Primary lung carcinoma combined with pulmonary amyloidosis secondary to syphilis infection
Introduction
Amyloidosis is an uncommon disease associated with the deposition of abnormal insoluble proteinaceous amyloid fibrils in the extracellular tissue. It may exist as a primary disease or secondary to a wide variety of chronic conditions such as tuberculosis, chronic renal disease, rheumatoid arthritis and ankylosing spondylitis. Localized pulmonary amyloidosis is rare, while solitary pulmonary nodules mimicking lung cancer are common imaging findings. We describe an unusual case of primary lung carcinoma combined with pulmonary amyloidosis secondary to syphilis infection, where widespread lung cysts are a dominant feature as well as lung nodules.
Case presentation
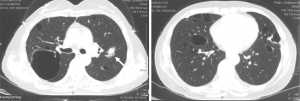
A 55-year-old non-smoking female presented with a pulmonary nodule combined with multiple lung cysts detected on chest CT scan. Chest CT revealed a pulmonary nodule measuring 2.2 cm × 1.5 cm in the lingual segment of the left upper lobe, suggesting a high possibility of malignancy. Multiple bilateral lung cysts of various sizes were also present in the central and subpleural regions. The wall of the cysts showed focal, punctate calcifications, especially apparent in the mediastinal windows (Figure 1). The patient did not have any other significant medical condition.
Laboratory tests showed elevated tumor markers (Table 1). The TP-PA test showed positive and the Venereal Disease Research Laboratory (VDRL) test showed a 1:4 VDRL titer. The brain magnetic resonance and the cerebrospinal fluid tests showed normal. Additional history revealed that the patient was diagnosed with syphilis infection since 1997. Thus, the history and laboratory findings were compatible with tertiary syphilis.
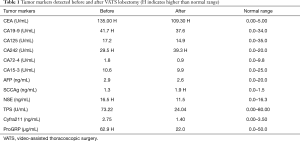
Full table
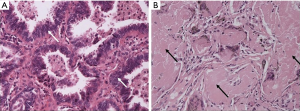
Video-assisted thoracoscopic left upper lobectomy was performed on March 27, 2017. Postoperative pathology confirmed the pulmonary adenocarcinoma (Figure 2A) with bronchopulmonary and mediastinal lymph node metastasis (T1N2M0, IIIa). Interestingly, the subpleural cyst wall showed dense aggregates of acellular, homogeneous, eosinophilic material and multinucleated giant cells. Congo red staining showed salmon pink staining on light microscopy (Figure 2B). Histological findings were consistent with localized nodular pulmonary amyloidosis. All subsequent investigations including serum and urine protein electrophoresis and immunofixation were normal, indicating the diagnosis with secondary pulmonary amyloidosis.
The patient was discharged 4 days after surgery and received routine benzathine penicillin regimen (benzathine penicillin G 240 MU, IM, QW ×3). She received chemotherapy (MP protocol, pemetrexed disodium 500 mg/m2 + cisplatin 75 mg/m2, d1, Q3W ×4) and radiotherapy (3DCRT, 50 Gy/2 Gy/fx) after surgery. No severe adverse effects appeared and no signs of local recurrence or distal disease were found at 3-month and 6-month follow-up visit. However, the multiple bilateral lung cysts remained unchanged on chest CT.
Discussion
Amyloidosis is a heterogenous group of disorders in which insoluble fibrillar proteins are deposited in extracellular tissues. Amyloidosis may present in systemic or localized forms, primary or secondary. Systemic amyloidosis is usually associated with myeloma, tuberculosis, chronic renal disease or rheumatoid arthritis and may affect multiple organs, such as the gastrointestinal system, heart and kidneys. Pulmonary involvement in systemic amyloidosis is not uncommon. However, the respiratory tract (that is, lungs and blood vessels) is commonly affected in localized disease (1). Nodular pulmonary amyloidosis are typically asymptomatic and incidental findings of pulmonary nodules on routine chest radiographs are a common mode of presentation. Because of its nodular appearance, nodular pulmonary amyloidosis is usually misconstrued as neoplasm. On CT, pulmonary nodules have sharp and lobulated margins, and are usually found in a subpleural or peripheral location, more frequently in the lower lobes. Over time, nodules may grow slowly and cavitate, calcify, or resolve spontaneously. Calcification can be seen in 20–50% of nodules on CT images (2). PET/CT with 18F-FDG is used to identify focal areas of increased cellular metabolism. Several case reports mention patients with nodular pulmonary amyloidosis who underwent 18F-FDG PET/CT, most of them showing an increased FDG uptake, but no FDG uptake has also been mentioned (3). For multiple pulmonary nodules, the differential diagnosis should include malignant neoplasm, and histological confirmation is mandatory. In any case a patient with single or multiple nodules highly suggesting malignancy, pathological examination should be performed through biopsy or surgery.
