Nonintubated thoracoscopic surgery: state of the art and future directions
Introduction
In the past two decades, video-assisted thoracoscopic surgery (VATS) has become a common and globally accepted alternative in place of thoracotomy to surgically treated patients with various thoracic conditions involving lungs, pleura and mediastinum (1-3). A minimally invasive approach is demonstrated to be superior in shortening length of hospital stay, alleviating postoperative pain, improving postoperative lung function and reducing overall morbidities after surgery (4-6). Traditionally, intubated general anesthesia with one-lung ventilation, using a double-lumen tube or an endobronchial blocker, has been considered mandatory during VATS to obtain a quiet, optimally visualized and better surgical environment (7). In spite of well-tolerated, complications and adverse effects following intubated general anesthesia and one-lung ventilation are inevitable, including intubation-related airway trauma, ventilation-induced lung injury, residual neuromuscular blockade, impaired cardiac performance, and postoperative nausea and vomiting (8-10).
Recently, interests and efforts have been made to adopt a thoracoscopic technique without tracheal intubation for avoidance of intubation-related complications and for a smoother postoperative recovery. Successful results are accumulating not only from anecdotal case reports of difficult and high-risk patients not suitable for an intubated general anesthesia (11-14), but also from a systemic application of this technique to various thoracic procedures, including management of pneumothorax, wedge resection of pulmonary tumors, excision of mediastinal tumors, lung volume reduction surgery, segmentectomy, and lobectomy (15-35). Encouragingly, the safety and feasibility of this surgical modality were well established in previous studies. Although its short- and long-term benefits comparing to standard intubated general anesthesia are not clearly addressed yet, several prospective studies are recruiting patients by now to answer this issue.
In this article, we revisit the current literature about anesthetic management and results of nonintubated VATS in various thoracic diseases, and suggest its future role in the field of thoracic surgery.
Anesthetic management of nonintubated VATS
Nonintubated VATS entails thoracoscopic procedures performed under regional anesthetic techniques, with or without consciousness sedation, in spontaneously breathing patients. The anesthetic techniques consist of local anesthesia, intercostal nerve blocks, paravertebral blocks or thoracic epidural anesthesia. Mostly, thoracic epidural anesthesia can be enough to serve solo for nonintubated VATS (36).
To be feasible and safe in performing nonintubated VATS, anesthetic management should meet the considerable physiological derangements during the procedure. The pathophysiological disturbances are mainly attributed to spontaneous one-lung breathing in an open pneumothorax status, influence of the chosen anesthetic techniques and type of surgical manipulations (37).
Open pneumothorax after trocar insertion can cause the nondependent lung to collapse gradually so that nonintubated VATS can be performed. In the meantime, patients may become dyspneic or tachypneic because of open pneumothorax. In such circumstances, awake patients should be reassured and coached to slow their breath. However, sedation may be necessary occasionally if patients become anxious and panic. In patients with conscious sedation, incremental titration of opioid can also be used to attenuate the respiratory responses after open pneumothorax.
Hypoxemia and hypercapnia are always major concerns during one-lung ventilation in thoracic surgery, which may also develop in nonintubated VATS. On contrary to one-lung ventilation during intubated general anesthesia with neuromuscular blockade, efficient contraction of dependent hemidiaphragm in spontaneous one-lung breathing during nonintubated VATS preserves favorably match of ventilation and perfusion in a lateral decubitus position. However, a paradoxical respiratory pattern may cause carbon dioxide rebreathing from nondependent, collapsed lung while mediastinal shifting after open pneumothorax may decrease the compliance and tidal volume of the dependent lung. Fortunately, although hypercapnia may occur, they are usually mild and well-tolerated. After returning to two-lung breathing after surgery, the level of carbon dioxide returns to the normal level. In addition, oxygenation is usually satisfactorily maintained with supplemental oxygen via a facemask (29).
Current results of nonintubated thoracoscopic surgery
Management of lung tumor
As progresses in cancer screening and treatment, patients with lung tumors are increasing, and requiring thoracoscopic management of their lung tumors either for diagnostic or therapeutic purposes. Surgical treatment of lung tumors includes wedge resection, anatomical segmentectomy, lobectomy or pneumonectomy with or without mediastinal lymph node dissection, depending on the nature of the lung tumors (38).
In 2004, Pompeo and his coworkers evaluated the feasibility of awake thoracoscopic resection of solitary pulmonary nodules in 30 patients under sole thoracic epidural anesthesia (15). Comparing to patients with intubated general anesthesia, their results showed that awake technique were safely feasible with better patient satisfaction, less nursing care and shorter in-hospital stay. However, it is important to note that two of the awake patients were converted to intubated general anesthesia because of lung cancer requiring lobectomy via thoracotomy approach (15). Similar results were obtained in patients with metastatic lung tumors using awake VATS metastasectomy (19) and even via a single-port VATS approach (39).
