Biportal complete video-assisted thoracoscopic lobectomy and systematic lymphadenectomy
Introduction
In 2007, CALGB 39802, the first prospective, multicenter study to examine a standardized, truly videoscopic, minimally invasive video-assisted thoracoscopic surgery (VATS) lobectomy for early-stage lung cancer defined a VATS lobectomy as one procedure performed with videoscopic guidance and anatomic hilar vascular, bronchial, and lymphatic dissection using two or four ports and without rib spreading (1). However, there is no standardized technique for the VATS approach to date, though most centers use a utility incision of about 3-5 cm and generally positioned anteriorly. Most surgeons then add two other ports (one for the optics and another at posterior level) (2). Groups such as those led by Gossot describe purely thoracoscopic lobectomies involving three incisions with a minithoracotomy only for the extraction of the lobe (3). In Jun 2011, Gonzalez D first reported uniportal VATS lobectomy, which becomes a milestone in the development history of VATS lobectomy, yet still in its infancy (4). Just as first proposed by D’Amico, two-incision (also called as biportal) approach is a safe and versatile procedure (5). We adopt and develop this recently published approach from experiences with 402 consecutive patients. Here we present a biportal complete VATS (biportal cVATS) right upper lobectomy and systematic lymphadenectomy.
Clinical data
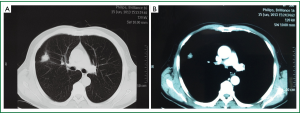
A 64-year-old male presented with a right upper lobe lesion on computed tomographic (CT) (Figure 1) was admitted in our institute on July 15th, 2013. The patient underwent preoperative staging and cardiac and pulmonary function assessment. PET-scan indicated no signs of metastasis. Under general anesthesia with double lumen tube, the patient underwent biportal cVATS lobectomy for right upper lung tumor on July 17th, 2013 (Video 1).
Operative techniques
Patient positioning and placement of incisions
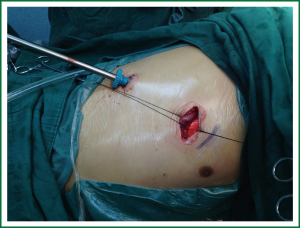
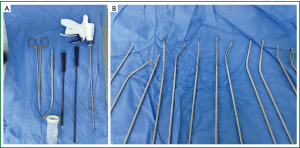
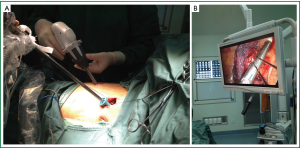
The patient is positioned in full lateral decubitus position with slight flexion of the table at the level of the mid-chest, which allows slight splaying of the ribs to improve exposure in the absence of rib spreading. Two incisions are used. The 30° 10 mm thoracoscope is placed in the 7th intercostal space slightly posterior to the midaxillary line, and a 4 cm anterior utility incision is placed in the 4th intercostal space anteriorly, providing access for hilar dissection. Plastic wound protector is not often used. Soft tissues are retracted by silk only for utility incision (Figure 2). The intercostals spaces are wider in this location, allowing for both better exposure and easier retrieval of specimens. Instruments are inserted directly through the incisions. We use a combination of endoscopic and open-surgery instruments (Figure 3).
Exploration
We begin the procedure with an exploration of the pleural cavity. The tumor is identified between anterior and posterior segment of the right upper lobe. Considering greater likelihood of malignancy, we proceed to right upper lobectomy and systematic lymphadenectomy.
Division of posterior mediastinal pleura
Move the operating table anteriorly. The first step following exploration is to loosen the pulmonary ligament, continue upward to cut open the posterior mediastinal pleura until turn around underneath the arch of the azygos vein at the top. This facilitates the exposure of the lung tissue.
