Incidental adult polysplenia with situs inversus, interrupted inferior vena cava with azygos continuation, patent ductus arteriosus, and aortic branches variations: a case report
Introduction
Polysplenia syndrome is a rare disease (about 2.5:100,000 live births) wherein a person has two or more spleens with accompanying various thoracic and abdominal organ abnormalities. Adult presentation of heterotaxic syndromes and related complexes, approximately 50–90% of polysplenia cases are associated with cardiac abnormalities, and only about 10% of people are expected to live until adulthood without complications (1). Situs inversus, a condition in which visceral organs are in mirror image from normal locations, is another rare disease entity with an incidence of 1:1,400 to 1:35,000 and polysplenia is usually associated with the situs ambiguous anomaly (1-3).
Here, we report a rare case of incidentally found polysplenia syndrome combined with situs inversus totalis in a 59-year-old female patient who also had an interrupted inferior vena cava (IVC) with azygos continuation, patent ductus arteriosus (PDA), and variations in the aortic arch branches. An aberrant left subclavian artery with Kommerell’s diverticulum and a large aneurysm of the non-aberrant, proximal-right subclavian artery were also noted by multi-detector computed tomography (MDCT) imaging. This study was approved by the institutional review board of Kyung Hee University Hospital (2017-12-068) with the requirement for informed consent being waived.
Case presentation
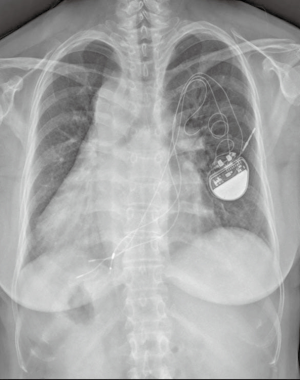
A 59-year-old woman was referred to our hospital for evaluation of exertional dyspnea and a chest X-ray abnormality. She also complained of discomfort in the right clavicular area. About 27 years ago, she underwent pacemaker insertion (VVI; ventricle pacing, ventricle sensing, inhibited by ventricle events) for management of sick sinus syndrome at a different hospital. She had known from a young age that she had dextrocardia. She had no history of operation, trauma (including severe trauma can result in spleen injury), hypertension, or malignancy in her family. A chest X-ray showed dextrocardia, left-sided hepatic contour, a right-sided aorta, and an enlarged cardio-thoracic ratio. Her pacemaker was well positioned (Figure 1). Echocardiography revealed atrial fibrillation with a ventricular frequency of 90 beats per minute (not shown here). Enhanced chest MDCT imaging was performed using a 128-slice MDCT scanner (Ingenuity core 128; Philips Medical Systems, Best, The Netherlands), which was confirmed during diagnosis.
Her enhanced computed tomography (CT) image showed dextrocardia with the liver on the left side, and the spleen and stomach on the right side, consistent with situs inversus. Observations of CT images in the lung window setting showed a right-sided bilobed lung and a left-sided trilobed lung. No active lung lesions were observed. Multiple spleens were noted on the right side of the upper abdomen, along the greater curvature of the stomach. The absence of the hepatic segment of the IVC with azygos continuation was also noted. A dilated azygos vein drained into the superior vena cava. Hepatic veins drained directly into the supra-hepatic part of the IVC and the right atrium. Variation in the aortic arch branches was also observed: both common carotid arteries and subclavian arteries branched off separately from the aortic arch. Furthermore, the left subclavian artery aberrantly originated from the right-sided aortic arch with Kommerell’s diverticulum and the artery coursed posterior to the trachea and esophagus. MDCT also showed PDA and a large aneurysm of the non-aberrant, proximal-right subclavian artery (Figure 2). The patient had no other associated congenital malformations.

The patient was discharged in good condition with medical therapy. At the time of writing this article, the patient has been monitored for 8 months and continues to be in good physical condition without significant symptoms.
Discussion
Polysplenia syndrome is a rare congenital disorder generally diagnosed in early childhood due to various and severe cardiac abnormalities. The majority of polysplenia patients (75%) die by the age five due to severe cardiovascular anomalies (1,2). However, isolated occurrence without severe cardiovascular anomalies may go unnoticed during early life and may be detected incidentally during radiologic examination or vascular interventions (4). The spectrum of abnormalities in patients with this syndrome can be broad. In addition to multiple spleens, there are often cardiac anomalies, interruption of the IVC with azygos continuation, bilateral hyparterial bronchi, and abdominal heterotaxia (1,2,5). This case included polysplenia syndrome in an adult patient who also had situs inversus totalis, an interrupted IVC with azygos continuation, and PDA. MDCT revealed separate origins of both the common carotid and subclavian arteries from the aortic arch. An aberrant left subclavian artery with Kommerell’s diverticulum and a large aneurysm of the non-aberrant, proximal right subclavian artery were also noted. According to the classification by Vučurević et al. (6), our case can be classified as having a type-IV aortic arch branching pattern with situs inversus totalis. This type-IV pattern and aberrant subclavian artery with Kommerell’s diverticulum is a rare anomaly of the aortic arch (6,7). Furthermore, aneurysms of the adjacent descending thoracic aorta or the non-aberrant subclavian artery may also be present in this type of branching and they can cause serious complications. Fortunately, our case had no significant symptoms or complications and did not require any specific treatment.
