Cerebral oximetry in cardiac anesthesia
Introduction
Intraoperative measurement of tissue oxygenation in regions of various organs was restricted until recently, and the available techniques were applied mainly in Intensive Care or for research. Gastrointestinal tonometry for early recognition of dysoxic states (1), flexible polarographic Clark-type microcatheter for brain tissue PO2 monitoring (2), jugular fiber oxymetry for SjVO2 measurement (3), bolt catheters for monitoring of microdialysis parameters (4,5), and jugular polyoptode oximetry with miniaturized electrodes for continuous brain venous blood gas analysis (6), remained in low intraoperative application for a number of reasons. Time-consuming application, invasiveness, technical difficulties, unstable signaling and costs created reluctance among anesthesiologists for their adoption intraoperatively. As a result, the imbalance of oxygenation of regional character was more to be hypothesized than early detected as tissue oxygenation was estimated by measuring systemic arterial and venous oxygenation. However, ischemia not detectable at the systemic level is considered a major contributor to postoperative morbidity and mortality. To limit this gap, between recognition of problematic oxygenation in systemic and tissue level, non invasive techniques capable for continuous assessment of tissue oxygenation were introduced. Among them, the most promising and broadly spread technique is near-infrared spectroscopy (NIRS).
The principal behind the determination of regional hemoglobin oxygen saturation is the change of optical properties of hemoglobin when binding to oxygen and the consequent change of absorption pattern for specific light wavelengths. An analogous of NIRS based oximetry is pulse oximetry. A number of measuring sites has been proposed for application of NIRS. Among them, the forehead is used as a site for assessing brain oxygenation. Furthermore, the thenar eminence, the forearm, the pectoral and deltoid muscle and the paravertebral region have been used for monitoring sites in various clinical and experimental settings of circulatory distress and hypovolemia or trauma (7-9). In neonates and infants, NIRS measurement of deeper organs like the kidney or the intestines is feasible due to their superficial location (10,11).
NIRS-based cerebral oximetry permits early detection of cerebral hypoxia and guides therapy to restore it. A number of devices are commercially available, having clearance by United States Food and Drug Administration for use as monitors of brain oxygenation. As neurological outcome remains problematic in cardiac and vascular surgery, many anesthesiologists working in these fields adopted their use for having continuous information about the status of brain perfusion.
Technical background—validation
Cerebral oximeters determine regional hemoglobin oxygen saturation (rSO2) in the frontal lobes by using specially designed probes. These probes comprise adhesive pads containing diodes (LED) or laser light sources which emit photons in the NIR spectrum capable of tissue penetration of several centimeters through the cranial bone to the underlying cerebral tissue. This light is partly reflected, partly redirected, scattered and absorbed. Contact with hemoglobin molecules results in a change of light spectrum depending on the oxygenation status of hemoglobin. A fraction of this resultant light returns towards the surface and is captured by detectors embedded to the adhesive pads. After this banana-shaped course of the light, from the emitter to the detector, the monitor differentiates the two forms of oxygenated and deoxygenated hemoglobin using specific computational algorithms in order to determine the rSO2 in the frontal lobes. Venus weighted blood saturation reflecting changes in cerebral oxygen demand/supply ratio is measured at a depth of about 1.5 cm. Existing devices incorporate similar technology but with differences in the number and absolute value of wavelengths and in the computational algorithms. Detailed presentations of the technical background of NIRS can be found in recent literature (7,12).
A first step for the evaluation of any new monitoring device requires comparison with existing monitors. Validation studies of NIRS-based cerebral oximetry have been performed with researchers seeking for correlations of rSO2 with other indexes of cerebral oxygenation such as regional brain-tissue partial pressure of oxygen (i.e., tiPO2) and SjVO2. However, it is clear that both these parameters are not the same as rSO2. The direct, invasive measurement of tiPO2 comes from white matter and SjVO2 value represents the oxygen demand/supply ratio of both grey and white matter, where considerable differences of flow and oxygen consumption exist. In some degree, SjVO2 value may be “polluted” by arteriovenous communications or/and by extracranial venous blood through venous tributaries near jugular bulb. Moreover, jugular fiber oximetry measures not only the saturation of venous blood which comes from the ipsilateral hemisphere to the one from which rSO2 values are taken for comparison but it measures also a significant quantity of venous blood coming from the contralateral side. For these reasons absolute, direct correlations of rSO2 to tiPO2 and SjVO2 cannot be expected to exist. Regional oxygenation in the cerebral microvasculature appears as a totally new monitored variable. Furthermore, inhomogenous distribution of ischemic areas instead of diffuse brain lesion may result poor correlations in studies including patients with head injury. However, a number of human clinical and experimental studies have shown that rSO2 traces very satisfactory these two different and distinct indexes of cerebral oxygenation (2,13-15).
A second step for the evaluation of a monitor is to determine its reliability, accuracy and clinical utility. Is NIRS-based cerebral oximetry a technology that has potential to contribute to the management of patients? After the early evaluation with comparisons to same or similar biological parameters taken from other devices in laboratory and clinical situations, a new monitor must enlighten more a patient’s clinical condition in order to improve outcome. In the past, studies of pulse oximetry and pulmonary artery catheters were in great difficulty to demonstrate the effect of monitoring of these parameters on changing outcomes (16,17). The fact that, in cardiac surgery cerebral oximetry is used, in most of the cases, together with these two modalities makes its effect to outcome particularly difficult to be shown. However, as it will be discussed later, there are data supporting that correction or improvement of low rSO2 values affect positively the outcome.