In our patient, we found a pulmonary adenocarcinoma combined with widespread cyst formation in her lungs, which was associated with nodular pulmonary amyloidosis (Figure 2B). The cysts were thin-walled, and there was no cavitation of the visualized pulmonary nodules to suggest that the cysts were secondary to extensive cavitation of nodules. While cavitation of existing pulmonary amyloid nodules is a well-recognized feature of nodular pulmonary amyloidosis, widespread lung cysts located apart from pulmonary nodules is rare, mostly in association immune diseases (4). We report that our patient is the sixth reported case of a lung nodule consisting of adenocarcinoma and amyloid deposition (5,6).
Pulmonary syphilis is rare and there are only 14 cases were reported in the English language literature (7). Radiological presentation included infiltrates and solitary or multiple nodules, sometimes associated with pleural effusion and mimicking malignant lesions (8). Diagnosis of osseous or pulmonary syphilis in reported cases was most often made based on radiological images resolving on penicillin in the context of positive serology. Considering VDRL positive and past history, we proposed the diagnosis of nodular pulmonary amyloidosis secondary to syphilis infection. However, after anti-syphilis treatment, the multiple lung cysts showed no remission at the 3-month follow-up, indicating the amyloidosis a chronic course which needs a long-time follow up. We believe this is the first case report of localized pulmonary amyloidosis secondary to syphilis infection.
Our case highlights a rare manifestation showing that localized pulmonary amyloidosis may be caused by syphilis infection. Widespread lung cysts located apart from pulmonary nodules may be a rare manifestation of pulmonary amyloidosis. It is difficult to differ malignant nodules from nodular pulmonary amyloidosis. CT, PET/CT, tumor marker may help but pathological examination should be proposed when necessary.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Khoor A, Colby TV. Amyloidosis of the Lung. Arch Pathol Lab Med 2017;141:247-54. [Crossref] [PubMed]
- Czeyda-Pommersheim F, Hwang M, Chen SS, et al. Amyloidosis: Modern Cross-sectional Imaging. Radiographics 2015;35:1381-92. [Crossref] [PubMed]
- Barešić M, Sreter KB, Brčić L, et al. Solitary pulmonary amyloidoma mimicking lung cancer on 18F-FDG PET-CT scan in systemic lupus erythematosus patient. Lupus 2015;24:1546-51. [Crossref] [PubMed]
- Sakai M, Yamaoka M, Kawaguchi M, et al. Multiple cystic pulmonary amyloidosis. Ann Thorac Surg 2011;92:e109. [Crossref] [PubMed]
- Miyazaki D, Yazaki M, Ishii W, et al. A rare lung nodule consisting of adenocarcinoma and amyloid deposition in a patient with primary systemic AL amyloidosis. Intern Med 2011;50:243-6. [Crossref] [PubMed]
- Okamoto S, Togo S, Nagata I, et al. Lung adenocarcinoma expressing receptor for advanced glycation end-products with primary systemic AL amyloidosis: a case report and literature review. BMC Cancer 2017;17:22. [Crossref] [PubMed]
- Riganti J, Martin M, Torre AC, et al. Secondary syphilis with pulmonary involvement. J Eur Acad Dermatol Venereol 2016;30:e177-9. [Crossref] [PubMed]
- Crouzy F, Alvarez V, Gex G, et al. Unusual presentations and pitfalls of secondary syphilis: osteitis, pneumonia and malignancy. BMJ Case Rep 2015;2015:bcr2015210618. [Crossref] [PubMed]


