Thoracoscopic purse string technique for minimally invasive Ivor Lewis esophagectomy
Introduction
Surgery is the main treatment for resectable esophageal cancer; however, the mortality of open esophagectomy is high and consequently minimally invasive esophagectomy (MIE) was developed (1). MIE was initially developed by Cuschieri et al. (2) and DePaula et al. (3). Various technical modifications has been made to this technique, including laparoscopic assisted and thoracoscopic assisted techniques. Combined thoracoscopic laparoscopic esophagectomy with cervical anastomosis (TLE-neck) and intrathoracic anastomosis (TLE-chest) have gradually become the mainstream MIE techniques. The first randomized controlled study in the world showed significant advantages of MIE over traditional open surgery (4). TLE-chest is increasingly used for the treatment of mid and lower esophageal cancers. Studies (5-7) have shown that this technique is safe and effective, particularly in reducing perioperative complications such as recurrent laryngeal nerve injury, lung infection, and anastomosis fistula (6). Previously we described our MIE technique with Ivor-Lewis anastomosis. Here we present in the video our TLE-chest operation procedures (Video 1).
Operative techniques
Abdominal part of the operation
Five ports are made. A forcep is placed through the 5 mm trocar below the xyphoid process to grasp the gastrohepatic ligament for liver retraction.
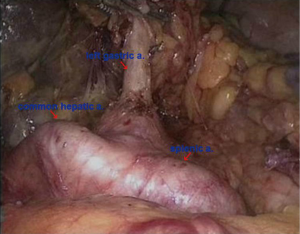
Stomach mobilization and lymph nodes dissection
After laparoscopic abdominal exploration, the gastric body is mobilized using a Harmonic scalpel. The mobilization is started at the lesser curvature. The three branches of the celiac trunk are “skeletonized” and surrounding lymph nodes are dissected (Figure 1). The gastrosplenic ligament is carefully transected. The dissection at the greater curvature side shall be made downwards to sufficiently separate the adhesions at the pylorus. The dissection is made upwards to expose both crus. Left and right cardia lymph nodes are dissected. Definitive attention shall be made to avoid gastric serosa injury, and to protect the integrity of right gastroepiploic vascular arch.
Gastric conduit preparation and staple line embedding
Vessels at the lesser curvature and 3-5 cm proximal to the pylorus are managed. Most of the gastric conduit is made using 3-4 firings of Echelon 60 stapler (Ethicon Endo-Surgery, Cincinnati, Ohio, USA). The staple line of the gastric conduit is embedded with gastric muscular and serosa layers using absorbable suture (4-0 Braided Absorbable Suture, Covidien, USA).
Jejunostomy
Jejunostomy is made laparoscopically at 20 cm distal to the Treitz ligament, and a feeding tube (Flocare CH08 jejunostomy feeding tube, Nutracia) is placed.
Thoracic part of the procedure
The patient is turned to left semi-prone position. Single lung ventilation is established. The thoracic procedure is operated using four ports.
Esophagus mobilization
Following thoracic exploration, the esophageal bed and mediastinal pleura are opened, and the esophagus is lifted. The azygos vein is divided after Hem-O-Lok double clipping at the proximal and distal sides. The esophagus is mobilized upwards until 2 cm above the azygos vein arch. Attention should be given to preserve the mediastinal pleura above the azygos vein arch.
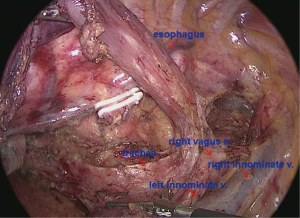
Lymph nodes dissection
The lymph nodes of inferior pulmonary ligament and of the starting point of the left recurrent laryngeal nerve, and paraesophageal and subcarinal lymph nodes are dissected (Figure 2). Exploration is made along the anatomical location of the right recurrent laryngeal nerve chain and the lymph nodes are dissected. Neither recurrent laryngeal nerve is skeletonized during their lymph nodes dissection.
Thoracoscopic purse string
The 5 mm trocar in the 3/4 intercostal space on the posterior axillary line is extended to 3-4 cm, and a wound protector is placed. The gastric conduit is lifted to the thoracic cavity. A purse string is made using 3-0 Prolene 5-8 cm proximal to the tumor. An incision is made 2-3 cm distal to the purse string. An anvil is placed into the esophagus and the purse string is tightened and tied.
