The potential role of postbronchoscopic fever on the postoperative outcomes in patients with non-small cell lung cancer
Introduction
Postbronchoscopic fever is a common phenomenon with a reported incidence rate of 2.5–21% (1-5). Transient fever is the most common pattern of postbronchoscopic fever which begins 2–8 hours after examination and lasts for 11–14 hours and return to normal without any intervention (6). Multiple factors of clinical characteristics and bronchoscopy procedure were not independent risk factors of postbronchoscopic fever (7). No organisms were isolated from blood culture specimens drawn at the time of fever (6,7). Moreover, there was no relationship between tumor load and postbronchoscopic fever (4). The mechanism of fever is unclear and the most accepted theory is acute inflammatory reaction or systemic inflammatory response induced by inflammatory cytokines. Bronchoscopy is a routine examination for NSCLC preoperation. Postbronchoscopic fever may be put into carefully consideration due to the underlying preoperative inflammation or infection, especially one day before operation. No reports have related postbronchoscopic fever with postoperative complications. Improved understanding of this phenomenon is needed because it may predispose some patients to develop infective or worse medical conditions.
An observational and retrospective study was conducted to assess the frequence of postbronchoscopic fever and to evaluate the risk of postoperative complications.
Methods
Patients with non-small cell lung cancer (NSCLC) undergoing operation between July 2015 and December 2015 in the Chest Surgery Department of the First Affiliated Hospital of SUN YAT-SEN University were enrolled in this study. Patients received routine preoperative bronchoscopy. Exclusion criteria were as follows: central type NSCLC, combining rheumatoid immune diseases, concurrent treatment with antibiotics and systemic corticosteroid, fever higher than 37.5 °C during the 48 hours before bronchoscopy, preoperative chemotherapy or radiotherapy, severe complications of bronchoscopy, massive haemorrhage during operation and postoperative blood transfusion, second operation. Approval for the research was obtained from the institutional review board of the First Affiliated Hospital of SUN YAT-SEN University.
Fever was considered to be elevation of axillary body temperature of 37.5 °C or higher postoperatively or within 24 hours postbronchoscopy. Preoperative assessment was completed on every patient according to NCCN guidelines (8). Lobectomy and mediastinal lymph node dissection were performed by video-assisted thoracoscopic surgery (VATS) or thoracotomy if the frozen section confirmed NSCLC. Prophylactic antibiotics were used 24–48 hours after operation with first- or second-generation cephalosporins (9). Upgrading use of antibiotics were advised if fever or count raised to more than 12×109/L on the third postoperative day. Sometimes original antibiotics were continued for one more day under the advice of surgeons.
Study outcomes included days of postoperative fever, days of postoperative antibiotic use, days of drainage, WBC counts on the first and third postoperative day. Days of postoperative fever was defined as days with elevation of axillary body temperature of 37.5 °C or higher in patients, from the first postoperative day to the discharge. Days of postoperative antibiotic use was defined as days from the first administration to the day antibiotics were stopped. Drainage tube was put regularly after operation and was removed until drainage fluids were less than 150 mL/day without air leakage.
Patients were divided into two groups for the purposes of this study: fever group (postbronchoscopic fever) and normal group (without postbronchoscopic fever).
All statistical analyses were performed with SPSS version 19. The data are shown as mean ± standard deviation. The data of both groups were compared using unpaired t-test of the chi-square test. A P value <0.05 was considered significant.
Results
Patients characteristics are shown in Table 1. Seventy-five patients diagnosed with NSCLC were enrolled in this study and 12 cases (16%) developed postbronchoscopic fever. Abnormal bronchoscopic finding such as obstruction and narrowing were not observed in any case. Biopsy was not performed. The mean age of 75 patients was 59.8 with a significant older age in the fever group (65.8 vs. 58.7, P=0.02). There were no significant differences between the two groups considering preoperative characteristics: gender (male, 66.7% vs. 63.5%), cigarette smoker (ever, 50% vs. 68.3%), preoperative WBC counts (6.4 vs. 7.0×109/L, P=0.414), serum albumin (ALB) (41.6 vs. 41.8 g/L, P=0.78), carcinoembryonic antigen (CEA) (3.1 vs. 13.4 µg/L, P=0.11). On comparison of characteristics of pathology and stage, the two groups also were found to have no significant differences in tumor size (2.8 vs. 3.2 cm, P=0.41), pathology (P=0.293), differentiation (P=0.87), grade (P=0.15).
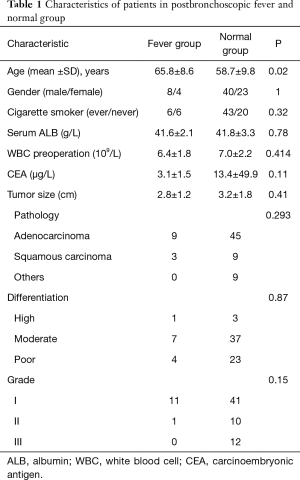
Full table
Table 2 shows the study outcomes in the two groups. The fever group was found to have longer postoperative fever time (1.9 vs. 0.8 days, P=0.02), more postoperative antibiotic use (3.4 vs. 2.5 days, P=0.005) and longer drainage (7.2 vs. 4.7 days, P=0.001). There were 3 cases of postoperative pulmonary infection, one case in the fever group and two cases in the normal group. WBC counts of the fever group were higher than those of the normal group on the first (14.5 vs. 11.4×109/L, P=0.003) and third (11.0 vs. 9.2×109/L, P=0.04) postoperative day.
