroke. This benefit was present in both subjects who received 1 graft or 2 and more grafts. OPCAB was also associated with a significantly lower risk of atrial fibrillation and wound infections. However, hospital mortality did not differ between the two strategies as well as the incidence of bleeding, sepsis, haemodialysis and tracheostomy. Length of stay and total costs were not different between the two groups although in subjects who received 1 graft only, we observed a non-significant trend towards a reduction in length of stay and costs with OPCAB.
Despite the potential advantages of avoiding CPB, the perceived benefits of OPCAB in terms of perioperative mortality and morbidity including stroke were not realized in the majority of studies comparing the two strategies (5,6). Short-term mortality and morbidity after off-pump and on-pump CABG were similar in a recent trial (5) involving 4,752 patients with a mixed operative-risk profile [the CABG Off or On Pump Revascularization Study (CORONARY)].
The octogenarians are now the fastest growing population in western countries, and the number of octogenarians with coronary artery disease (CAD) potentially eligible for surgery is expected to increase (2). Octogenarians are a special subset of patients with more comorbidities than their younger counterparts and are particularly vulnerable to organ dysfunction due to the deleterious effects of CPB (1). The German Off-Pump Coronary Artery Bypass Grafting in Elderly Patients (GOPCABE) (6) study focused exclusively on patients 75 years of age or older. COCAB and OPCAB were used in 1,207 and 1,187 subjects, respectively. The two groups were comparable in terms of mortality (2.8% vs. 2.6%; P=0.75) and stroke (2.7% vs. 2.2%; P=0.47). However, the majority of patients enrolled were not octogenarians (mean age 78 years) and the study was largely underpowered to detect significant difference for mortality or stroke. In fact, we estimated that, assuming a 2.5% stroke rate after COCAB in octogenarians and 1% reduction with OPCAB, a sample size of 8,494 will be required to achieve 90% power. A recently published large meta-analysis (11) of 16 retrospective studies including octogenarians only (9,744 COCAB and 8,566 OPCAB patients) showed that early mortality was comparable at 4.6% and 5.2% in the OPCAB and COCAB cohorts, respectively (P=0.60). However, the stroke rate was significantly lower with OPCAB (1.3%) when compared to COCAB (2.4%; P<0.001). Of note, these results are consistent with those observed in the US Nationwide Inpatient Database thus supporting the generalizability of the present findings. Despite multifactorial pathogenesis of cerebral injury and cognitive dysfunction after cardiac surgery, there is increasing evidence that diffuse ischemic cerebral injury is caused by multiple micro-emboli arising from the ascending aorta, the heart chambers, or the bypass circuit (12). Elimination of CPB and adoption of the aortic “no touch” technique, which avoids intraoperative atheromatous embolization from the atherosclerotic aorta into the cerebral circulation, are associated with improved neurologic outcomes (13). Therefore, an argument for preferentially offering OPCAB to octogenarians could be based on the assumption that reduction of stroke may translate into substantial improvement in quality of life and savings in this group of patients with a higher-level of resource utilization (11).
The incidence of post-operative atrial fibrillation was significantly lower in the OPCAB group. Atrial fibrillation is not a life-threatening occurrence, though its presence could predispose to haemodynamic compromise, thromboembolic events, anxiety and increased costs (14). One of the primary reasons why OPCAB may elicit less atrial fibrillation is that it avoids atrial cannulation. Moreover postoperative atrial fibrillation is an independent predictor of postoperative stroke (15) which can account for the lower rate of stroke after OPCAB. We could not find any effect from OPCAB over COCAB in terms of need for dialysis, in accordance with a recent meta-analysis including 33 RCTs with 17,322 patients which showed no significant difference in the need for dialysis in the two groups (16).
Several limitations of the current analysis should be acknowledged. First, the NIS database is assembled from data intended for billing purposes and is thus subject to the appropriate coding of diagnoses and procedures. We do not have granularity to account for pre-hospital CAD management or the varying severity of patient characteristics, such as frailty, precise ejection fraction, pre-operative serum creatinine levels, interval from acute myocardial infarction (in acute myocardial infarction cases), medications, urgency of CABG, hemodynamic data, and severity of CAD. This precludes the ability to calculate Syntax, surgical risk scores, as well as the possibility to compare completeness of revascularization between the two groups, and may have impacted unmeasured confounders that could not be accounted for in our adjustment models. Yet, the large sample size and the 10-year data provide a comprehensive dataset to delineate baseline patient characteristics and trends in risk profile over time.