Monitoring
Cerebral oximetry measures regional tissue saturation in an area of frontal cortex of approximately 1 cm3. RSO2 values are affected by the physiologic variables that determine brain oxygen supply and demand. Alterations in most of these variables result in a more or less symmetrical effect on rSO2. Nevertheless, some of the variables listed below, such as procedure-related variables especially in patients with anatomic asymmetries in their brain circulation, may affect more one of the hemispheres. Oxygen delivery to the brain depends on cerebral blood flow and oxygen content and hence cardiac output, hemoglobin concentration, pulmonary function, inspired oxygen concentration and hemoglobin saturation primarily affect rSO2. Intraoperative events of acute character such as cardiovascular collapse, hemorrhage, intraoperative myocardial infarction and hypoxemia are examples of situations where cerebral oximetry values may be affected. Mechanical perturbation of any kind affecting arterial inflow or venous outflow such as occlusion or compression, embolic events, and acute hematoma formation may affect rSO2 values. Perturbation affecting rSO2 values in cardiovascular surgery may include iatrogenic clamping or dissection, and malposition of arterial perfusion cannula or intra-aortic balloon pump. Brain’s oxygen consumption is related to cerebral metabolism and cerebral temperature, variables that significantly alter in the course of a cardiac operation. Acid-base status and PaCO2 affect not only the hemoglobin saturation for a given PO2 but also cerebral blood flow. Cerebral oximetry values must be monitored bilaterally as pre-existing tissue dysfunction, past cerebral infarction, significant carotid stenosis, incomplete circle of Willis, or mechanical perturbation, or procedure-related factors (e.g., unilateral and bilateral antegrade cerebral perfusion during surgery of the aorta) may affect oxygenation/perfusion of each hemisphere in a different way. The interpretation of rSO2 values must be based on all available clinical information. In this way, rSO2 values provide a more detailed picture for brain’s regional oxygenation and, at the same time, give the opportunity to the clinician to use brain as an index organ for the adequacy of perfusion of other vital organs.
Normal rSO2 values, prior to the induction of general anesthesia, range from 60% to 80%. Although lower values (55-60%) for cardiac surgery patients breathing room air are not considered atypical, in our opinion these patients deserve a higher degree of attention. Besides cerebral oxygenation, baseline cerebral oximetry values reflect a patient’s overall cardiopulmonary function and systemic oxygen needs. Cerebral oximetry values were found low in patients with normotensive acute heart failure (18). Successful treatment increased rSO2 values. In this study, a fatal myocardial infarction was accompanied with rSO2 of 18% before leading to death. In another study, the correlation between rSO2 values and cardiac function was assessed after anesthetic induction. RSO2 values were significantly correlated to hemodynamic and echographic parameters and superior at predicting left ventricular dysfunction (19). In another study, during implantation of cardioverters/defibrillators it was found that severely compromised left ventricular pump function was associated with diminished rSO2 (20). In another study including 344 patients with coronary artery disease who performed cardiopulmonary exercise testing, rSO2 values were continuously monitored and cardiac deaths and cardiovascular events were recorded for a follow-up period of more than three years (21). The change of cerebral oximetry values from rest to peak exercise was significantly lower in non-survivors than in survivors and this change together with left ventricular ejection fraction was found to be independent prognostic marker for cardiac deaths. A number of studies demonstrated good correlations of rSO2 and SvO2 or central venous oxygen saturation (ScvO2). These results were from awake, spontaneously breathing adult patients after cardiac surgery (22), in cases of prolonged cardiopulmonary resuscitation (23), in varying hemodynamic conditions during transapical transcatheter aortic valve implantation (24), in patients requiring temporary circulatory support by extracorporeal membrane oxygenation due to refractory cardiogenic shock (25) and in pediatric patients (26). The correlation between rSO2 and SvO2 exists also during tepid hypothermia but in moderate hypothermia it becomes poorer (27).
The previously mentioned studies demonstrate a strong agreement between rSO2 and SvO2 under varying hemodynamic conditions, from a stable situation to a significantly challenged one in subjects with different degrees of reserve. In many of these observations SvO2 was primarily affected by changes in cardiac output and oxygen consumption, with the effect of some change in arterial oxygen content (i.e., hypoxemia, anemia) to be minimal or even absent. It is known that cerebral metabolic rate is coupled to oxygen delivery. Cerebral blood flow is modulated in the presence of decreased oxygen delivery due to decreased arterial oxygen content. In this case, this mechanism of cerebral autoregulation maintains cerebral oxygen delivery by proportionate increases in cerebral blood flow. In case of stable arterial oxygen content, decreases in rSO2 reflect an increased oxygen extraction ratio and are indicative of a relative decrease in cerebral perfusion. A diversion of flow towards the central compartment is apparent during circulatory distress, to maintain perfusion/oxygenation of vital organs. In this case and due to physiologic mechanisms preserving cerebral blood flow at the expense of relative systemic hypoperfusion, the presence of low rSO2 may thus reflect significant systemic circulatory compromise (28). The NIRS-monitored brain becomes an index organ where, beyond alterations of local factors, alone or in combination, derangements of systemic factors are reflected also. In this case, NIRS may detect states of regional tissue hypoperfusion, even when blood pressure is still within the normal range. Actually, the changing status of rSO2 values has to be interpreted in the context of all available clinical information because it is relatively nonspecific.
A substantial literature now evidences the potential clinical benefit of NIRS-based thenar or cerebral oximetry in a wide range of areas and situations including resuscitation in shock and cardiac arrest, prehospital medicine including transportation of trauma or other critically ill patients, admission to the emergency area, various kinds of elective and urgent cardiac and non-cardiac surgical operations, and during intensive care of critically ill patients (7,23,29-36). These published studies strongly suggest that NIRS monitoring provides a measurable clinical benefit to patients under various conditions.
