Is closed thoracic drainage tube necessary for minimally invasive thoracoscopic-esophagectomy?
Introduction
Despite the incredible surgical progress recently, esophagectomy remains the most complex and high-risk operation procedure with high perioperative morbidity and mortality rates (1,2), even by the popular way of minimally invasive esophagectomy (MIE) approach (3,4). For now, almost all patients underwent thoracic operation had to leave a closed thoracic drainage tube (CTDT), a 11-mm diameter hard pipe, though intercostals space as the optimal treatment worldwide (5).
Although, the use of CTDT could help us access the postoperative chest situation, it also has some disadvantages including postoperative pain and tube related complications, which might reduce the patients’ satisfaction and delay the perioperative recovery (6,7). Thus, it comes a question about the necessity of CTDT after esophagectomy.
Although some studies have analyzed the application of fast-track surgery concept on esophageal cancer patients through esophagectomy (open and/or MIE approach) (8-10), few studies had focused on the perioperative effect of CTDT after thoracoscopic-esophagectomy. Thus, we report a single center, retrospective study to exam the safety and necessity of no-CTDT treatment in esophageal cancer patients underwent thoracoscopic-esophagectomy.
Methods
Patients
Candidate patients who underwent minimally invasive esophagectomy (including thoracoscopy and laparoscopy process) for esophageal squamous carcinoma in Division One of Xijing Digestive Hospital between October 2015 and August 2016 were enrolled in the study in chronological order. Every patient was evaluated carefully before anesthesia and operation. This retrospective study was approved by the Ethics Committee of Xijing Hospital (No. KY20163378-1) and all aspects of the study comply with the Declaration of Helsinki and local legislation. A written informed consent was obtained from all patients at the time of admission, with which the blood, tissue and other sample were authorized to scientific purpose.
Surgical procedures
Each patient was underwent two-lung ventilation anesthesia approach with a single-lumen endotracheal tube in the standard conventional procedure in semi-prone position. The thoracic procedure was performed by the same team of two experienced trained surgeons. The thoracoscopic process of three-port approach (fifth intercostal space on mid-axillary line for observation, fourth and eighth intercostal space on posterior axillary line respectively for thoracic procedure) was used as we described before (11). And, the fourth port as an assistant operation hole was made at sixth intercostal space on subscapular angle line if the patient had a bigger pleural space (Figure 1).
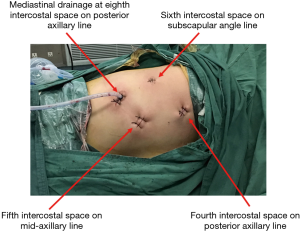
At the end of thoracoscopy, a 6 mm-diameter soft mediastinal drainage tube through the whole thoracic cavity from the port at eighth intercostal space on posterior axillary line was placed (Figure 1). The enrolled patients had been separated into two groups by chronological order, CTDT group (October 2015 to March 2016) and no-CTDT group (April 2016 to August 2016), and patients with pleural adhesions, history of pleurisy or tuberculosis, and broken pleural during thoracoscopy were excluded. Then, patients were changed to supine position for conventional standard laparoscopic and cervical procedure, and a nasal feeding tube was put into the jejunum. Nasogastric intubation and cervical drainage wasn’t used as routine treatment, and abdominal drainage was used for all patients after operation (Figure 2).

Perioperative demographic and surgical parameter in the two groups (age, gender, smoking habit, neoadjuvant treatment, ASA classification, thoracoscopic operation time, blood loss, ICU stay, postoperative mobilization and oral feeding, postoperative TNM stages, postoperative complications and length of hospital stay, pain scale scoring and Norton scoring) on postoperative days 0, 1, 2 and 3 were carefully recorded and assessed. Also, the situation of co-morbidity (including coronary heart disease, diabetes, hypertension and COPD) was collected.
Statistical analysis
Continuous variables are expressed as the mean ± SD, or the median (range) and categorical variables as a percentage. A Student t-test or Mann-Whitney test was used for intergroup comparisons of continuous variables, whereas a χ2 test or Fisher test was used to compare categorical data. Data were analyzed using SPSS 21.0 for Windows (SPSS Inc., Chicago, IL, USA). The P values were considered to be statistically significant at the 5% level.
Results
All patients performed esophagectomy successfully by combination of thoracoscopy and laparoscopy at Xijing Hospital of Digestive Disease, Shanxi Province, China, by the same skilled surgeons team, and it was no incidence of conversion to open thoracotomy or major complications during operation, such as aorta bleeding, tracheal and lung injury, or perioperative death.
Finally, 50 consecutive patients were enrolled, 18 patients without CTDT and 32 patients with CTDT. All patients received chest routine X-ray examine at the first three days, and the CTDT of CTDT group were removed at postoperative day 3. After the operation, the abdominal drainage was also removed at day 3 and mediastinal drainage withdraws at day 7 after assessed by upper gastrointestinal radiography test.