Despite improvement in patient care management, CABG-related mortality and morbidity in octogenarians remains remarkable. Although the current analysis has failed to prove overwhelming superiority of one technique over the other, OPCAB might represent a valid option to reduce procedure-specific morbidity in this high-risk subgroup in particular in subjects at higher risk of cerebrovascular events.
Supplementary
Outcome measures were identified by the following International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes: stroke (997.02, 362.31, 368.12, 781.4, 433.11, 435, 434), major bleeding (430 to 432, 578.X, 719.1X, 423.0, 599.7, 626.2, 626.6, 626.8, 627.0, 627.1, 786.3, 784.7, and 459.0), wound infection (998.51 and 998.59), sepsis (038, 995.91, 995.92 and 999.3), haemodialysis (V45.1, V45.12, V45.11), tracheostomy (519.00, 519.01, 519.02, 519.09), atrial fibrillation (427.31, 427.3, 427.32).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Weill Cornell Medical College determined that institutional review board approval and informed consent was not required because this study uses a de-identified administrative database.
References
- Fruitman DS, MacDougall CE, Ross DB. Cardiac surgery in octogenarians: can elderly patients benefit? Quality of life after cardiac surgery. Ann Thorac Surg 1999;68:2129-35. [Crossref] [PubMed]
- Alexander KP, Anstrom KJ, Muhlbaier LH, et al. Outcomes of cardiac surgery in patients > or = 80 years: results from the National Cardiovascular Network. J Am Coll Cardiol 2000;35:731-8. [Crossref] [PubMed]
- Boyd WD, Desai ND, Del Rizzo DF, et al. Off-pump surgery decreases postoperative complications and resource utilization in the elderly. Ann Thorac Surg 1999;68:1490-3. [Crossref] [PubMed]
- Trehan N, Mishra M, Sharma OP, et al. Further reduction in stroke after off-pump coronary artery bypass grafting: a 10-year experience. Ann Thorac Surg 2001;72:S1026-32. [Crossref] [PubMed]
- Lamy A, Devereaux PJ, Prabhakaran D, et al. Off-pump or on-pump coronary-artery bypass grafting at 30 days. N Engl J Med 2012;366:1489-97. [Crossref] [PubMed]
- Diegeler A, Börgermann J, Kappert U, et al. Off-pump versus on-pump coronary-artery bypass grafting in elderly patients. N Engl J Med 2013;368:1189-98. [Crossref] [PubMed]
- Pawlaczyk R, Swietlik D, Lango R, et al. Off-pump coronary surgery may reduce stroke, respiratory failure, and mortality in octogenarians. Ann Thorac Surg 2012;94:29-37. [Crossref] [PubMed]
- HCUP Nationwide Inpatient Sample (NIS) Healthcare Cost and Utilization Project (HCUP) Agency for Healthcare Research and Quality, Rockville, MD (May 2015). Available online: www.hcup-us.ahrq.gov/nisoverview.jsp
- Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care 1998;36:8-27. [Crossref] [PubMed]
- Austin PC. An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies. Multivariate Behav Res 2011;46:399-424. [Crossref] [PubMed]
- Altarabsheh SE, Deo SV, Rababa'h AM. Off-pump coronary artery bypass reduces early stroke in octogenarians: a meta-analysis of 18,000 patients. Ann Thorac Surg 2015;99:1568-75. [Crossref] [PubMed]
- Knipp SC, Matatko N, Wilhelm H, et al. Evaluation of brain injury after coronary artery bypass grafting. A prospective study using neuropsychological assessment and diffusion-weighted magnetic resonance imaging. Eur J Cardiothorac Surg 2004;25:791-800. [Crossref] [PubMed]
- Kapetanakis EI, Stamou SC, Dullum MK, et al. The impact of aortic manipulation on neurologic outcomes after coronary artery bypass surgery: a risk-adjusted study. Ann Thorac Surg 2004;78:1564-71. [Crossref] [PubMed]
- Ascione R, Caputo M, Calori G, et al. Predictors of atrial fibrillation after conventional and beating heart coronary surgery. A prospective randomized study. Circulation 2000;102:1530-5. [Crossref] [PubMed]
- Kozora E, Kongs S, Collins JF, et al. Cognitive outcomes after on- versus off-pump coronary artery bypass surgery. Ann Thorac Surg 2010;90:1134-41. [Crossref] [PubMed]
- Cheungpasitporn W, Thongprayoon C, Kittanamongkolchai W, et al. Comparison of Renal Outcomes in Off-Pump Versus On-Pump Coronary Artery Bypass Grafting: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Nephrology (Carlton) 2015. [Epub ahead of print].