For surgical management of primary lung cancer, major pulmonary resections such as segmentectomy or lobectomy with mediastinal lymph node dissection are usually necessary (38). However, these procedures are associated with longer operating time, frequent lung traction and intense hilar manipulation, which can trigger cough reflex in awake patients. When thoracic epidural anesthesia is used, the reactivity of coughing response can be exaggerated because of an unbalanced parasympathetic activity after sympathetic block (36). While Al-Abdullatief et al. used stellate ganglion block to attenuate cough reflex (18), Chen and his colleagues used ipsilateral intrathoracic vagal block to achieve effective control of cough reflex (29-33,40). In addition, intravenous opioid and propofol were titrated with monitoring of anesthesia depth to further control respiratory rate and alleviate anxiety of patients. Using their nonintubated methods, they reported that nonintubated VATS lobectomy and segmentectomy with mediastinal lymphadenectomy for early stage non-small cell lung cancer could be safely performed (29-33). Rates of conversion to intubated general anesthesia were reported to be between 2.3% to 10.0%, depending on the type of procedure and which could be further decreased as the learning curve progressed (29-33). In addition to be feasible and safe, nonintubated thoracoscopic lobectomy for lung cancer using thoracic epidural anesthesia also offered better postoperative pain control, lower rates of sore throat, earlier resumption of oral intake and shorter length of hospital stay with better noncomplication rates, when comparing to its counterpart of intubated general anesthesia (29,30,32), especially in geriatric lung cancer patients (32).
Spontaneous pneumothorax
Nonintubated VATS for wedge resection of blebs and pleural abrasion have been reported in several studies for management of either primary or secondary spontaneous pneumothorax with satisfactory results (11-13,20,39,41-48). High-risk patients with pneumothorax are usually considered difficult, and might be harmful, to maintain adequate respiratory function during intubated one-lung ventilation, including patients after pneumothorax (11,13,41,42), lung transplantation (47) or those pregnant women (43,46). Successful results are obtained in these high-risk patients using either local anesthesia, intercostal blocks, or thoracic epidural anesthesia.
In a small randomized trial performed by Pompeo et al., 43 awake patients with spontaneous pneumothorax were anesthetized with sole thoracic epidural anesthesia to received VATS bullectomy and pleural abrasion (20). Their results have shown that the awake procedures were not only easily feasible, but also shorten the hospital stay, reduced the cost with comparable clinical outcomes to patients anesthetized with intubated general anesthesia (20). Noda et al. reported similar results in 15 patients with secondary spontaneous pneumothorax with shorter operating room stay and less respiratory complications in awake patients (42).
Recently, awake single-access (uniportal) VATS was also reported feasible for management of spontaneous pneumothorax (39,43,45), even in a case of bilateral pneumothorax (45).
Pleural effusion and empyema
Patients with pleural effusion are frequently associated with medical comorbidities. These patients therefore carry additional risks for intubated general anesthesia. However, chronic collapse of operated lung enables these patients to favorably tolerate surgical pneumothorax during spontaneous one-lung breathing. As a result, they rarely develop significant hypoxemia requiring additional ventilatory support and seem to be the optimal candidate for nonintubated VATS (49).
When management of pleural effusions with medical thoracoscopy, local anesthesia with or without sedation has been widely reported (16,21,50-53). In addition, thoracic paravertebral block or epidural anesthesia are also useful and reported for more accurate pleural biopsies or extensive pleurodesis to be easily performed by nonintubated VATS (14,22).
Moreover, Tacconi et al. had reported 19 cases with thoracic empyema treated with awake VATS decortication under sole thoracic epidural anesthesia or paravertebral block (24). Notably, conversion to lateral thoracotomy was performed in four patients because of thick pleural adhesions. The oxygenation was satisfactory during surgery except permissive hypercapnia developed in three patients but no need of conversion to intubated general anesthesia. Their results are successful and no recurrence requiring another surgery in all patients (24). Nonetheless, thoracic epidural catheterization in patients with empyema should be cautiously evaluated to avoid of epidural abscess resulting from bacterial contamination (54).
Emphysema and lung volume reduction surgery
Resectional lung volume reduction surgery is a palliative surgical treatment in severe emphysema patients with impaired exercise tolerance to improve pulmonary function, exercise capacity, and quality of life (55,56). However, it still carries high rates of mortality and morbidity, especially prolonged air leak after surgery (57,58). In 2006, Mineo et al. developed a novel nonresectional technique to perform awake lung volume reduction surgery in awake patients under thoracic epidural anesthesia (17). Their further studies including a randomized trial showed that awake nonresectional lung volume reduction surgery caused significantly functional improvement, including absolute increase in forced expiratory volume in one second, functional vital capacity and residual volume, improvement in exercise capacity index and 6-minute walking test. These improvements lasted for more than 24 months (26,27,59). Comparing to conventional intubated general anesthesia, durations of postoperative air leak and hospital stay were significantly shorter in awake technique, while 3-year survival was comparable (26,60). Similar results were also reported in patients with bullous emphysema (25,61).