Clinical use in cardiac surgery
NIRS-based cerebral oximetry is increasingly in use in the field of cardiac anesthesia. It has been adopted in a large scale by anesthesiologists for monitoring during adult and pediatric cardiothoracic and vascular operations. It provides clinicians unique information allowing them to make clinical decisions that will positively affect outcome. Neurological outcome is still problematic in these operations. The incidence of stroke, ranges from 1% to 3% in coronary artery bypass grafting and may be substantially higher in aortic surgery. Although a number of technical improvements, surgical modifications, and various other recommendations for management have been proposed and, in a degree, adopted (37), a significant percentage of strokes occur among patients at low or medium preoperative risk, suggesting that many of these strokes may be preventable by adequate monitoring. Furthermore, other causes of peri-operative morbidity and mortality are also present, associated to patient’s history and underlying illness and to the demands of the procedure. Presently, cerebral oximetry in cardiac surgery has proven its utility for preoperative risk stratification, for alerting during less-common intraoperative events, for supporting decisions and for guiding physiologic interventions.
Preoperative risk stratification
In a large prospective study, including 1,178 patients undergoing various elective, urgent and emergency on-pump cardiac operations, preoperative rSO2 measurements along with other patient- and procedure-related risk factors were evaluated for their ability to stratify risk (38). Cerebral oximetry measurements were taken the day before surgery and mean minimal values without (rSO2min) and with supplemented oxygen (rSO2mean-ox) were correlated to clinical outcomes such as 30-day and 1-yr mortality and major morbidity. As expected, patients in the cohort with older age, ventricular failure, renal dysfunction, anemia, need for circulatory support, and need for emergency surgery showed worse outcome by experiencing morbidity or not surviving. Low rSO2mean-ox was significantly correlated with ejection fraction <30%, impaired renal function, anemia, elevated N-terminal pro-B-type natriuretic peptide and high-sensitivity troponin T levels. Patients who failed to increase rSO2 beyond a cut-off value of approximately 50% while breathing supplemented oxygen showed significantly higher 30-day morbidity and mortality compared to oxygen responders. Baseline cerebral oxygen saturation was connected to outcome as an independent risk factor. Furthermore, in the highest risk subgroup of patients with an additive EuroSCORE more than ten, it was found that baseline rSO2 <50% was a more accurate predictor of 30-day mortality than the EuroSCORE.
These results indicate that the presence of low preoperative cerebral oximetry values may reflect significant systemic circulatory compromise (28). Patients failing to increase rSO2 while breathing supplemented oxygen are near the limits of the physiologic mechanisms for preserving cerebral blood flow. Preoperative cerebral oximetry may alert for significant systemic circulatory compromise and is of additive value to other risk stratification methods as the EuroSCORE or the STS Score. These systems have gained wide acceptance and are continuously improving (39-41). They have an influence on how to decide that certain patients should not be considered surgical candidates because of the high risk, or on the selection of type of surgery and the preoperative preparation and planning (42). If some combination with cerebral oximetry makes a scoring system more accurate remains to be clarified. Decisions concerning patient selection, for example as which patient will benefit more with traditional aortic valve replacement or transcatheter aortic valve implantation, or medical therapy, may be partly based on cerebral oximetry (43). Whether preoperative optimization of cerebral oxygenation by optimizing oxygen content and/or hemodynamic status could reduce the postoperative risk need to be subjected to further studies.
In a substudy including 231 consecutive patients of the previous population, the same team of investigators determined the relationship between preoperative rSO2 levels and postoperative delirium (44). Delirium was assessed on each of the first three days after surgery and was correlated to patient- and surgery-related factors including preoperative cognitive function. The study reconfirmed the known role of old age, altered cognitive function, and neurological or psychiatric disease as risk factors for postoperative delirium. Beyond this, lower preoperative rSO2 values were identified as independent risk factor for delirium. Similar findings concerning rSO2 were observed in a small cohort of non-cardiac surgical patients by other investigators (45). It is worth to note that in both the previously mentioned studies (38,44) cerebral oximetry was part of the routine monitoring, and patients presenting low rSO2 values intraoperatively were managed with corrective interventions.
Outcome without cerebral oximetry-based interventions
In an observational study of cardiac surgery patients treated with no NIS-based interventions, low intraoperative rSO2 values were significantly correlated to the postoperative impairments in cognitive function (46). The incidence of impairment for both the two neuropsychological tests used in the study was higher in those patients with either a nadir rSO2 below 35% or with rSO2 values below 40% for more than 10 min. Similar findings were reported for early and late neurocognitive evaluation in 61 elderly patients (47). In another study of also observational character, including 30 patients undergoing aortic arch surgery, spending more than 30 minutes under the absolute threshold of 60% was associated with complications, extended hospital stay, and additional cost (48). These studies, although useful to clarify the impact of intraoperative cerebral desaturations on outcome, leave unknown whether interventions to increase rSO2 would have averted complications and adverse outcomes.
Impact of intraoperative cerebral oximetry on outcome
The true value of a monitor is linked firstly to the amount of decisions, interventions, and corrective measures that are based on it, and secondly to the improvement on outcome that these create. As it was mentioned earlier, the effect of cerebral oximetry on outcome in cardiac operations is particularly difficult to be shown due to many reasons. Besides procedural complexity and equipment involvement affecting outcome by themselves, a number of other monitoring modalities are used as standards and the impact of a new monitor is not traceable in small populations. So, criticism is unavoidable for the value of cerebral oximetry in cardiac surgery (43,49). At the initiation of by-pass however, the response of pulse oximetry and/or SvO2 monitoring in a case of mistakenly turned off oxygen in gas mixer is limited due to absence of pulse (for pulse oximetry) and venous return to the machine (for SvO2 readings). If no other monitoring devices (i.e., NIRS-based oximetry) are implemented, the color of the blood in the field is the only warning for the complications which are about to follow.