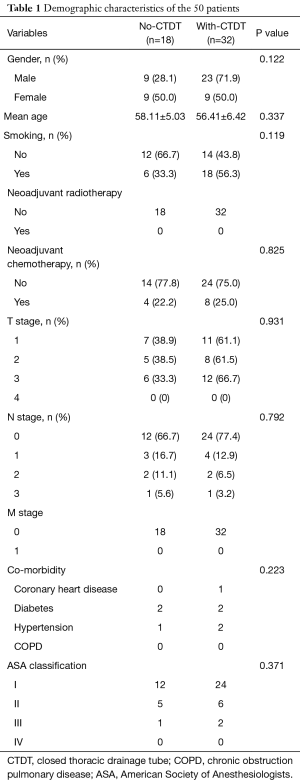
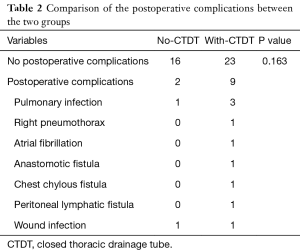
The epidemiologic and clinical characteristics (gender, age, smoking habit, neoadjuvant treatment, ASA classification, co-morbidity, thoracoscopic operation time, blood loss, ICU stay, pathological T and N staging, postoperative mobilization and oral feeding, postoperative hospital stay) between the two groups showed no significant difference (Table 1). Although two patients of no-CTDT group had postoperative complication (one pneumonia and one wound infection), there were difference in the incidence of postoperative complications between the two groups (Table 2).
Full table
Full table
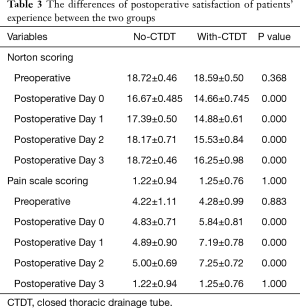
Compared with CTDT group, the no-CTDT group had significantly better Norton scoring and less pain scale scoring according to the Numeric Rating Scale from the first day after the operation, led to better post-operative patients’ experience (Table 3).
Full table
Discussion
Regardless the development of MIE in esophageal cancer, patient with esophageal squamous carcinoma still forced to go through a series of dangerous perioperative treatment and terrible experience with less post-operative satisfaction (1,12).
Since the fast-track surgery (FTS) was introduced to esophageal surgery by Cerfolio et al. (13,14), few studies focused on the role in esophageal surgery practice. Zhao et al. (15) reported a result of FTS for 68 patients, in which they demonstrated FTS promote early recovery of gastrointestinal function and reduce stress reaction and postoperative insulin resistance after esophagectomy. Shewale et al. (16) indicated a fast-track esophagectomy protocol could reduce patients’ length of hospital stay, perioperative morbidity and hospital charges. Also in Chen’s research (8), FTP improved postoperative clinical recovery and effectively inhibited release of inflammatory factors after esophagectomy. And Gemmill reviewed 11 articles about FTS in esophageal resection, and the focus following esophagectomy (open or MIE approach) was early mobilization, reduction in ICU stay, early drain removal and (no) contrast swallow studies (10).
Although the FTS concept was practiced in esophageal surgery recently (17), we still believed options could be made for better and faster recovery after MIE, such as the use of CTDT. Now, none of these studies mainly explored the necessity of CTDT after esophagectomy, especially the MIE approach.
Until now, the use of CTDT seems to be one of the most significant treatments after thoracoscopy. But with the CTDT, patients often felt uncomfortable when breathing and mobilization because the drainage tube could hurt the right lung during variation of the lung volume, might lead to less satisfaction, more postoperative complication and longer hospital stay.
Here, we report the result of safety and necessity on patients without CTDT after thoracoscopic-esophagectomy. All patients underwent minimally invasive esophagectomy successfully without major complications which need convert to open thoracotomy, such as tracheal and lung injury, aorta bleeding, and perioperative mortality.
Compared to patients of with-CTDT group, patients in no-CTDT group had better post-operative satisfaction experience, less pain and better Norton scoring, with similar perioperative surgical parameters (thoracic operation time, blood loss, ICU stay, postoperative mobilization and oral feeding and hospital stay), and there was no statistical difference in postoperative complications between the two groups. Also, the treatment of without-CTDT would reduce the work intensity of medical on patients after MIE, which might give the nursing team better work experience.
But, there are limitations in our study. Firstly, the lack of patients’ accumulation in this study might be solved by the time. Secondly, a single center-based research design might lead to an uncertain amount of selection bias. Thirdly, the present study is a retrospective analysis and a well-designed randomized clinical trial should be carried out in order to avoid statistical bias.