Lung biopsy for interstitial lung diseases
Patients with interstitial lung disease are usually associated with impaired respiratory function (62). Although precise histopathologic characterization by surgical lung biopsy can help orient therapy and reliably predict prognosis, VATS biopsy using intubated general anesthesia still carries not negligibly mortality rate (63). In 2012, Pompeo and his colleagues reported 30 awake patients completed VATS biopsy for interstitial lung disease using thoracic epidural anesthesia or intercostal blocks without operative mortality and only one minor complication (3.3%) (28). In addition, precise histopathologic diagnosis was achieved in 29 (97%) patients. They concluded that awake VATS lung biopsy by regional anesthesia might become the safest and most accurate surgical method for obtaining precise histopathologic diagnosis, and potentially leading to better management of interstitial lung diseases (28).
Myasthenia gravis/thymectomy and biopsy of mediastinal masses
Patients with myasthenia gravis are usually sensitive to neuromuscular blockade and perioperative uses of muscle relaxants are associated prolonged mechanical ventilation or re-intubation in these patients. In addition, risks of intubated general anesthesia are increased when anterior mediastinal mass compresses the airway. The rationale of avoiding use of muscle relaxants in these patients, both Matsumoto et al. (64) and Al-Abdullatief et al. (18) reported satisfactory feasibility and results of awake VATS thymectomy using thoracic epidural anesthesia. VATS biopsy of anterior mediastinal masses could also be satisfactorily achieved with high diagnostic yield and no mortality and limited morbidity (23).
Other nonintubated VATS procedures were also reported to manage pericardial effusion (14) and treat palmar hyperhidrosis via thoracic sympathectomy (65).
Potential advantages of nonintubated VATS and its future directions
Although thoracic surgery has its traditional root under regional anesthesia without tracheal intubation, modern thoracoscopic surgery benefits and fundamentally develops under the establishment and safety practice of intubated general anesthesia with effective one-lung ventilation (7). Still, critically ill patients are sometimes challenging and their risks for an intubated general anesthesia are not negligible (9). For instance, prolonged use of mechanical ventilator and stay of intensive care unit are not uncommon for patients with compromised lung function or neuromuscular diseases such as myasthenic patients. Renaissance of nonintubated techniques for VATS, either in awake or sedative patients, are naturally applied not only on anecdotal difficult cases but also broadly on a variety of VATS procedures.
Current reported studies in the literature support the feasibility and safety of nonintubated VATS for management of pleural, mediastinal and pulmonary diseases. Potential advantages of nonintubated VATS are faster postoperative recovery and less over-all complication rates, by which enhance a short length of hospital stay. Therefore, use of nonintubated VATS may translate into a fast track protocol bypassing intensive care or postoperative ventilator support. For patients with high risks for an intubated general anesthesia, this technique may offer better chances for surgical treatment.
In addition to these beneficial early outcomes, nonintubated VATS under thoracic epidural anesthesia are also demonstrated to attenuate surgical stress responses as decreased level of stress hormones and preservation of function of natural killer cells, comparing to intubated general anesthesia (66,67). It is recently hypothesized that regional anesthesia and analgesia may protect cancer patients from recurrence or metastases after surgery (68-70). This implies that further investigation including long-term outcomes (recurrence-free survival or over-all survival) by large controlled trial is needed in attempts to develop safer, more effective and less invasive surgical strategies for an optimal treatment of lung cancer patients.
For institution applying this technique, we suggest that collaborative thoracic surgeons and anesthesiologists should select their patients carefully in the early phase of learning curve. Individualized decisions should be made according to the intended procedure, anesthetic method and characteristics of patients without jeopardizing the safety of patients. Suggested indications and contraindications of nonintubated VATS are listed in Table 1. Notably, nonintubated thoracoscopic experiences can be accumulated from simple and minor procedures. When both surgeon and anesthesiologist getting familiar with this technique, major pulmonary resections for lung tumors, such as segmentectomy or lobectomy, are feasible. However, we suggest an effective sedative anesthetic care and blockade of cough reflex are imperative in nonintubated procedures for major pulmonary resections. Monitoring of anesthetic depth and adequacy of ventilation are important for patients’ safety, which requiring the continuing vigilance of caring anesthesiologists through the procedure. Even so, conversion to intubated general anesthesia may occasionally mandatory. Plans and equipment for a prompt conversion to intubated general anesthesia should be available immediately and performed without hesitation to decrease the risk of emergency intubation (29).
