A novel simple external fixation for securing silicone stent in patients with upper tracheal stenosis
Introduction
Upper tracheal stenosis, which is considered as a potentially life-threatening condition, results from endotracheal intubation, tracheostomy, trauma, infections, tumor or tumor-related treatment, and congenital disorders (1). Surgical resection and reconstruction is the gold standard for the treatment of tracheal stenosis. However, for the patients ineligible for surgery due to poor general condition, airway stenting is the option of treatment (2-6). Currently available stents mainly include silicone stent and metal stent. Silicone stent is one of the most widely clinically used stents. It is well tolerated, easily removable and exchanged, and relatively inexpensive. However, one of major disadvantages of silicone stent used in upper tracheal stenosis is the high risk of stent migration. To resolve this issue, we therefore in this report described a novel simple method, i.e., to externally fix silicone stent when placing it in patients with upper tracheal stenosis.
Technique
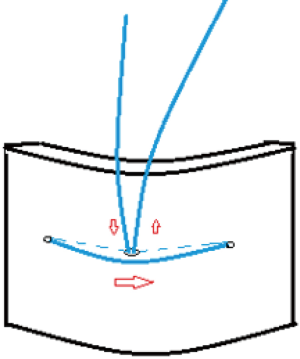
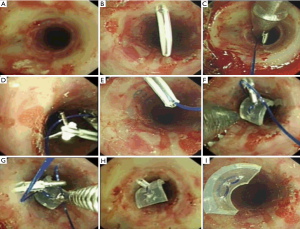
At our institution, we prefer to treat upper tracheal stenosis using hourglass-typed silicon stent. All procedures are performed in the bronchoscopy suite under general anesthesia. The appropriate size of hourglass-typed silicone stent is determined by measuring the length and diameter of the lesion using preoperative computed tomography. A silicone chip (about 6 mm in length) is made by utilizing the residual silicone stent fragment. A round tip needle is used to drill three holes in the chip. Then a polypropylene suture passes through those holes to tie the chip as shown in Figure 1. The patient is then inserted with a rigid bronchoscope. After the initial bronchoscopic interventions including balloon dilatation, electrocautery, laser therapy or cryotherapy, the stenosis is mechanically dilated by rigid bronchoscope of increasing diameters. Then a silicone stent is inserted through the opening of the bronchoscope into the area of stenosis by a prosthesis pusher. Once the finally ideal position of the stent is determined, the anterior neck between the second and third tracheal cartilage is prepared and draped in usual sterile manner. A 16-gauge intravenous angiocatheter is inserted through skin, subcutaneous tissue, anterior tracheal wall, and the anterior wall of silicone stent. The inner-stylet is removed, and the catheter sheath is left in place inside the stent lumen. The two free ends of the suture tying the chip are inserted through rigid bronchoscope by endoscopic biopsy forceps. Simultaneously, a thinner biopsy forceps inserts through the catheter sheath and grasps the two ends of suture out the catheter sheath one after another. Once secured, the catheter sheath is removed. Meanwhile, the two ends of suture are both pulled taut and then the chip is pulled closely against stent. Finally, the free ends of the suture are passed through a Nylon button placed snugly to the skin surface of anterior neck, which results in a secure fixation of the stent. The technique is fully described in Figures 2,3. After overnight postoperatively observation, the patient’s follow-up visit is carried out in 2 weeks and then monthly if needed.

Case presentation
Case 1
A 44-year-old female patient with a history of endotracheal intubation after cardiac surgery was admitted due to increasing dyspnea. The flexible bronchoscope revealed cicatricial stenosis in the upper trachea and an hourglass-typed silicone stent was inserted to the lesion in July 2014. The distance between the vocal cords and the upper end of the silicone stent was 20 mm. However, migration of the stent was found 7 months after the initial stenting. Then the stent was re-inserted and externally fixed by above-mentioned method. The patient had been followed up for 29 months and the stent had remained in place.
Case 2
A 25-year-old male patient had a history of endotracheal intubation, tracheotomy and placement of a Montgomery T-tube following acute pancreatitis. The T-tube was placed 10 months previously due to scar-granulation tissue in the upper trachea. In June 2015, the T-tube was removed via the tracheotomy site, and a silicone stent was inserted with 5 mm distant from the vocal cords to the upper end of the stent. However, stent migration was found during bronchoscopic reexamination on the fifth postoperative day and then external fixation was performed after readjustment of the stent. No stent migration occurred since. Moreover, the patient underwent replacement of silicone stents twice, in November 2016 and August 2017, respectively. The stent removal was uneventful by simply cutting the suture in the button. Figure 4 showed the external button sutured in place after the fixation method used during the patient’s follow-up visit.

