Climbing the hill of left main coronary artery revascularization: percutaneous coronary intervention or coronary artery bypass graft?
Unprotected left main coronary artery (ULMCA) disease can be found in 3–10% of patients undergoing coronary angiography and has an impact on prognosis (1). Surgical myocardial revascularization by means of coronary artery bypass graft (CABG) has traditionally represented the standard therapeutic procedure for ULMCA disease (2) mainly because up to 80% of left main (LM) lesions involve the bifurcation and up to 80% of patients with ULMCA disease also have multivessel coronary artery disease. In the last few years, percutaneous coronary intervention (PCI) with stent implantation has been challenging CABG. The continuous technical improvement of coronary stents allows the progressive extension of percutaneous treatment to more extensive coronary disease and more complex patients (3). In particular, the recent publication of the results of the NOBLE and EXCEL trials, reporting the results for PCI of ULMCA disease, shed new light on the everlasting confrontation between PCI and CABG (4,5).
In the LM-subset analysis of the pivotal Synergy between PCI with Taxus and Cardiac Surgery (SYNTAX) trial no difference in major adverse cardiac and cerebrovascular events (MACCE) between PCI- and CABG-treated was found. There was a lower stroke rate but a larger proportion of patients undergoing repeat revascularization in the PCI arm compared with CABG (6). In fact, the 5-year MACCE rate was 36.9% for PCI patients versus 31.0% for CABG patients [HR =1.23 (95% CI, 0.95–1.59)], while the stroke rate was significantly higher in the CABG group [4.3% vs. 1.5% in PCI patients; HR =0.33 (95% CI, 0.12–0.92)]. On the contrary, repeat revascularization was lower in the CABG arm [15.5% vs. 26.7%; HR =1.82 (95% CI, 1.28–2.57)]. MACCE rates were similar between the treatment arms in patients with a low to intermediate SYNTAX score, while it raised significantly in patients with a higher SYNTAX score (≥33) (7).
The Pre-COMBACT trial also randomized patients with ULMCA stenoses to either CABG (n=300) or PCI with a first generation sirolimus-eluting stents (n=300). In this randomized trial, PCI was non-inferior to CABG, in terms of MACCE (8).
In the recently published NOBLE trial, however, 1,201 patients were treated with PCI with biolimus-eluting stent (n=598) or CABG (n=603), despite 592 had been randomly assigned to each arm (5). In this trial CABG performed significantly better than PCI, as the limit for non-inferiority was crossed (P=0.0066) (5). Similarly, all-cause mortality rates were 12% for PCI versus 9% for CABG (P=0.77) (5). CABG showed a better performance for myocardial infarction not related to the procedure (7% vs. 2%; P=0.0040), or any revascularization (16% vs. 10%; P=0.032) (5), suggesting that CABG might be a better option for the treatment of ULMCA disease (5).
However, in the recent EXCEL trial the primary endpoint of MACCE was 15.4% for PCI versus and 14.7% for CABG in patients with ULMCA disease and low to intermediate SYNTAX score (4). Hence the authors concluded that PCI is non-inferior to CABG for the treatment of ULMCA bifurcation lesions when the syntax scores is below 32 (4). It should be pointed out that the low mortality registered at 30 days in the CABG arm (1%) was probably related to high quality of the surgical centers involved in the study as well as to the frequent use of off-pump surgery, arterial revascularization, and guidance by transesophageal ultrasonography (4).
More recently, a sub-analysis was performed alongside the EXCEL trial to assess the impact on quality of life (QoL) in patients with ULMCA disease (9). Over 36 months, both PCI and CABG were associated with significant improvements in QoL compared with baseline. However, at 1 month, PCI was associated with better QoL than CABG, while these differences were largely attenuated by 12 months and virtually absent by 36 months (9). These data could additionally influence the decision to select a percutaneous or surgical revascularization. Nevertheless, as the results of the EXCEL study confirm, a Heart Team approach is of paramount importance to achieve complete myocardial revascularization (4). In fact, routine patients’ evaluation by the heart team in the EXCEL study was associated to excellent results, both in the Stent-PCI and in the CABG arms (4).