During anesthesia, an absolute rSO2 value less than 50% or a greater than 20% drop from individual baseline rSO2 is commonly considered as intervention trigger. Attending anesthesiologists are using NIRS monitoring to intervene for the benefit of the patient. During cardiac surgery, the incidence of desaturations in cerebral oximetry is high, especially in pediatric patients and in aortic surgery (48,50,51). A number of trials have been conducted examining the impact on outcome after treatment based on rSO2 monitoring in cardiac surgical patients. In a study involving more than 2,000 patients undergoing cardiac operations the incidence of stroke was assessed in two groups (52). In the treatment group, NIRS-based cerebral oxygen monitoring was used to optimize oxygen delivery and consumption variables to maintain oximetry values at or near the patient’s preinduction values. For this, a standardized interventional protocol was used. In the other group cerebral oximetry was not applied. The patients in the rSO2 monitoring group showed significantly lower incidence of stroke (0.97% rSO2 group vs. 2.5% control), incidence of prolonged postoperative mechanical ventilation time (6.8% rSO2 group vs. 10.6% control) and length of postoperative hospital stay. The study showed that these differences in outcomes were found not among the sickest patients but among the New York Heart Association Class I patients. The high incidence of stroke among patients at low or medium preoperative risk during cardiac surgery has been reported by others also (53). These observations suggest that it is not just the sickest patients who benefit from the use of cerebral oximetry.
Another study examined two groups of patients that were both monitored with cerebral oximetry (54). In treatment group, the rSO2 results were open to the clinicians and a standardized intervention protocol was employed. Desaturations below 75% of the preoperative established baseline values were treated with a predetermined protocol designed to optimize PaCO2, cerebral perfusion pressure and pump flow. In case of persistent rSO2 below treatment threshold then FiO2 was increased, pulsatile perfusion was initiated, hypnotics were given, and, if needed, packed red cells were transfused. In the second group, the rSO2 data were blinded to clinicians. Patients in the control group had significantly greater desaturation values and longer intensive care unit stays compared to the patients in the active treatment group. Further, the composite outcome of death, myocardial infarction, stroke, postoperative ventilation greater than 48 hours and reoperation for hemorrhage was significantly higher in the control group than the observed in the treatment group. The study was not accompanied by an economic analysis. Independently, however, it was estimated that for the included patients direct hospital savings exceeded cerebral oxygen monitoring cost by a factor of ten (55).
Other investigators attempted to replicate the results of the prior study randomizing cardiac surgery patients to the same interventional protocol in response to low rSO2 values (56). In agreement, they observed that patients with intraoperatively declined rSO2 values exhibited significantly more severe postoperative cognitive decline and a higher incidence of prolonged hospital stay. In contrast to the previous study, the group with NIRS-guided interventions experienced the same magnitude of cognitive decline as the control group. However, the authors described poor intervention protocol compliance resulting in the same desaturation magnitude in the control and treatment groups.
As it has been discussed earlier, the intraoperative course of rSO2 values may be influenced by a number of factors. Irrespectively of rSO2 reflecting events related to the overall disease or not, the correction of an imbalance between cerebral oxygen supply and demand seems logical. Even mistakes can happen in the complexity of cardiac procedures, and, if not corrected, they can lead otherwise low risk patients to complications. Literature describes an association between low rSO2 values and worse outcome in cardiac surgery. In the previously mentioned “positive” for cerebral monitoring studies, the reversed low rSO2 values with the appropriate intervention directly represent a cause-effect relationship. Practically, proposed algorithms to treat low-rSO2 events (44,56-58) recommend head repositioning, correction of variables such as mean arterial pressure, hemoglobin saturation and concentration, cerebral metabolism, intracranial pressure, and optimization of cardiac performance (or pump flow on cardiopulmonary bypass). Controlling and optimizing PaCO2 is also of primary importance. Hypocapnia consistently decreases cerebral saturation (59). A methodical approach with first-line interventions, reevaluations and second-line interventions, and the interpretation of rSO2 values in the context of all available clinical information is necessary.
Cerebral oximetry supporting intraoperative decisions
There is a long list of case reports that highlight the utility of cerebral oximetry to alert clinicians to serious intraoperative events. In some instances, it prompted the clinician to investigate further. As monitoring parameters are usually interrelated, the monitors often function as an adjunct to each other. In these case reports cerebral oximetry was at that moment the sole indicator or it accompanied clinical signs or/and data from other monitoring devices. In the case that cerebral oximetry is able to detect uncommon events earlier than standard monitors its value becomes significant. But even if the change in rSO2 goes in parallel or even later to other findings, it integrates the picture and the significance of the situation, it shows the results to brain of the measures taken, and thus is still beneficial.