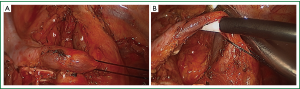
Division and transection of superior pulmonary vein
Move the operating table posteriorly. Pull the upper right lung backward with oval forceps through the utility incision to expose the anterior part of the right hilum. Sometimes, insert a suction device through the auxiliary port to assist the electrotome in freeing the right superior pulmonary vein. To cut open the tunica adventitia of vessel facilitates to further extend the vessels and subsequent stapler insertion. The location of endostapler and the thoracoscope are interchangeable between two incisions (Figure 4). This is the key point of biportal VATS lobectomy for the resection of hilar structures during upper and middle lobectomies. A reticulating endoscopic linear cutter is preferred. Lower lobectomy seems to be carried out with less difficulty because the whole procedure is performed through the utility incision.
Division and transection of truncus anterior and the posterior ascending artery
Then the apical and anterior branches behind the right superior pulmonary vein as well as the posterior ascending artery are divided and transected. We strongly recommend the use of silk ligation in cases where the angle for stapler insertion is not optimal. Forcing a stapler in a place where there is no good angle could cause a vascular accident, which could very easily be avoided by direct ligation. Keeping the silk tension-free during ligation by a knot pusher help locate the knot in case of no assistance.
Division and transection of right upper lobe bronchus
Identify and clear the lymph nodes between the upper and intermediate bronchus first. The distal lymph nodes at the second carina should be dissociated to the distal end of the bronchus, and then removed en bloc with the right upper pulmonary lobe. The bronchus can be transected via anterior hilum or posterior hilum by a stapler.
Dissection of the posterior halves of the oblique and horizontal fissure
The above fissures can be divided using stapler last or create a tunnel after division of superior vein and before division of artery.
Specimen retrieval
The lobe is extracted through the anterior superior incision using a specimen retrieval bag self-made from a latex glove. The intercostals muscles may have to be slightly enlarged to facilitate extraction.
Mediastinal lymph node dissection
Clear the hilar lymph nodes simultaneously with above structures. Systematic lymph node dissection using en bloc excision, instead of systematic sampling, is applied for the removal of 2, 4, 3a, 7, 8 and 9 mediastinal lymph nodes. Recently, we modify the procedures for mediastinal lymph node dissection. Cut open mediastinal pleura by a “∩” shaped incision for 7th, a “⊿” above azygos vein and “—” beneath azygos vein for 2th and 4th and a “□” for 3ath which greatly simplify the en bloc mediastinal lymph node dissection (Figures 5,6).

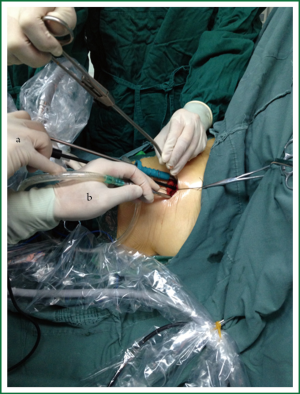
Leakage testing, intercostals nerve blockade, insert drainage tube and incision closure
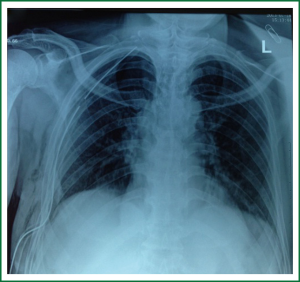
The lung is re-expanded for air leakage testing for the bronchial stump and the pulmonary resection margin. We use one chest tube with enough side holes introduced through the thoracoscopy port up to apex of thoracic cavity (Figure 7). The utility incision is routinely closed (Figure 8).
Comments
To date, the VATS approach to lobectomy for non-small-cell lung cancer (NSCLC) has not been standardized. Most centers and VATS lobectomists use two ports and an additional utility incision (2). However, to further reduce the number and the length of incisions has already become an irresistible trend (6). Gonzalez-Rivas developed and optimized uniportal VATS lobectomy from biportal and triportal VATS lobectomy (7). The optimistic estimate is that an upsurge of uniportal VATS lobectomy will be set off globally within the next few years. As experiences accumulated in these centers, VATS lobectomy has evolved from triportal VATS to biportal to uniportal approach. We share the same route of VATS learning curve with Gonzalez-Rivas group. From 1996 till Oct 2013, we have accomplished more than 6,000 cases of minimally invasive thoracic procedures among which there were 402 cases of biportal VATS lobectomy, 78 cases of uniportal VATS minor procedures and 4 cases of uniportal VATS lobectomy (3 cases of lower lobe lobectomy and 1 case of right upper lobectomy). We agree that previous experiences in the biportal approach and anterior minithoracotomy greatly flatten the learning curve of uniportal VATS lobectomy. In this respect, optimization of biportal approach is a critical prerequisite to uniportal approach (7).