En bloc tumor resection
The esophagus is transected layer by layer. The esophagus and the stomach are pulled out of the chest cavity. The mid and lower esophagus with the tumor, cardia and lesser curvature lymph nodes are resected en bloc.
Gastroesophageal anastomosis
The incision of the gastric conduit is lifted using the triangle-shaped sutures and the body of the circular stapler (CDH stapler, Ethicon Endo-Surgery, USA). The anvil is connected to the stapler and an end-to-side gastroesophageal anastomosis is completed in the right thoracic cavity. The remaining gastric conduit is completed using Echelon 60, and the staple line is embedded.
Embedding of the anastomosis
The anastomosis is embedded with mediastinal pleura that has been preserved for this purpose.
Discussion
TLE-chest provides an effective technique for the treatment of mid and lower esophageal cancers; however, thoracoscopic gastrointestinal tract reconstruction remains challenging. Although devices such as OrVil (8,9) and Endo-Stich (6,10) are available, these devices are quite expensive. We previously reported a novel purse string technique for the first time in the world (11). We have been applying this technique to the TLE-chest of 80 consecutive cases since October 2011, and the perioperative results have been satisfactory.
This technique presents the following features: (I) the purse string is made thoracoscopically using an atraumatic suture and the process is convenient, fast and cost effective; (II) the transection of the esophagus is made layer by layer; the muscular layer is divided first, followed by the division of the mucosal layer. More importantly, the mucosal layer is retained 5 mm longer than the muscular layer to prevent mucosa retraction; (III) the tumor is resected en bloc, which is consistent with the oncology principle and it facilitates intrathoracic anastomosis; (IV) the anastomosis is made with a regular circular stapler, which is cost effective for wider application; (V) mediastinal pleura is preserved for the embedding of the anastomosis to enhance the safety of the anastomosis.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med 2002;346:1128-37. [PubMed]
- Cuschieri A, Shimi S, Banting S. Endoscopic oesophagectomy through a right thoracoscopic approach. J R Coll Surg Edinb 1992;37:7-11. [PubMed]
- DePaula AL, Hashiba K, Ferreira EA, et al. Laparoscopic transhiatal esophagectomy with esophagogastroplasty. Surg Laparosc Endosc 1995;5:1-5. [PubMed]
- Biere SS, van Berge Henegouwen MI, Maas KW, et al. Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Lancet 2012;379:1887-92. [PubMed]
- Nguyen NT, Follette DM, Lemoine PH, et al. Minimally invasive Ivor Lewis esophagectomy. Ann Thorac Surg 2001;72:593-6. [PubMed]
- Bizekis C, Kent MS, Luketich JD, et al. Initial experience with minimally invasive Ivor Lewis esophagectomy. Ann Thorac Surg 2006;82:402-6; discussion 406-7. [PubMed]
- Luketich JD, Pennathur A, Awais O, et al. Outcomes after minimally invasive esophagectomy: review of over 1000 patients. Ann Surg 2012;256:95-103. [PubMed]
- Nguyen TN, Hinojosa MW, Smith BR, et al. Thoracoscopic construction of an intrathoracic esophagogastric anastomosis using a circular stapler: transoral placement of the anvil. Ann Thorac Surg 2008;86:989-92. [PubMed]
- Campos GM, Jablons D, Brown LM, et al. A safe and reproducible anastomotic technique for minimally invasive Ivor Lewis oesophagectomy: the circular-stapled anastomosis with the trans-oral anvil. Eur J Cardiothorac Surg 2010;37:1421-6. [PubMed]
- Misawa K, Hachisuka T, Kuno Y, et al. New procedure for purse-string suture in thoracoscopic esophagectomy with intrathoracic anastomosis. Surg Endosc 2005;19:40-2. [PubMed]
- Zhang RQ, Xia WL, Kang NN, et al. Pursestring stapled anastomotic technique for minimally invasive Ivor Lewis esophagectomy. Ann Thorac Surg 2012;94:2133-5. [PubMed]