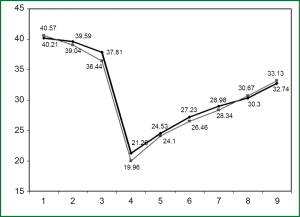
Decreased rSO2 values upon initiation of bypass were reported in a patient who had axillary artery cannulation (60). This alerted clinicians to proceed with ultrasound examination which confirmed the diagnosis of arterial air embolism from the insertion site of axillary cannula. After repairing cannulation, the surgical procedure was continued. Although the patient suffered only delirium requiring prolonged mechanical ventilation, no one can exclude severe postoperative complications and bad outcome in case that cerebral oximetry had not been in use. In another case of an off-pump left ventricular assist device implantation, the circulatory instability was tracked more promptly and sensitively by changes in rSO2 than by continuous cardiac output monitoring (61). The procedure involves many manipulations which may alter hemodynamics as collapsing the left lung, clamping descending aorta, traction of the pericardium, and maneuvers for implanting the device into the left ventricle. Cases have been reported where cerebral oximetry alerted the clinicians during malfunction of the superior vena cava cannula in a child (62), or during post-by-pass obstruction of superior vena cava in an adult (63). In the second case, after the fall in rSO2 values, it was discovered that the repair had partially obstructed the vein. However, it can be argued that when an event is accompanied by acute superior vena cava syndrome the value of cerebral oximetry in alerting is moderate. Information provided by newer monitoring technologies may be useful for decisions that concern issues not directly associated to the “primary” monitored variable. For example, a significant percentage of interventions based on bispectral index monitor may target not hypnotic state depth but other aspects of patient care (64). Having in mind that reducing blood product utilization is particularly important in cardiac surgery (65), we wondered if cerebral oximetry is of value for decisions extended to transfusions. In a study investigating the impact of perioperative intravenous fluid restriction on red blood cell transfusions in cardiac surgery under by-pass, we used NIRS-based cerebral oximetry as an adjunct tool to hematocrit for deciding about transfusion (66). The idea behind this was that, because the degree of hematocrit drop which is caused by hemodilution and by true red cell loss is clinically unclear in the course of such an operation, a blood transfusion may not be quite justifiable when there is a decrease in hematocrit values and, at the same time, rSO2 values are acceptable. The results of this investigation were favoring fluid restriction combined with the use of cerebral oximetry (Figure 1). To elucidate the impact of NIRS-monitoring alone on the amount of transfusions in cardiac surgery we conducted a prospective trial, comparing patients where transfusion was based on hematocrit criteria only and patients who were transfused under a NIRS-monitoring based protocol combined to hematocrit. Our results were in favor of NIRS-monitoring as a tool to avoid unnecessary blood transfusions (67).
Cerebral oximetry in aortic surgery
Aortic aneurysm surgery involving the aortic arch is still accompanied by a considerable incidence of neurological events. Interruption of flow to cerebral vessels remains an inherent risk in these operations. In avoiding cerebral ischemia different surgical approaches have been developed during the last decades. Lately, selected antegrade cerebral perfusion seems wide spreading. The technique allows perfusion via the right axillary artery with or without a combination of perfusion via a cannula inserted directly into the left common carotid artery, with left subclavian artery occluded with a Fogarty catheter, and is followed by a neurological injury rate of <5% (68-70). Bilateral perfusion allows longer times of circulatory arrest compared to unilateral perfusion without increasing the rate of permanent neurological disorders. On the other hand, however, manipulations of arch-vessel cannulation may increase the incidence of stroke. There has been steady adoption of NIRS-based cerebral oximetry as a routine use for these operations by the majority of high-volume centers in North America (71) and Western Europe. In a study comparing patients with and without neurological events after aortic surgery with selective cerebral perfusion it was found that operation time and duration of rSO2 drops were significantly longer when neurological events occurred. Sustained decreases in rSO2 were observed in patients with transient neurological events and hypoperfusion infarcts while not in patients with embolic infarcts (72). Similar results were reported for thoracic cardiovascular surgery with deep hypothermic circulatory arrest involving the aortic arch treated with selective antegrade perfusion (73). Another study including 51 patients, reported significant incidence of stroke equaling 18.1% in the 11 desaturated patients (rSO2 lower than 80% of baseline) versus 0% in the 40 patients of the no-desaturation group (74). In a series of 13 patients operated under moderate hypothermic arrest, the choice between uni- or bi-lateral antegrade cerebral perfusion was based on NIRS-monitoring, with a regimen including threshold of rSO2 drop <55% and/or drop of 15-20% below baseline (75). The need for institution of bi-lateral antegrade cerebral perfusion was not seen in only one patient (rSO2 drop from 70% to 60%). The in-hospital mortality was two patients and transient postoperative neurological delirium occurred in three patients (23%). In another case of aortic arch replacement due to acute dissection, rapid decrease in rSO2 values prompted for inadequate antegrade cerebral perfusion by the innominate artery cannulation (76). The decision to directly cannulate left carotid artery to restore cerebral blood flow was based on cerebral oximetry, which also allowed assessment of this measure. This strategy resulted in a good neurological outcome for the patient. Yet, these reports are of somehow observational character providing limited clinical data about the value of cerebral oximetry on decision-making. During aortic surgery clinicians consider rSO2 monitoring as a standard and apply proposed algorithms to treat low-rSO2 events (44,56-58). Hence, it may be considered of problematic ethical level to suggest blinded prospective studies for the assessment of the impact of cerebral oximetry on outcome.
Conclusions
NIRS-based cerebral oximetry contributes to the management of patients undergoing cardiac surgery. It is simple, non-invasive and reliable, and its regular use is adopted by cardiovascular anesthesiologists in a large scale. Its perioperative use is accompanied by multiple literature of supportive character. It is of value for preoperative risk stratification recognizing patients with limited organ functional reserve, it provides online intraoperative insight into regional oxygenation of brain, it serves as a first-alert indicator of intraoperative events potentially affecting outcome adversely, and it positions the brain in a place of indexing organ which reflects the adequacy of tissue perfusion and oxygenation of other vital organs. Obtaining adequate tissue oxygenation with cerebral oximetry may prevent complications which could result from tissue hypoxia undetected by conventional invasive hemodynamic monitoring. Interventions to treat rSO2 desaturations are associated with less major organ injury and shorter intensive care unit hospitalization. Future research, generating higher-level evidence, may expand the use of this promising monitoring modality to the place of standard monitor in cardiac surgery.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Gutierrez G, Taylor D. Gastrointestinal tonometry: basic principles and recent advances in monitoring regional CO2 metabolism. Semin Respir Crit Care Med 1999;20:17-27.