As our experience gained, we considered the knacks of biportal VATS imply two radical changes of perspectives from the traditional three-portal technique. One fundamental step is how to achieve satisfactory exposure in the case of single utility incision for multiple instruments to insert? Our solutions to this problem are as follows. First, rigid trocar and the plastic wound protector seem to be unnecessary because “naked” utility incision does not interfere with the cross placement of the instruments and provides maximal working space for both identification and resection of the neoplasm. Second, to minimize the number of instruments that are simultaneously used. The “pick” technique with an electric hook can safely peel the mediastinal pleura and tissues surrounding hilar structures. Right-angle clamp with a thread for looping the vessels often needs a curved forceps to fetch. We use instead a right-angle clamp to take a silk thread with a circle at the tip of it to directly loop the vessels which can avoid another forceps. Meanwhile, knot pusher should not push thread with tension as usual in open surgery or video-assisted minithoracotomy when a forceps help to locate, otherwise the knot is difficult to be in optimal place. Often it is simpler and less bloody to remove a whole package at a given site than just a single node, especially if very fatty, so we prefer en bloc resection for 7 and 8, R2 and R4, L5 and L6. “No grasping” technique is applied in almost the entire process of lymph node dissection by electric hook and ultrasonic scalpel without ring clamp grasping the target tissue. Routinely, two instruments are enough for exposure and dissection, sometimes three are needed. Thus, the inferior and the upper part of the utility incision belonging to different instruments is essential. Third, the operating table to be rotated to different body postures facilitates the exposure. Move the operating table according to each procedure: hilar vascular dissection (posterior rotation), lymph node dissection (anterior rotation), paratracheal (head up) and subcarinal (head down). Fourth, we prefer a 30° 10 mm high definition video thoracoscope as it provides a multiple axis view allowing different orientation. Also, zoom effect by close vision is necessary for precise anatomic manipulation and avoidance of too much exposure needed. Fifth, whichever lobe to be resected, the first step following exploration is to loosen the pulmonary ligament, continue upward to cut open the posterior mediastinal pleura until turn around underneath the arch of the azygos vein or aorta at the top. Meanwhile, 9, 8 and 7th lymph nodes are resected. All these can help lung retraction and facilitate manipulation by ring-type sponge-holding forceps.
Another technical tip that should be taken into account is how to introduce staplers without the third posterior port conveniently? This has ever been found to be the most time-consuming step. The following can be performed to facilitate the insertion of the staplers and minimize the risk of vascular injury. First, the location of endostapler and the thoracoscope are interchangeable between two incisions, usually it is necessary for the resection of hilar structures during upper and middle lobectomies.
Confusion of orientation is a bit problematic for the operator or assistants because of deviation of the view angle in earlier cases. A reticulating endoscopic linear cutter such as Flex (Johnson & Johnson, USA) or Tristaple (Covidien, USA) is preferred. Second, a proper execution of the above-mentioned port site is essential. Based on our experiences, more anterior utility port and more posterior thoracoscope port is better so that they do not collide with each other. Third, if the gap between the blood vessel and its surrounding tissues is small, it can pass through the gap under the guidance of a guiding tube before the triggering, which is safer. Fr. 16 disposable catheter is used in our clinical practice. Fourth, usually, to cut open the tunica adventitia of vessel facilitates further extension of the vessels and insertion of subsequent stapler. And simultaneous dissection of N1 lymph node during the course of individual hilar structure is conducive to free the pulmonary vessels with a sufficient length. Fifth, alternatively, a silk-thread ligation of blood vessels with a knot pusher, clamping with a vascular clip or direct cut with an ultrasonic scalpel is convenient and economical depending on the vessels and its angle whilst large vessels and lung parenchyma are divided using endoscopic stapling devices to ensure haemostasis and aerostasis.