Case 3
A 47-year-old male patient had carried a metal tracheal tube after tracheotomy for the past 5 years. With increasing dyspnea, he was found to have upper cicatricial stenosis via flexible bronchoscopy. After bronchoscopic interventions, a silicone stent was inserted with a 10-mm distance from the vocal cords to the upper end of the stent but distal migration of the stent was noted 7 days later. Therefore, external fixation of the stent was performed in May 2015. After stent removal in December 2015, the symptom of dyspnea reoccurred on the tenth day. Therefore, a new silicone stent was inserted and sutured into place in March 2016. Twelve months after the procedure, the patient was hospitalized with severe dyspnea. The bronchoscopy revealed that stent was in place but abundant granulation tissue grown between the vocal cords and the upper end of stent. After cleaning of granulation tissue, the patient lost consciousness due to low blood oxygen saturation level. An urgent endotracheal intubation, temporary tracheotomy and stent removal were performed. Three days later, the patient was discharged with a metal tracheal tube.
Discussion
Patients with severe upper tracheal stenosis from both benign and malignant lesions have severe symptoms such as dyspnea, stridor, obstructive pneumonia, and even respiratory failure. Surgical resection and reconstruction is indicated as the best treatment for the management of tracheal stenosis (4). However, management of upper stenosis is particularly challenging because surgical resection is often difficult to perform without a relatively free subglottic operational space and poor general conditions make some patients ineligible for surgery. Fortunately, bronchoscopic interventions may provide a well-accepted alternative for immediate and durable symptom relief and improvement of quality of life (2,4). The tracheal stenting is an attractive treatment option that preserves vocal cords’ function and improves respiratory symptoms (5). Metal and silicone stents are two main types of stents currently used in practice. The primary advantage of silicone stent is that it can be easily removed and exchanged. Also, silicone stent provokes no or minimal granulation tissue formation as compared to metal stent. Finally, silicone stent is inexpensive and can be easily customized on-site with cutting or combining as to fit the complex airway conditions (8). The major criticisms of silicone stent are the requirement for rigid bronchoscopy and general anesthesia, reduction in inner airway diameter, and potential complications including granulation tissue formation, stent migration and mucus plugging (3,6). The straight-typed or hourglass-typed silicone stent, a silicone tube, is well established for treatment of upper tracheal stenosis. However, the problem of stent migration can be particularly prominent.
Several fixation methods for upper tracheal stents have previously been reported to alleviate this complication. Some authors introduce special apparatus such as Bodkin threader, loop fixture or Endo Close, and Berci needle (9-12). Dhooria et al. (13) and Mehta et al. (14) both described an external fixation using routinely available devices. However, those methods are technically complex and require two puncture sites through the anterior trachea and silicone stent which may carry a risk of laceration of the stent when externally tying sutures. An internal fixation to anchor a silicone stent in a patient with upper tracheal stenosis is also reported (15). However, if the stent is required to be removed, it could be potentially complex because the sutures are hided in subcutaneous tissue.
We describe a simple external fixation method, not reported before, in order to facilitate the placement of silicone stent. Primarily, our method requires only one puncture site, which results in a more convenient procedure for bronchoscopist is to perform, a more comfortable experience for patients and accordingly a lower risk of tearing silicone stent. So far there are no reported studies of breaking silicone stent resulting from sutures dragging on two puncture sites. However, the puncture needle is relatively bland and forcibly inserting it through silicone stent may cause rough defect even cracks in the stent. Thus, it is more likely to tear silicone stent because of sutures rubbing two puncture sites during neck movement. Secondly, to fix stent using one puncture site, we specially design a silicon chip as an anchoring device by utilizing the redundant silicone fragment, which is matched with the shape of silicone stent. A similar method is reported by Musani et al. (16) to fix silicone stent; however, it requires special equipment as anchor device, a percutaneous endoscopic gastrostomy tube fastener which needs a water proof dressing to cover the external portion when patients taking shower. Lastly, all equipment and materials including silicone chip needed in our method are commonly available in bronchoscopy suite. So the method is applicable to urgent situation for fixing silicone stent, especially in the bronchoscopy suite equipped with no special apparatus.
The current study reported 3 consecutive patients with upper tracheal stent migration and then the initial stent placement using the introduced external fixation. The patients were monitored for over 20 months after the intervention, and no spontaneous stent migration or subcutaneous infection occurred. Meanwhile, we observed that 2 patients were successfully managed with removing the stent by cutting the suture in the button. It should be pointed out that the patient of the third case was hospitalized for the last time because of granulation tissue formation which was more likely resulted from the silicon stent and not the silicone chip. Our experience of three cases suggests that our new method can overcome stent migration and successfully treat upper tracheal stenosis without technical difficulties. Symptoms can be improved and quality of life is maintained, although granulation tissue formation requires repeat bronchoscopic interventions.