- Brawanski A, Faltermeier R, Rothoerl RD, et al. Comparison of near-infrared spectroscopy and tissue p(O2) time series in patients after severe head injury and aneurysmal subarachnoid hemorrhage. J Cereb Blood Flow Metab 2002;22:605-11. [PubMed]
- Vigué B, Ract C, Benayed M, et al. Early SjvO2 monitoring in patients with severe brain trauma. Intensive Care Med 1999;25:445-51. [PubMed]
- Paraforou T, Paterakis K, Fountas K, et al. Cerebral perfusion pressure, microdialysis biochemistry and clinical outcome in patients with traumatic brain injury. BMC Res Notes 2011;4:540. [PubMed]
- Rao GS, Durga P. Changing trends in monitoring brain ischemia: from intracranial pressure to cerebral oximetry. Curr Opin Anaesthesiol 2011;24:487-94. [PubMed]
- Vretzakis G, Papadimitriou D, Koutsias S, et al. Continuous contralateral jugular acid-base and blood gas monitoring during carotid endarterectomy. Vasa 2000;29:221-4. [PubMed]
- Scheeren TW, Schober P, Schwarte LA. Monitoring tissue oxygenation by near infrared spectroscopy (NIRS): background and current applications. J Clin Monit Comput 2012;26:279-87. [PubMed]
- Bartels SA, Bezemer R, de Vries FJ, et al. Multi-site and multi-depth near-infrared spectroscopy in a model of simulated (central) hypovolemia: lower body negative pressure. Intensive Care Med 2011;37:671-7. [PubMed]
- Soller BR, Ryan KL, Rickards CA, et al. Oxygen saturation determined from deep muscle, not thenar tissue, is an early indicator of central hypovolemia in humans. Crit Care Med 2008;36:176-82. [PubMed]
- Danduran MJ, Dixon JE, Rao RP. Near infrared spectroscopy describes physiologic payback associated with excess postexercise Oxygen consumption in healthy controls and children with complex congenital heart disease. Pediatr Cardiol 2012;33:95-102. [PubMed]
- Kaufman J, Almodovar MC, Zuk J, et al. Correlation of abdominal site near-infrared spectroscopy with gastric tonometry in infants following surgery for congenital heart disease. Pediatr Crit Care Med 2008;9:62-8. [PubMed]
- Pellicer A, Bravo Mdel C. Near-infrared spectroscopy: a methodology-focused review. Semin Fetal Neonatal Med 2011;16:42-9. [PubMed]
- Holzschuh M, Woertgen C, Metz C, et al. Dynamic changes of cerebral oxygenation measured by brain tissue oxygen pressure and near infrared spectroscopy. Neurol Res 1997;19:246-8. [PubMed]
- Kim MB, Ward DS, Cartwright CR, et al. Estimation of jugular venous O2 saturation from cerebral oximetry or arterial O2 saturation during isocapnic hypoxia. J Clin Monit Comput 2000;16:191-9. [PubMed]
- Mcleod AD, Igielman F, Elwell C, et al. Measuring cerebral oxygenation during normobaric hyperoxia: a comparison of tissue microprobes, near-infrared spectroscopy, and jugular venous oximetry in head injury. Anesth Analg 2003;97:851-6. [PubMed]
- Connors AF Jr, Speroff T, Dawson NV, et al. The effectiveness of right heart catheterization in the initial care of critically ill patients. SUPPORT Investigators. JAMA 1996;276:889-97. [PubMed]
- Moller JT, Johannessen NW, Espersen K, et al. Randomized evaluation of pulse oximetry in 20,802 patients: II. Perioperative events and postoperative complications. Anesthesiology 1993;78:445-53. [PubMed]
- Madsen PL, Nielsen HB, Christiansen P. Well-being and cerebral oxygen saturation during acute heart failure in humans. Clin Physiol 2000;20:158-64. [PubMed]
- Paquet C, Deschamps A, Denault AY, et al. Baseline regional cerebral oxygen saturation correlates with left ventricular systolic and diastolic function. J Cardiothorac Vasc Anesth 2008;22:840-6. [PubMed]
- Skhirtladze K, Birkenberg B, Mora B, et al. Cerebral desaturation during cardiac arrest: its relation to arrest duration and left ventricular pump function. Crit Care Med 2009;37:471-5. [PubMed]
- Koike A, Nagayama O, Hoshimoto-Iwamoto M, et al. Clinical significance of cerebral oxygenation during exercise in patients with coronary artery disease. Circ J 2008;72:1852-8. [PubMed]
- Schön J, Heringlake M, Berger K, et al. Relationship between mixed venous oxygen saturation and regional cerebral oxygenation in awake, spontaneously breathing cardiac surgery patients. Minerva Anestesiol 2011;77:952-8. [PubMed]
- Paarmann H, Heringlake M, Sier H, et al. The association of non-invasive cerebral and mixed venous oxygen saturation during cardiopulmonary resuscitation. Interact Cardiovasc Thorac Surg 2010;11:371-3. [PubMed]
- Paarmann H, Heringlake M, Heinze H, et al. Non-invasive cerebral oxygenation reflects mixed venous oxygen saturation during the varying haemodynamic conditions in patients undergoing transapical transcatheter aortic valve implantation. Interact Cardiovasc Thorac Surg 2012;14:268-72. [PubMed]
- Paarmann H, Schoen J, Schmidt W, et al. Agreement of noninvasive cerebral oxygenation with mixed venous oxygen saturation in patients undergoing ECMO-therapy. Appl Cardiopulm Pathophysiol 2011;15:55-61.