In light of the different results of the most recent trials, the updated meta-analysis by Mahmoud and colleagues on randomized trials comparing PCI with CABG in patients with ULMCA disease, published in the current issue of Catheterization and Cardiovascular Interventions, comes up timely (10). In this comprehensive meta-analysis of six randomized trials, including 4,700 patients with ULMCA disease with a low to intermediate SYNTAX score (mean of 23±3), the authors compared the outcomes of PCI versus CABG (10). At the short-term follow-up of 30-day, PCI was associated with a lower risk of MACCE, driven by a lower risk of MI and stroke. At 1 year, the risk of MACCE was similar, while CABG was associated with a lower risk of the composite of MACCE at the long-term follow-up (weighted mean follow-up of 5-year), mainly driven by a lower rate of ischemia-driven revascularization (10). All-cause mortality, MI, and stroke were similar in both groups (10). However, some issues about this analysis are worth mentioning. First, the inclusion of selected populations in the single studies, together with specific treatment protocols and outcomes definitions might have influenced results. This could also partly explain some of the different results between the studies. For instance in the NOBLE trial (5), the endpoint of death, stroke and myocardial infarction was driven by a higher rate of myocardial infarction and stroke in the PCI arm, which could have been related to the specific characteristics of the NOBLE study. In fact, an excess of stroke was registered in this latter trial at 1 year just after dual antiplatelet therapy (DAPT) interruption, while DAPT was still ongoing at the 2-year follow up in 70% of patients enrolled in the EXCEL trial (4,5). In addition, the use of biodegradable-polymer biolimus drug-eluting stents was also a peculiar characteristic of this study (5). In addition, the trials included in the meta-analysis by Mahmoud and colleagues, were conducted in highly specialized centers by experienced operators, hence, the findings of this study should not be easily generalizable.
The most recent guidelines for myocardial revascularization issued by the European Society of Cardiology endorse PCI (class I) for the treatment of ULMCA stenoses in patients with a SYNTAX score (SS) <22, reserving a weaker recommendation (class IIa) for patients with a SS between 23 and 32 (11). On one hand, these recommendations reflect the sum of current clinical evidence. In fact, in our recent meta-analysis comparing PCI vs. CABG for the treatment of ULMCA disease, CABG was associated with a better outcome, in terms of the composite endpoint of death, MI, stroke or repeat revascularization on the long-term (>24 months) only in the subgroup of patients with a Syntax score over 33. We should notice that this difference was mainly driven by an excess of repeat revascularization rate in patients who had been randomized to PCI (12). To this regard, it should be noticed that the 10-year follow up of the LE MANS study revealed a late catch-up, with repeat revascularizations occurring later but almost reaching up in prevalence with PCI (13). On the other hand, risk stratification on the basis of the Syntax score alone has several limitations. Our recent meta-analysis suggested additional benefit from the use of clinical variables to select the best revascularization strategy. In fact, diabetes was associated with a better performance of CABG over PCI on the long-term clinical success at meta-regression (12). In line with this concept, it was demonstrated that addition of clinical parameters to the mere anatomical evaluation makes risk stratification more effective (14).
Altogether, a number of elements should be taken into account beyond the results of clinical trials, to select the better strategy for individual patients (Table 1). The better peri-procedural safety profile, the shorter hospitalization, as well as an improved cost-effectiveness make PCI attractive. In contrast, the hospitalization length, need for transfusions, and risk of infection are higher for the CABG compared with PCI. Nevertheless, CABG seems to perform better in specific patients’ categories, such as complex anatomical settings or females. On the contrary, PCI performs better in older patients and less diffuse coronary disease (12).
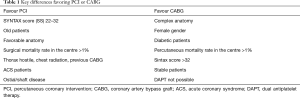
Full table
Further key elements in the decision-making process for treating ULMCA disease that are missing in the article by Mahmoud and colleagues but are well worth a mention are: (I) the known difference in terms of technical execution and clinical outcome for PCI between stenting of the LM ostium or trunk and the treatment of bifurcation or trifurcation lesions, that are associated with a higher rate of restenosis, while lesion location has no relevant influence on long-term results of CABG; (II) the angiographic definition of “significant” ULMCA disease remains challenging, whereas intracoronary evaluation techniques such as intracoronary imaging (IVUS/OCT) or iFR/FFR might be very helpful in this setting (15-18); (III) PCI techniques to treat the stenosis of ULMCA are different and quite heterogeneous, and we know that implantation techniques have a significant impact on clinical results for PCI of a ULMCA (18); (IV) in our recent meta-regression analysis, older patients did better with PCI than CABG (12).