There is another important aspect, the instrumentation interference with each other in and out thoracic cavity (5). Instrumentation with both proximal and distal articulation, modern articulated staplers, high definition 30° cameras and energy devices seem to be more fitted for successful biportal VATS lobectomy. And bi-manual instrumentation using cross hand technique is often used (Figure 9).
Systematic lymph node dissection is routinely performed in all biportal VATS procedures. For right-sided tumors, nodal stations 2, 3, 4, 7-12. Cut open mediastinal pleura by a “∩” shaped incision for 7th, a “⊿” above azygos vein and “—” beneath azygos vein for 2th and 4th and a “□” for 3ath which greatly simplify the en bloc mediastinal lymph node dissection. We preserve the azygos vein in most cases because we believe azygos vein can help to exposure especially for the lymph node beneath the bifurcation between azygos vein and vena cava which is critical for the beginning of en bloc excision of R2 and 4 under the azygos vein bridge. Also, the tip of “⊿” mediastinal pleura cut above azygos vein draws a red line against any injury to the right recurrent laryngeal nerve. For 7th and 8th, a “∩” shaped incision mediastinal pleura is cut to disperse right bronchus and esophagus and en bloc excision following the counterclockwise route from right bronchus to carina to left bronchus and esophagus, which avoid the likelihood of injury to the thoracic duct. This modification provides average lymph nodes harvest from 16 in earlier cases to 25 in recent 100 cases.
While for left-sided stations 5-12, average lymph nodes harvest less than right–sided partly can be explained by dissection of L7, which is believed to be taxing and time-consuming and requires a prepared and patient maneuver, especially by biportal approach. We rountinely employ this posterior approach. Also, the anterior approach to the subcarinal area after left upper lobectomy was applied to some cases according to Kwhanmien Kim (8). However, it is difficult to perform well for every structure “naked” of the right-sided.
To summarize, biportal VATS lobectomy is applicable in the selected cases and may obtain similar results with the conventional VATS lobectomy through a certain period of learning curve. Greater emphasis will be placed on uniportal approach on adequate exposure, stapler introduction angle and instrumentation interference (9). Process optimization of biportal VATS lobectomy will flatten the learning curve of uniportal approach.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Swanson SJ, Herndon JE 2nd, D’Amico TA, et al. Video-assisted thoracic surgery lobectomy: report of CALGB 39802--a prospective, multi-institution feasibility study. J Clin Oncol 2007;25:4993-7. [PubMed]
- McKenna RJ Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg 2006;81:421-5; discussion 425-6. [PubMed]
- Gossot D, Girard P, Raynaud C, et al. Totally endoscopic major pulmonary resection for stage I bronchial carcinoma: initial results. Rev Mal Respir 2009;26:961-70. [PubMed]
- Gonzalez D, de la Torre M, Paradela M, et al. Video-assisted thoracic surgery lobectomy: 3-year initial experience with 200 cases. Eur J Cardiothorac Surg 2011;40:e21-8. [PubMed]
- Onaitis MW, Petersen RP, Balderson SS, et al. Thoracoscopic lobectomy is a safe and versatile procedure: experience with 500 consecutive patients. Ann Surg 2006;244:420-5. [PubMed]
- Gonzalez-Rivas D. VATS lobectomy: surgical evolution from conventional VATS to uniportal approach. ScientificWorldJournal 2012;2012:780842.
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [PubMed]
- Kim K. Video-assisted Thoracic Surgery Lobectomy. Korean J Thorac Cardiovasc Surg 2011;44:1-8. [PubMed]
- Bertolaccini L, Rocco G, Viti A, et al. Geometrical characteristics of uniportal VATS. J Thorac Dis 2013;5:S214-6. [PubMed]