- Ranucci M, Isgrò G, De la Torre T, et al. Near-infrared spectroscopy correlates with continuous superior vena cava oxygen saturation in pediatric cardiac surgery patients. Paediatr Anaesth 2008;18:1163-9. [PubMed]
- Baraka A, Naufal M, El-Khatib M. Correlation between cerebral and mixed venous oxygen saturation during moderate versus tepid hypothermic hemodiluted cardiopulmonary bypass. J Cardiothorac Vasc Anesth 2006;20:819-25. [PubMed]
- Murkin JM. Cerebral oximetry: monitoring the brain as the index organ. Anesthesiology 2011;114:12-3. [PubMed]
- Crookes BA, Cohn SM, Bloch S, et al. Can near-infrared spectroscopy identify the severity of shock in trauma patients? J Trauma 2005;58:806-13; discussion 813-6. [PubMed]
- Ward KR, Ivatury RR, Barbee RW, et al. Near infrared spectroscopy for evaluation of the trauma patient: a technology review. Resuscitation 2006;68:27-44. [PubMed]
- Sagraves SG, Newell MA, Bard MR, et al. Tissue oxygenation monitoring in the field: a new EMS vital sign. J Trauma 2009;67:441-3; discussion 443-4. [PubMed]
- Beekley AC, Martin MJ, Nelson T, et al. Continuous noninvasive tissue oximetry in the early evaluation of the combat casualty: a prospective study. J Trauma 2010;69:S14-25. [PubMed]
- Cohn SM, Nathens AB, Moore FA, et al. Tissue oxygen saturation predicts the development of organ dysfunction during traumatic shock resuscitation. J Trauma 2007;62:44-54; discussion 54-5. [PubMed]
- Casati A, Fanelli G, Pietropaoli P, et al. Continuous monitoring of cerebral oxygen saturation in elderly patients undergoing major abdominal surgery minimizes brain exposure to potential hypoxia. Anesth Analg 2005;101:740-7. [PubMed]
- Pugliese F, Ruberto F, Tosi A, et al. Regional cerebral saturation versus transcranial Doppler during carotid endarterectomy under regional anaesthesia. Eur J Anaesthesiol 2009;26:643-7. [PubMed]
- Murphy GS, Szokol JW, Marymont JH, et al. Cerebral oxygen desaturation events assessed by near-infrared spectroscopy during shoulder arthroscopy in the beach chair and lateral decubitus positions. Anesth Analg 2010;111:496-505. [PubMed]
- Murkin JM. Attenuation of neurologic injury during cardiac surgery. Ann Thorac Surg 2001;72:S1838-44. [PubMed]
- Heringlake M, Garbers C, Käbler JH, et al. Preoperative cerebral oxygen saturation and clinical outcomes in cardiac surgery. Anesthesiology 2011;114:58-69. [PubMed]
- Shahian DM, O’Brien SM, Filardo G, et al. The Society of Thoracic Surgeons 2008 cardiac surgery risk models: part 1--coronary artery bypass grafting surgery. Ann Thorac Surg 2009;88:S2-22. [PubMed]
- Roques F, Michel P, Goldstone AR, et al. The logistic EuroSCORE. Eur Heart J 2003;24:881-2. [PubMed]
- Nashef SAM, Roques F, Sharples L, et al. EUROSCORE II. Interact Cardiovasc Thorac Surg 2011;13:573. [PubMed]
- Ranucci M. Risk stratification in cardiac surgery. Semin Cardiothorac Vasc Anesth 2010;14:66-7. [PubMed]
- Gregory A, Kohl BA. Con: near-infrared spectroscopy has not proven its clinical utility as a standard monitor in cardiac surgery. J Cardiothorac Vasc Anesth 2013;27:390-4. [PubMed]
- Schoen J, Meyerrose J, Paarmann H, et al. Preoperative regional cerebral oxygen saturation is a predictor of postoperative delirium in on-pump cardiac surgery patients: a prospective observational trial. Critical Care 2011;15:R218. [PubMed]
- Morimoto Y, Yoshimura M, Utada K, et al. Prediction of postoperative delirium after abdominal surgery in the elderly. J Anesth 2009;23:51-6. [PubMed]
- Yao FS, Tseng CC, Ho CY, et al. Cerebral oxygen desaturation is associated with early postoperative neuropsychological dysfunction in patients undergoing cardiac surgery. J Cardiothorac Vasc Anesth 2004;18:552-8. [PubMed]
- de Tournay-Jetté E, Dupuis G, Bherer L, et al. The relationship between cerebral oxygen saturation changes and postoperative cognitive dysfunction in elderly patients after coronary artery bypass graft surgery. J Cardiothorac Vasc Anesth 2011;25:95-104. [PubMed]
- Fischer GW, Lin HM, Krol M, et al. Noninvasive cerebral oxygenation May predict outcome in patients undergoing aortic arch surgery. J Thorac Cardiovasc Surg 2011;141:815-21. [PubMed]
- Zheng F, Sheinberg R, Yee MS, et al. Cerebral near-infrared spectroscopy monitoring and neurologic outcomes in adult cardiac surgery patients: a systematic review. Anesth Analg 2013;116:663-76. [PubMed]
- Edmonds HL Jr. Protective effect of neuromonitoring during cardiac surgery. Ann N Y Acad Sci 2005;1053:12-9. [PubMed]
- Austin EH 3rd, Edmonds HL Jr, Auden SM, et al. Benefit of neurophysiologic monitoring for pediatric cardiac surgery. J Thorac Cardiovasc Surg 1997;114:707-15, 717; discussion 715-6.
