Symptomatic sinus arrest induced by acute marijuana use
Case vignette
A 54-year-old female presented to the emergency department (ED) after episodes of decreased levels of consciousness following acute marijuana use. The intermittent episodes were presyncopal, where the patient felt frequent dizziness with tingling sensations around the left-side of the mouth, as well as in the left arm with chest pressure and lightheadedness for 2 hours. The past medical history was significant for frontotemporal craniotomy for brain aneurysm, cerebrovascular accident, and chronic obstructive pulmonary disease. There was no previous history of coronary artery disease, myocardial infarction, angina, palpitations, or chest pain. The patient was receiving antidepressants, bronchodilators, narcotics, and anti-inflammatory agents, all without changes prior to this indexed episode.
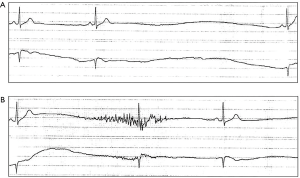
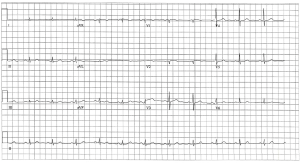
The patient was a regular cigarette (1 pack/day) and marijuana (3 g/day-joint) smoker. On this particular occasion, she reportedly smoked 1 g of marijuana and noted the aforementioned symptoms for the first time. While in the ED, the initial heart rate varied between 70–103 beats per minute (bpm) under sinus rhythm. Shortly after, she was witnessed to have an episode of sinus arrest with a 4.6 s pause where the heart rate dropped to 38 bpm (Figure 1A). After a few beats, another prolonged asystole was observed (Figure 1B). Sinus rhythm resumed several hours after admission and her symptoms self-resolved (Figure 2). Upon physical examination, the patient had normal heart sounds and no significant murmurs. Her blood pressure was 118/70 mmHg, O2 saturation of 92% and a temperature of 36.4 °C. The echocardiogram was normal. Upon follow-up of whether a pacemaker was warranted, the patient was non-compliant and did not return.
ECG description and discussion
The rhythm strips on admission (Figure 1) demonstrate sinus arrest resulting hours after consumption of 1 g of marijuana in a patient with no previous cardiac history. This likely represents a sudden increase in vagal tone and parasympathetic activity due to marijuana consumption (1). It has been shown experimentally that marijuana can induce severe postural dizziness and syncope in a small randomized study with healthy subjects. Subjects who experienced severe dizziness stood upright after drug intake, and a drop in pulse-rate, middle cerebral artery blood-velocity, and blood pressure was observed (2). Recently there has been a steady increase in case reports describing asystolic events shortly following marijuana usage. Menahem reported sinus arrest with 17 pauses and 2 syncopal episodes in a 21-year-old male who had consumed 25–35 “bongs” of 1 g marijuana mixed with tobacco. The previous history was significant for congenital heart disease and cardiac surgery (3). Brancheau et al. linked marijuana use to sinus arrest and recurrent syncope in a 28-year-old healthy male with no previous cardiac history, although the amount of marijuana consumed was not reported (1). These cases document young male patients experiencing asystolic episodes followed by syncope. Our case adds to the growing literature and demonstrates an example of sinus pauses most likely induced by marijuana intake in a female with no previous cardiac history. In our case, the patient did not lose complete consciousness, and this could be due to the patient being seated or reclined.
As no toxic screening, serum or urine tests were performed, an ideal causal relationship cannot be established, however since the sinus arrest and presyncopal symptoms shortly succeeded marijuana inhalation, a presumptive cause-and-effect relationship was inferred. Our case, in conjunction with previous literature, may allow clinicians to stay vigilant in recognizing the electrocardiographic pathologies in the context of marijuana use as a sinus arrest during extreme increases in parasympathetic activity may precede a cardiac arrest.
Points to ponder
Marijuana use has been linked to serious adverse outcomes. The main psychoactive component of marijuana is Δ9-tetrahydrocannabinol (THC), which mediates its effects by interacting with two G-protein-coupled cannabinoid specific receptors—CB1 and CB2. The CB1 receptor is most abundantly expressed in the brain, whereas CB2 is normally present in the cells of the immune system (4,5). Marijuana is postulated to affect the autonomic nervous system in a dose-dependent manner, where a low-to-moderate intake induced tachycardia and raised blood pressure via sympathetic stimulation, whereas a high dose is linked to hypotension and bradycardia through a predominant increase in parasympathetic activity (5). It can also produce more serious, life-threatening, ventricular arrhythmias (6). Due to the aforementioned findings, cannabis smokers presenting with symptoms such as syncope and presyncope should be offered monitoring.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Brancheau D, Blanco J, Gholkar G, et al. Cannabis induced asystole. J Electrocardiol 2016;49:15-7. [Crossref] [PubMed]
- Mathew RJ, Wilson WH, Davis R. Postural syncope after marijuana: a transcranial Doppler study of the hemodynamics. Pharmacol Biochem Behav 2003;75:309-18. [Crossref] [PubMed]
- Menahem S. Cardiac asystole following cannabis (marijuana) usage--additional mechanism for sudden death? Forensic Sci Int 2013;233:e3-5. [Crossref] [PubMed]
- Pacher P, Steffens S, Haskó G, et al. Cardiovascular effects of marijuana and synthetic cannabinoids: the good, the bad, and the ugly. Nat Rev Cardiol 2017. [Epub ahead of print]. [Crossref] [PubMed]
- Menahem S. Chapter 50: Cardiovascular Effects of Cannabis Usage. In: Preedy VR. editor. Handbook of Cannabis and Related Pathologies. San Diego: Academic Press, 2017:481-5.
- Baranchuk A, Johri AM, Simpson CS, et al. Ventricular fibrillation triggered by marijuana use in a patient with ischemic cardiomyopathy: a case report. Cases J 2008;1:373. [Crossref] [PubMed]