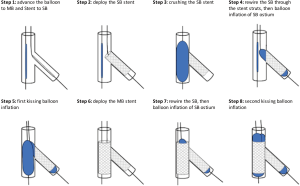
A limitation of the meta-analysis by Mahmoud and colleagues (10), as it is often the case with meta-analyses, is the lack of stratification on the basis of the different PCI techniques used. In fact, provisional stenting (PS) is the most common technique used to treat distal LM bifurcation lesions in patients with ULMCA disease undergoing PCI (19). However, the Double Kissing Crush versus PS for LM Distal Bifurcation Lesions (DKCRUSH-V) that compared two different techniques for PCI of true distal LM bifurcation lesions, demonstrated that a planned DK crush 2-stent strategy resulted in a lower rate of (target lesion failure) TLF at 1 year than a PS strategy (5% vs. 10.7%, P<0.02) (20) (Figure 1). In addition, DK crush also resulted in lower rates of target vessel myocardial infarction (2.9% vs. 0.4%; P=0.03) and definite or probable stent thrombosis (3.3% vs. 0.4%; P=0.02), compared with PS. This study doesn’t apply to LM lesions with less than 50% diameter stenosis of the side branch. In this latter case, the provisional stent remains the standard of care. The DKCRUSH III trial demonstrated that the routine 2-stent DK crush technique is superior to culotte stenting for LM CAD (21). These results could suggest that the prevalent use of culotte stenting in the NOBLE trial could have contributed to the worse performance of PCI (5).
In conclusion, the study of Mahmoud and colleagues (10) demonstrated that ULMCA disease with low/intermediate syntax score can be safely treated equally well with PCI or CABG. However, the selection of the technique which should be adopted in the individual patient with ULMCA disease requires training, experience, and attention to procedural details. When PCI is used to treat ULMCA disease, intravascular ultrasound guidance should be used, as it was associated with better outcomes (22).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Puricel S, Adorjan P, Oberhänsli M, et al. Clinical outcomes after PCI for acute coronary syndrome in unprotected left main coronary artery disease: insights from the Swiss Acute Left Main Coronary Vessel Percutaneous Management (SALVage) study. EuroIntervention 2011;7:697-704. [Crossref] [PubMed]
- Cavalcante R, Sotomi Y, Lee CW, et al. Outcomes After Percutaneous Coronary Intervention or Bypass Surgery in Patients With Unprotected Left Main Disease. J Am Coll Cardiol 2016;68:999-1009. [Crossref] [PubMed]
- Schwietz T, Ehrlich JR, De Rosa S, et al. Prognostic impact of using drug-eluting-stents on outcome and strategy in multivessel PCI: data from the Frankfurt MV-PCI registry. J Cardiol 2013;61:38-43. [Crossref] [PubMed]
- Stone GW, Sabik JF, Serruys PW, et al. Everolimus-Eluting Stents or Bypass Surgery for Left Main Coronary Artery Disease. N Engl J Med 2016;375:2223-35. [Crossref] [PubMed]
- Mäkikallio T, Holm NR, Lindsay M, et al. Percutaneous coronary angioplasty versus coronary artery bypass grafting in treatment of unprotected left main stenosis (NOBLE): a prospective, randomised, open-label, non-inferiority trial. Lancet 2016;388:2743-52. [Crossref] [PubMed]
- Morice MC, Serruys PW, Kappetein AP, et al. Outcomes in patients with de novo left main disease treated with either percutaneous coronary intervention using paclitaxel-eluting stents or coronary artery bypass graft treatment in the Synergy Between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery (SYNTAX) trial. Circulation 2010;121:2645-53. [Crossref] [PubMed]