“Heterotaxy” broadly refers to a wide spectrum of anomalies involving malposition and dysmorphism of the thoracoabdominal organs and vessels across the left-right axis of the body (5,8). In a narrow sense, heterotaxy is a somewhat ambiguous entity that includes situs ambiguous and can classify into several conditions, including asplenia (right isomerism) and polysplenia (left isomerism) syndromes. Right isomerism involves bilateral trilobed lungs, bilateral eparterial bronchi, and bilateral right atria with asplenia. Left isomerism involves bilateral bilobed lungs, bilateral hyparterial bronchi, and bilateral left atria with multiple spleens (5,8). However, our case had polysplenia without definite isomerism.
Polysplenia is also usually accompanied by abdominal-organ abnormalities, including renal agenesis or hypoplastic kidneys, double ureters, and a short pancreas. These gastrointestinal abnormalities can cause variable symptoms or disease, such as abdominal pain and pancreatitis. However, in our case, only the absence of the hepatic segment of the IVC with azygos continuation was noted in the abdominal area. Anomalous IVC is frequently accompanied by various rhythm disorders, such as sick sinus syndrome (4,9). Kakura et al. (9) suggested that in sick sinus syndrome cases, pacemaker cells do not differentiate during development and, thus, produce hypoplastic sinus nodes. Our adult case previously received a pacemaker due to sick sinus syndrome and, in her case, this condition may be associated with an interrupted IVC.
Although most of these anomalies were detected incidentally, knowledge of the presence of vascular anomalies and situs inversus could be important if the affected individual needs to undergo catheterization of vessels coursing to the right side of the heart, electrophysiologic studies, cardiopulmonary bypass surgery, IVC filter placement, temporary pacing through the transfemoral route, or arterial angiography (4,9). Recent advances in MDCT technology can lead to incidental diagnoses of these complex anomalies.
In summary, herein, we report a rare case of incidentally found polysplenia syndrome combined with situs inversus totalis in a 59-year-old female patient with an interrupted IVC with azygos continuation, PDA, and variations in the aortic arch branches. MDCT also revealed an aberrant left subclavian artery with Kommerell’s diverticulum and a large aneurysm in the non-aberrant, proximal-right subclavian artery. We want to emphasize knowledge of anatomical details using MDCT can be important in diagnosis and management of such patient.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: This study was approved by the institutional review board of Kyung Hee University Hospital (2017-12-068) with the requirement for informed consent being waived.
References
- Gayer G, Apter S, Jonas T, et al. Polysplenia syndrome detected in adulthood: report of eight cases and review of the literature. Abdom Imaging 1999;24:178-84. [Crossref] [PubMed]
- Kayhan A, Lakadamyali H, Oommen J, et al. Polysplenia syndrome accompanied with situs inversus totalis and annular pancreas in an elderly patient. Clin Imaging 2010;34:472-5. [Crossref] [PubMed]
- Rasool F, Mirza B. Polysplenia syndrome associated with situs inversus abdominus and type I jejunal atresia. APSP J Case Rep 2011;2:18. [PubMed]
- Vijayvergiya R, Bhat MN, Kumar RM, et al. Azygos continuation of interrupted inferior vena cava in association with sick sinus syndrome. Heart 2005;91:e26. [Crossref] [PubMed]
- Kim SJ. Heterotaxy syndrome. Korean Circ J 2011;41:227-32. [Crossref] [PubMed]
- Vučurević G, Marinković S, Puškaš L, et al. Anatomy and radiology of the variations of aortic arch branches in 1,266 patients. Folia Morphol (Warsz) 2013;72:113-22. [Crossref] [PubMed]
- Kouchoukos NT, Masetti P. Aberrant subclavian artery and Kommerell aneurysm: surgical treatment with a standard approach. J Thorac Cardiovasc Surg 2007;133:888-92. [Crossref] [PubMed]
- Jacobs JP, Anderson RH, Weinberg PM, et al. The nomenclature, definition and classification of cardiac structures in the setting of heterotaxy. Cardiol Young 2007;17 Suppl 2:1-28. [PubMed]
- Kakura H, Miyahara K, Sohara H, et al. Isolated Levocardia Associated with Absence of Inferior Vena Cava, Lobulated Spleen and Sick Sinus Syndrome. Jpn Heart J 1998;39:235-41. [Crossref] [PubMed]