A potential problem of this method is that the silicon chip may be a foreign body aspiration in the event of suture breakage. At present, the case has not occurred in the long follow-ups for three patients. In considering of the potential complication before performing the method, we specially adopt polypropylene non-absorbable surgical suture with greater tensile strength and more tissue compatibility. Another issue is that the chip decreases the inner diameter of stent and may serve as a nidus for mucus plugging. However, with regular reexamination of bronchoscopy, the potential complication could be easily managed.
In summarize, silicone stenting is an attractive treatment option for patients with upper tracheal stenosis. However, stent migration is a major complication of silicone stent placement. We introduce a novel simple external fixation of silicone stent which may help prevent stent migration. This method has been performed in three patients until now at our institution, and we believe it should be considered to become a part of silicone stent placement due to its feasibility and convenience.
Acknowledgements
Funding: This work was supported by the National Nature Science Foundation of China (81270131 to C Chen, 81770074 to C Chen, 81570075 to C Chen); the Natural Science Foundation of Zhejiang Province (LZ15H010001 to C Chen); the Science Technology Department Foundation of Zhejiang Province (WKJ-ZJ-1526 to C Chen); National Key R&D Program of China (2016YFC1304000 to C Chen); the Interventional Pulmonology Key Laboratory of Wenzhou City to C Chen; and the Interventional Pulmonology Innovation Subject of Zhejiang Province to C Chen.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for patients for publication of manuscript and any accompanying images.
References
- Semaan R, Yarmus L. Rigid bronchoscopy and silicone stents in the management of central airway obstruction. J Thorac Dis 2015;7:S352-62. [PubMed]
- Wood DE, Liu YH, Vallieres E, et al. Airway stenting for malignant and benign tracheobronchial stenosis. Ann Thorac Surg 2003;76:167-72; discussion 173-4. [Crossref] [PubMed]
- Chin CS, Litle V, Yun J, et al. Airway stents. Ann Thorac Surg 2008;85:S792-6. [Crossref] [PubMed]
- Ernst A, Feller-Kopman D, Becker HD, et al. Central airway obstruction. Am J Respir Crit Care Med 2004;169:1278-97. [Crossref] [PubMed]
- Ranu H, Madden BP. Endobronchial stenting in the management of large airway pathology. Postgrad Med J 2009;85:682-7. [Crossref] [PubMed]
- Saito Y. Endobronchial stents: past, present, and future. Semin Respir Crit Care Med 2004;25:375-80. [Crossref] [PubMed]
- Lin X, Ye M, Li Y, et al. Bronchoscopic video of the fixation method used. Asvide 2018;5:380. Available online: http://www.asvide.com/article/view/23854
- Breen DP, Dutau H. On-site customization of silicone stents: towards optimal palliation of complex airway conditions. Respiration 2009;77:447-53. [Crossref] [PubMed]
- Colt HG, Harrell J, Neuman TR, et al. External fixation of subglottic tracheal stents. Chest 1994;105:1653-7. [Crossref] [PubMed]
- Miwa K, Takamori S, Hayashi A, et al. Fixation of silicone stents in the subglottic trachea: preventing stent migration using a fixation apparatus. Ann Thorac Surg 2004;78:2188-90. [Crossref] [PubMed]
- Majid A, Fernandez-Bussy S, Kent M, et al. External fixation of proximal tracheal airway stents: a modified technique. Ann Thorac Surg 2012;93:e167-9. [Crossref] [PubMed]
- Hohenforst-Schmidt W, Linsmeier B, Zarogoulidis P, et al. Transtracheal single-point stent fixation in posttracheotomy tracheomalacia under cone-beam computer tomography guidance by transmural suturing with the Berci needle - a perspective on a new tool to avoid stent migration of Dumon stents. Ther Clin Risk Manag 2015;11:837-50. [PubMed]
- Dhooria S, Agarwal R. External fixation of a subglottic tracheal silicone stent. Ann Am Thorac Soc 2014;11:467-8. [Crossref] [PubMed]
- Mehta RM, Singla A, Shah A, et al. The "Hitch Stitch": An Effective Method of Preventing Migration in High Tracheal Stenosis. Respiration 2017;93:106-11. [Crossref] [PubMed]
- Temes RT, Wernly JA, Cooper JD, et al. Internal fixation of high tracheal stents. Ann Thorac Surg 1995;59:1023-4. [Crossref] [PubMed]
- Musani AI, Jensen K, Mitchell JD, et al. Novel use of a percutaneous endoscopic gastrostomy tube fastener for securing silicone tracheal stents in patients with benign proximal airway obstruction. J Bronchology Interv Pulmonol 2012;19:121-5. [Crossref] [PubMed]