- Morice MC, Serruys PW, Kappetein AP, et al. Five-year outcomes in patients with left main disease treated with either percutaneous coronary intervention or coronary artery bypass grafting in the synergy between percutaneous coronary intervention with taxus and cardiac surgery trial. Circulation 2014;129:2388-94. [Crossref] [PubMed]
- Park SJ, Kim YH, Park DW, et al. Randomized trial of stents vs. bypass surgery for left main coronary artery disease. N Engl J Med 2011;364:1718-27. [Crossref] [PubMed]
- Baron SJ, Chinnakondepalli K, Magnuson EA, et al. Quality-of-Life After Everolimus-Eluting Stents or Bypass Surgery for Left-Main Disease: Results From the EXCEL Trial. J Am Coll Cardiol 2017;70:3113-22. [Crossref] [PubMed]
- Mahmoud AN, Elgendy IY, Mentias A, et al. Percutaneous coronary intervention or coronary artery bypass grafting for unprotected left main coronary artery disease. Catheter Cardiovasc Interv 2017;90:541-52. [Crossref] [PubMed]
- Kolh P, Windecker S, Alfonso F, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur J Cardiothorac Surg 2014;46:517-92. [Crossref] [PubMed]
- De Rosa S, Polimeni A, Sabatino J, et al. Long-term outcomes of coronary artery bypass grafting versus stent-PCI for unprotected left main disease: a meta-analysis. BMC Cardiovasc Disord 2017;17:240. [Crossref] [PubMed]
- Buszman PE, Buszman PP, Banasiewicz-Szkróbka I, et al. Left main stenting in comparison with surgical revascularization 10-year outcomes of the (left main coronary artery stenting) LE MANS trial. JACC Cardiovasc Interv 2016;9:318-27. [Crossref] [PubMed]
- Schwietz T, Spyridopoulos I, Pfeiffer S, et al. Risk stratification following complex PCI: clinical versus anatomical risk stratification including "post PCI residual SYNTAX-score" as quantification of incomplete revascularization. J Interv Cardiol 2013;26:29-37. [Crossref] [PubMed]
- Caiazzo G, Longo G, Giavarini A, et al. Optical coherence tomography guidance for percutaneous coronary intervention with bioresorbable scaffolds. Int J Cardiol 2016;221:352-8. [Crossref] [PubMed]
- Indolfi C, Mongiardo A, Spaccarotella C, et al. The instantaneous wave-free ratio (iFR) for evaluation of non-culprit lesions in patients with acute coronary syndrome and multivessel disease. Int J Cardiol 2015;178:46-54. [Crossref] [PubMed]
- Davies JE, Sen S, Dehbi HM, et al. Use of the Instantaneous Wave-free Ratio or Fractional Flow Reserve in PCI. N Engl J Med 2017;376:1824-34. [Crossref] [PubMed]
- De Rosa S, Polimeni A, Petraco R, et al. Diagnostic performance of the instantaneous wave-Free Ratio: comparison with Fractional Flow Reserve. Circ Cardiovasc Interv 2018;11:e004613. [Crossref] [PubMed]
- Lehmann R, Ehrlich JR, De Rosa S, et al. Impact of interventional strategy for unprotected left main coronary artery percutaneous coronary intervention on long-term survival. Can J Cardiol 2012;28:553-60. [Crossref] [PubMed]
- Chen SL, Zhang JJ, Han Y, et al. Double Kissing Crush Versus Provisional Stenting for Left Main Distal Bifurcation Lesions: DKCRUSH-V Randomized Trial. J Am Coll Cardiol 2017;70:2605-17. [Crossref] [PubMed]
- Chen SL, Xu B, Han YL, et al. Clinical Outcome After DK Crush Versus Culotte Stenting of Distal Left Main Bifurcation Lesions: The 3-Year Follow-Up Results of the DKCRUSH-III Study. JACC Cardiovasc Interv 2015;8:1335-42. [Crossref] [PubMed]
- Park SJ, Kim YH, Park DW, et al. Impact of intravascular ultrasound guidance on long-term mortality in stenting for unprotected left main coronary artery stenosis. Circ Cardiovasc Interv 2009;2:167-77. [Crossref] [PubMed]