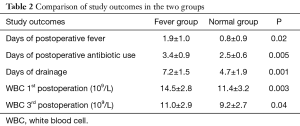
Full table
All patients were stratified by a median age (60) into a younger subgroup (<60) and an older subgroup (<60) (Table 3). In the younger subgroup, days of drainage were longer in the fever group (6.0 vs. 4.2 days, P=0.02), other study outcomes were not significantly different between two groups. In the older subgroup, study outcomes were longer in the fever group: days of postoperative fever (2.0 vs. 0.8 days, P=0.01), days of postoperative antibiotic use (3.6 vs. 2.5 days, P<0.05), days of drainage (7.6 vs. 5.1 days, P=0.004), WBC counts on the first (14.6 vs. 11.3×109/L, P=0.01) and third day (11.7 vs. 9.4×109/L, P=0.017) postoperative day. Surgical procedures may be a confounding factor, we analysed the study outcomes between the thoracotomy subgroup and the VATS subgroup (Table 4). There were no significant differences between the two subgroups.
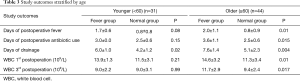
Full table
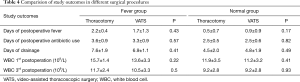
Full table
Discussion
Fiberoptic bronchoscopy is accepted as a routine and safe diagnostic method with low morbidity and mortality in NSCLC patients (8,10). Postbronchoscopic fever was found in 16% of 75 NSCLC patients in this study. In the fever group, longer postoperative drainage was observed. Longer postoperative fever and more postoperative antibiotic use were observed in the fever group especially in the older subgroup (≥60). The WBC counts were higher in the fever group and maintained at high levels for a longer time.
The mechanism of postbronchoscopic fever is unclear. The early speculation was “transient bacteremia”, but no microbiological evidences were found (6,7). Moreover, prophylactic antibiotics before bronchoscopy did not reduce the frequency of postbronchoscopy fever (11). These findings suggest that microbiological factors may not be responsible for the development of postbronchoscopy fever. However the overall incidence of pneumonia after bronchoscopy was 5.6% in patients older than 70 (12). Acute phase reaction (13) and systemic inflammatory response (14-16) were raised as new theories which were specific defensive reaction of organism. Fever, elevated serum acute phase protein and elevated peripheral white blood cells were observed after bronchoscopy. What is the role of this specific reaction on the operable NSCLC patients has not been analysed. If this could be ascertained, postbronchoscopic fever might act as a predictive factor on postoperative complications and lead to prophylactic intervention measures.
Postbronchoscopic fever is a well-known adverse reaction (1-5). Strumpf et al. reported 2.5% of 281 procedures that developed postbronchoscopic fever (2). Postbronchoscopic fever was found in 21% of healthy volunteers (3). In a prospective study, postbronchoscopic fever was found in 16% of 100 bronchoscopies (1). The differences may be due to the populations enrolled in each study and to the different definition of fever. 37.5 °C was defined as boundary in this study and the report of Deng with a incidence rate of 11% (4). However 38 °C was defined as boundary in other studies with incidence rate of 2.5% (2) and 6.7% (12). Age was associated with differences in postbronchoscopic fever (12,17,18). Postbronchoscopic fever was a common event in immunocompetent children (18). There was increased risk for adverse events with increasing age (17). However, Kanemoto et al. declared that increasing age was not associated with increasing fever after bronchoscopy (12). Um et al. found that the final diagnosis of pulmonary tuberculosis was identified as independent risk factor of postbronchoscopic fever (7), though there was no relationship between tumor load and postbronchoscopy fever (4).
Inflammatory factors such as TNF, IL-1, IL-6 and G-CSF were elevated postbronchoscopy and higher in postbronchoscopic fever patients (14-16). WBC counts were higher in the fever patients postbronchoscopy (16). One dose of dexamethasone administered prior to performing bronchoscopy may prevent fever subsequent to the procedure (19). Moreover, steroid pretreatment before surgery reduced the early postoperative inflammatory response without increasing postoperative infection (20).
This excessive inflammatory response was obvious in the postbronchoscopic fever patients. In operable NSCLC patients, this specific reaction might again play an important role postoperatively. In this study, we found longer postoperative drainage, longer postoperative fever and more postoperative antibiotic use in the postbronchoscopic fever group. Moreover, the WBC counts were higher in the postbronchoscopic fever group and maintained at high levels for a longer time. In the report of steroid pretreatment before surgery, there was no postoperative infection complication in groups. WBC did not differ between groups. However, the serum CRP was suppressed in the steroid group (20). It is uncertain yet if preoperative prophylactic intervention measures, such as steroid pretreatment, can reduce postoperative inflammatory response leading to shorter drainage time, less antibiotic use and rapid recovery.