In conclusion, the current study indicated that patients without CTDT after MIE is safe and feasible with almost the same surgical condition compared to traditional treatment, but might lead to a better post-operative experience for both patients and medical stuff.
Acknowledgements
Funding: This work was supported by National Natural Science Foundation of China Grants: No.81300301, 8572306, 81672742, 81502403; Xijing Zhu-Tui Project of the Fourth Military Medical University: No. XJZT12Z03.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This retrospective study was approved by the Ethics Committee of Xi-jing Hospital (No. KY20163378-1) and all aspects of the study comply with the Declaration of Helsinki and local legislation. A written informed consent was obtained from all patients at the time of admission, with which the blood, tissue and other sample were authorized to scientific purpose.
References
- Kauppila JH, Xie S, Johar A, et al. Meta-analysis of health-related quality of life after minimally invasive versus open oesophagectomy for oesophageal cancer. Br J Surg 2017;104:1131-40. [Crossref] [PubMed]
- Gurusamy KS, Pallari E, Midya S, et al. Laparoscopic versus open transhiatal oesophagectomy for oesophageal cancer. Cochrane Database Syst Rev 2016;3:CD011390. [PubMed]
- Xiong WL, Li R, Lei HK, et al. Comparison of outcomes between minimally invasive oesophagectomy and open oesophagectomy for oesophageal cancer. ANZ J Surg 2017;87:165-70. [Crossref] [PubMed]
- Yibulayin W, Abulizi S, Lv H, et al. Minimally invasive oesophagectomy versus open esophagectomy for resectable esophageal cancer: a meta-analysis. World J Surg Oncol 2016;14:304. [Crossref] [PubMed]
- Zheng GL, Zhou H, Zhou XG, et al. Is Traditional Closed Thoracic Drainage Necessary to Treat Pleural Tears After Posterior Approach Thoracic Spine Surgery? Spine (Phila Pa 1976) 2018;43:E185-92. [Crossref] [PubMed]
- Sohda M, Kuwano H. Current Status and Future Prospects for Esophageal Cancer Treatment. Ann Thorac Cardiovasc Surg 2017;23:1-11. [Crossref] [PubMed]
- de Abreu IR, Pontes EP, Tamagno MF, et al. Treatment of thoracic wounds with adapted vacuum therapy. Asian J Surg 2014;37:49-52. [Crossref] [PubMed]
- Chen L, Sun L, Lang Y, et al. Fast-track surgery improves postoperative clinical recovery and cellular and humoral immunity after esophagectomy for esophageal cancer. BMC Cancer 2016;16:449. [Crossref] [PubMed]
- Tan JT, Zhong JH, Yang Y, et al. Comparison of postoperative immune function in patients with thoracic esophageal cancer after video-assisted thoracoscopic surgery or conventional open esophagectomy. Int J Surg 2016;30:155-60. [Crossref] [PubMed]
- Gemmill EH, Humes DJ, Catton JA. Systematic review of enhanced recovery after gastro-oesophageal cancer surgery. Ann R Coll Surg Engl 2015;97:173-9. [Crossref] [PubMed]
- Cai L, Li Y, Sun L, et al. Better perioperative outcomes in thoracoscopic-esophagectomy with two-lung ventilation in semi-prone position. J Thorac Dis 2017;9:117-22. [Crossref] [PubMed]
- Gatenby PA, Shaw C, Hine C, et al. Retrospective cohort study of an enhanced recovery programme in oesophageal and gastric cancer surgery. Ann R Coll Surg Engl 2015;97:502-7. [Crossref] [PubMed]
- Cerfolio RJ, Bryant AS, Bass CS, et al. Fast tracking after Ivor Lewis esophagogastrectomy. Chest 2004;126:1187-94. [Crossref] [PubMed]
- Cerfolio RJ, Bryant AS. Does minimally invasive thoracic surgery warrant fast tracking of thoracic surgical patients? Thorac Surg Clin 2008;18:301-4. [Crossref] [PubMed]
- Zhao G, Cao S, Cui J. Fast-track surgery improves postoperative clinical recovery and reduces postoperative insulin resistance after esophagectomy for esophageal cancer. Support Care Cancer 2014;22:351-8. [Crossref] [PubMed]
- Shewale JB, Correa AM, Baker CM, et al. Impact of a Fast-track Esophagectomy Protocol on Esophageal Cancer Patient Outcomes and Hospital Charges. Ann Surg 2015;261:1114-23. [Crossref] [PubMed]
- Wang JY, Hong X, Chen GH, et al. Clinical application of the fast track surgery model based on preoperative nutritional risk screening in patients with esophageal cancer. Asia Pac J Clin Nutr 2015;24:206-11. [PubMed]