- Goldman S, Sutter F, Ferdinand F, et al. Optimizing intraoperative cerebral oxygen delivery using noninvasive cerebral oximetry decreases the incidence of stroke for cardiac surgical patients. Heart Surg Forum 2004;7:E376-81. [PubMed]
- Likosky DS, Leavitt BJ, Marrin CA, et al. Intra- and postoperative predictors of stroke after coronary artery bypass grafting. Ann Thorac Surg 2003;76:428-34. [PubMed]
- Murkin JM, Adams SJ, Novick RJ, et al. Monitoring brain oxygen saturation during coronary bypass surgery: a randomized, prospective study. Anesth Analg 2007;104:51-8. [PubMed]
- Edmonds HL Jr. 2010 standard of care for central nervous system monitoring during cardiac surgery. J Cardiothorac Vasc Anesth 2010;24:541-3. [PubMed]
- Slater JP, Guarino T, Stack J, et al. Cerebral oxygen desaturation predicts cognitive decline and longer hospital stay after cardiac surgery. Ann Thorac Surg 2009;87:36-44; discussion 44-5. [PubMed]
- Denault A, Deschamps A, Murkin JM. A proposed algorithm for the intraoperative use of cerebral near-infrared spectroscopy. Semin Cardiothorac Vasc Anesth 2007;11:274-81. [PubMed]
- Fedorow C, Grocott HP. Cerebral monitoring to optimize outcomes after cardiac surgery. Curr Opin Anaesthesiol 2010;23:89-94. [PubMed]
- Mutch WA, Patel SR, Shahidi AM, et al. Cerebral oxygen saturation: graded response to carbon dioxide with isoxia and graded response to oxygen with isocapnia. PLoS One 2013;8:e57881. [PubMed]
- Fischer GW, Stone ME. Cerebral air embolism recognized by cerebral oximetry. Semin Cardiothorac Vasc Anesth 2009;13:56-9. [PubMed]
- Argiriadou H, Anastasiadis K, Antonitsis P, et al. Use of cerebral oximetry for monitoring cardiac output during off-pump implantation of Jarvik 2000 left ventricular assist device. Artif Organs 2010;34:267-71. [PubMed]
- Han SH, Kim CS, Lim C, et al. Obstruction of the superior Vena Cava cannula detected by desaturation of the cerebral oximeter. J Cardiothorac Vasc Anesth 2005;19:420-1. [PubMed]
- Vernick WJ, Oware A. Early diagnosis of superior Vena Cava obstruction facilitated by the use of cerebral oximetry. J Cardiothorac Vasc Anesth 2011;25:1101-3. [PubMed]
- Vretzakis G, Ferdi E, Argiriadou H, et al. Influence of bispectral index monitoring on decision making during cardiac anesthesia. J Clin Anesth 2005;17:509-16. [PubMed]
- Vretzakis G, Kleitsaki A, Aretha D, et al. Management of intraoperative fluid balance and blood conservation techniques in adult cardiac surgery. Heart Surg Forum 2011;14:E28-39. [PubMed]
- Vretzakis G, Kleitsaki A, Stamoulis K, et al. Intra-operative intravenous fluid restriction reduces perioperative red blood cell transfusion in elective cardiac surgery, especially in transfusion-prone patients: a prospective, randomized controlled trial. J Cardiothorac Surg 2010;5:7. [PubMed]
- Vretzakis G, Georgopoulou S, Stamoulis K, et al. Monitoring of brain oxygen saturation (INVOS) in a protocol to direct blood transfusions during cardiac surgery: a prospective randomized clinical trial. J Cardiothorac Surg 2013;8:145. [PubMed]
- Dossche KM, Schepens MA, Morshuis WJ, et al. Antegrade selective cerebral perfusion in operations on the proximal thoracic aorta. Ann Thorac Surg 1999;67:1904-10. [PubMed]
- Hedayati N, Sherwood JT, Schomisch SJ, et al. Axillary artery cannulation for cardiopulmonary bypass reduces cerebral microemboli. J Thorac Cardiovasc Surg 2004;128:386-90. [PubMed]
- Malvindi PG, Scrascia G, Vitale N. Is unilateral antegrade cerebral perfusion equivalent to bilateral cerebral perfusion for patients undergoing aortic arch surgery? Interact Cardiovasc Thorac Surg 2008;7:891-7. [PubMed]
- Murkin JM. NIRS: a standard of care for CPB vs. an evolving standard for selective cerebral perfusion? J Extra Corpor Technol 2009;41:11-4. [PubMed]
- Orihashi K, Sueda T, Okada K, et al. Near-infrared spectroscopy for monitoring cerebral ischemia during selective cerebral perfusion. Eur J Cardiothorac Surg 2004;26:907-11. [PubMed]
- Olsson C, Thelin S. Regional cerebral saturation monitoring with near-infrared spectroscopy during selective antegrade cerebral perfusion: diagnostic performance and relationship to postoperative stroke. J Thorac Cardiovasc Surg 2006;131:371-9. [PubMed]
- Schön J, Serien V, Heinze H, et al. Association between cerebral desaturation and an increased risk of stroke in patients undergoing deep hypothermic circulatory arrest for cardiothoracic surgery. Appl Cardiopulm Pathophysiol 2009;13:201-7.
- Harrer M, Waldenberger FR, Weiss G, et al. Aortic arch surgery using bilateral antegrade selective cerebral perfusion in combination with near-infrared spectroscopy. Eur J Cardiothorac Surg 2010;38:561-7. [PubMed]
- Anastasiadis K, Argiriadou H, Antonitsis P, et al. Cerebral Oximetry-Guided antegrade cerebral perfusion in aortic arch surgery. J Cardiothorac Vasc Anesth 2011;25:591-2. [PubMed]