Postbronchoscopic fever is a common adverse reaction in operable NSCLC patients. Postbronchoscopic fever may be a predictor of longer postoperative fever, longer drainage and more antibiotic use. Further studies should be developed to verify the relationship between postbronchoscopy inflammatory factors, such as CRP, and the postoperative outcomes. And further evaluation of the role of preoperative prophylactic intervention measures in these patients is needed.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Approval for the research was obtained from the institutional review board of the First Affiliated Hospital of SUN YAT-SEN University (No. [2017]176).
References
- Pereira W, Kovnat DM, Khan MA, et al. Fever and pneumonia after flexible fiberoptic bronchoscopy. Am Rev Respir Dis 1975;112:59-64. [PubMed]
- Strumpf IJ, Feld MK, Cornelius MJ, et al. Safety of fiberoptic bronchoalveolar lavage in evaluation of interstitial lung disease. Chest 1981;80:268-71. [Crossref] [PubMed]
- Burns DM, Shure D, Francoz R, et al. The physiologic consequences of saline lobar lavage in healthy human adults. Am Rev Respir Dis 1983;127:695-701. [PubMed]
- Deng XM, Tan XY. HE QY. An investigation of clinical characteristics of fever and infection after flexible fiberoptic bronchoscopy. China Journal of Endoscopy 2006;12:673-6.
- Krause A, Hohberg B, Heine F, et al. Cytokines derived from alveolar macrophages induce fever after bronchoscopy and bronchoalveolar lavage. Am J Respir Crit Care Med 1997;155:1793-7. [Crossref] [PubMed]
- Drummond M, Magalhães A, Hespanhol V. Transient fever after fiberoptic bronchoscopy--a prospective study. Rev Port Pneumol 2004;10:87-95. [Crossref] [PubMed]
- Um SW, Choi CM, Lee CT, et al. Prospective analysis of clinical characteristics and risk factors of postbronchoscopy fever. Chest 2004;125:945-52. [Crossref] [PubMed]
- Ettinger DS, Kris MG. Update: NCCN non-small cell lung cancer clinical practice guidelines. J Natl Compr Canc Netw 2004;2 Suppl 3:S-9-13. [PubMed]
- Park JS, Lee CH, Yim JJ, et al. Impact of antibiotic prophylaxis on postbronchoscopy fever: a randomised controlled study. Int J Tuberc Lung Dis 2011;15:528-35. [Crossref] [PubMed]
- The Chinese medical association respiratory neurology, bronchoscope dehaene. Fiber bronchoscope (flexible bronchoscope) clinical practice guidelines (draft). Zhonghua Jie He He Hu Xi Za Zhi 2000;23:134.
- Park JS, Lee CH, Yim JJ, et al. Impact of antibiotic prophylaxis on postbronchoscopy fever: a randomised controlled study. Int J Tuberc Lung Dis 2011;15:528-35. [Crossref] [PubMed]
- Kanemoto K, Satoh H, Ishikawa H, et al. Prospective study of fever and pneumonia after flexible fiberoptic bronchoscopy in older people. J Am Geriatr Soc 2006;54:827-30. [Crossref] [PubMed]
- Huang YC, Bassett MA, Levin D, et al. Acute phase reaction in healthy volunteers after bronchoscopy with lavage. Chest 2006;129:1565-9. [Crossref] [PubMed]
- Standiford TJ, Kunkel SL, Strieter RM. Elevated serum levels of tumor necrosis factor-alpha after bronchoscopy and bronchoalveolar lavage. Chest 1991;99:1529-30. [Crossref] [PubMed]
- Krause A, Hohberg B, Heine F, et al. Cytokines derived from alveolar macrophages induce fever after bronchoscopy and bronchoalveolar lavage. Am J Respir Crit Care Med 1997;155:1793-7. [Crossref] [PubMed]
- Terashima T, Amakawa K, Matsumaru A, et al. BAL induces an increase in peripheral blood neutrophils and cytokine levels in healthy volunteers and patients with pneumonia. Chest 2001;119:1724-9. [Crossref] [PubMed]
- Hehn BT, Haponik E, Rubin HR, et al. The relationship between age and process of care and patient tolerance of bronchoscopy. J Am Geriatr Soc 2003;51:917-22. [Crossref] [PubMed]
- Picard E, Schwartz S, Goldberg S, et al. A prospective study of fever and bacteremia after flexible fiberoptic bronchoscopy in children. Chest 2000;117:573-7. [Crossref] [PubMed]
- Picard E, Goldberg S, Virgilis D, et al. A single dose of dexamethasone to prevent postbronchoscopy fever in children: a randomized placebo-controlled trial. Chest 2007;131:201-5. [Crossref] [PubMed]
- Maruta K, Aoki A, Omoto T, et al. The Effect of Steroid Therapy on Postoperative Inflammatory Response after Endovascular Abdominal Aortic Aneurysm Repair. Ann Vasc Dis 2016;9:168-72. [Crossref] [PubMed]


