Pacific trial: a new ocean or an abnormal wave?
Recently, Antonia et al. (1) have published a phase III randomized trial exploring durvalumab after concurrent chemoradiotherapy (CRT) in stage III non-small cell lung cancer (NSCLC). The study reported results on progression free-survival (co-primary end-point with overall survival) with a benefit of the addition of durvalumab to chemoradiation. The median progression-free survival (PFS) improved from 5.6 months with placebo to 16.8 months with durvalumab (HR: 0.52; 95% CI: 0.42–0.65). These are the first positive results in stage III disease after those negative of high dose radiotherapy (2) or the inclusion of new drugs (2,3). Table 1 summarizes results according to PFS for these trials.

Full table
Looking to the control arm, median PFS in this study (5.6 months) is quite lower than in RTOG 0617 (11.8 months) or in PROCLAIM trial (9.8 months).
Thus, how can we explain this halved survival of standard arm?
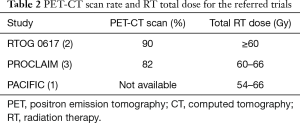
First of all, approximately 2 months should be explained by the time of randomization (before CRT in RTOG 0617 and PROCLAIM versus end of CRT as in PACIFIC). But, main differences among these studies are the inclusion of PET-CT in up-front staging, and delivery of radiation therapy (RT). Both PROCLAIM and RTOG 0617 recorded 82% and 90% respectively of patients who received a staging by positron emission tomography (PET)/computed tomography (CT) scan, while data are not available in PACIFIC trial, probably due to the enrollment and patients’ randomization after CRT completion. Moreover, total RT dose is quite different, because in PACIFIC trial patients received a dose range between 54 and 66 Gy while in RTOG 0617 and PACIFIC trial the minimum dose was 60 Gy. And we all know that 54 Gy is substantially different from 60–66 Gy (Table 2).
Full table
Thus, which results would be reported if up-front PET-CT along with right RT total dose have been adopted? Moreover, is durvalumab a justified expensive therapy or just a financially toxic one’s if compared with the best standard of care in treating stage III NSCLC?
Waiting for the final results on survival, these issues should be taken into account, even if median PFS of 16.8 months with durvalumab is a step forward when compared to about 12 months of the best arm in RTOG 0617 or PROCLAIM trials.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Antonia SJ, Villegas A, Daniel D, et al. Durvalumab after chemoradiotherapy in stage III non-small cell lung cancer. N Engl J Med 2017;377:1919-29. [Crossref] [PubMed]
- Bradley JD, Paulus R, Komaki R, et al. Standard-dose versus high-dose conformal radiotherapy with concurrent and consolidation carboplatin plus paclitaxel with or without cetuximab for patients with stage IIIA or IIIB non-small cell lung cancer (RTOG 0617): a randomised, two-by-two factorial phase 3 study. Lancet Oncol 2015;16:187-99. [Crossref] [PubMed]
- Senan S, Brade A, Wang LH, et al. PROCLAIM: PROCLAIM: Randomized Phase III Trial of Pemetrexed-Cisplatin or Etoposide-Cisplatin Plus Thoracic Radiation Therapy Followed by Consolidation Chemotherapy in Locally Advanced Nonsquamous Non-Small-Cell Lung Cancer. J Clin Oncol 2016;34:953-62. [Crossref] [PubMed]