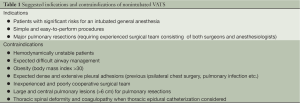
Full table
Conclusions
In a modern era of minimally invasive thoracoscopic surgery, we are encouraged that tracheal intubation with double lumen tube or bronchial blocker is no longer regarded as a prerequisite for single lung ventilation in series of reported studies. Nonintubated thoracoscopic surgery is feasible and safe in a variety of thoracic procedures, including pulmonary resection, empyema, and excision of pleural and mediastinal tumors. Although the risks and benefits of this technique are not clear yet, it seems to offer an equally effective and safe alternative for those patients with high risks to intubated general anesthesia. Postoperative recovery is faster with less complication rates. Nonetheless, further studies are still necessary to clarify the indications and true benefits of this technique and its potential beneficial role against postoperative recurrence in lung cancer patients.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Brodsky JB, Cohen E. Video-assisted thoracoscopic surgery. Curr Opin Anaesthesiol 2000;13:41-5. [PubMed]
- Yan TD. Video-assisted thoracoscopic lobectomy-from an experimental therapy to the standard of care. J Thorac Dis 2013;5:S175-6. [PubMed]
- Yan TD, Cao C, D’Amico TA, et al. Video-assisted thoracoscopic surgery lobectomy at 20 years: a consensus statement. Eur J Cardiothorac Surg 2013; [PubMed]
- Shaw JP, Dembitzer FR, Wisnivesky JP, et al. Video-assisted thoracoscopic lobectomy: state of the art and future directions. Ann Thorac Surg 2008;85:S705-9. [PubMed]
- Whitson BA, Groth SS, Duval SJ, et al. Surgery for early-stage non-small cell lung cancer: a systematic review of the video-assisted thoracoscopic surgery versus thoracotomy approaches to lobectomy. Ann Thorac Surg 2008;86:2008-16. [PubMed]
- Yan TD, Black D, Bannon PG, et al. Systematic review and meta-analysis of randomized and nonrandomized trials on safety and efficacy of video-assisted thoracic surgery lobectomy for early-stage non-small-cell lung cancer. J Clin Oncol 2009;27:2553-62. [PubMed]
- Ovassapian A. Conduct of anesthesia. In: Shields TW, LoCicero J, Ponn RB. eds. General thoracic surgery. Philadelphia: Lippincott Williams & Wilkins, 2000:327-44.
- Murphy GS, Szokol JW, Avram MJ, et al. Postoperative residual neuromuscular blockade is associated with impaired clinical recovery. Anesth Analg 2013;117:133-41. [PubMed]
- Fitzmaurice BG, Brodsky JB. Airway rupture from double-lumen tubes. J Cardiothorac Vasc Anesth 1999;13:322-9. [PubMed]
- Gothard J. Lung injury after thoracic surgery and one-lung ventilation. Curr Opin Anaesthesiol 2006;19:5-10. [PubMed]
- Mukaida T, Andou A, Date H, et al. Thoracoscopic operation for secondary pneumothorax under local and epidural anesthesia in high-risk patients. Ann Thorac Surg 1998;65:924-6. [PubMed]
- Inoue K, Moriyama K, Takeda J. Remifentanil for awake thoracoscopic bullectomy. J Cardiothorac Vasc Anesth 2010;24:386-7. [PubMed]
- Noda M, Okada Y, Maeda S, et al. Successful thoracoscopic surgery for intractable pneumothorax after pneumonectomy under local and epidural anesthesia. J Thorac Cardiovasc Surg 2011;141:1545-7. [PubMed]
- Guarracino F, Gemignani R, Pratesi G, et al. Awake palliative thoracic surgery in a high-risk patient: one-lung, non-invasive ventilation combined with epidural blockade. Anaesthesia 2008;63:761-3. [PubMed]
- Pompeo E, Mineo D, Rogliani P, et al. Feasibility and results of awake thoracoscopic resection of solitary pulmonary nodules. Ann Thorac Surg 2004;78:1761-8. [PubMed]
- Katlic MR. Video-assisted thoracic surgery utilizing local anesthesia and sedation. Eur J Cardiothorac Surg 2006;30:529-32. [PubMed]
- Mineo TC, Pompeo E, Mineo D, et al. Awake nonresectional lung volume reduction surgery. Ann Surg 2006;243:131-6. [PubMed]
- Al-Abdullatief M, Wahood A, Al-Shirawi N, et al. Awake anaesthesia for major thoracic surgical procedures: an observational study. Eur J Cardiothorac Surg 2007;32:346-50. [PubMed]
- Pompeo E, Mineo TC. Awake pulmonary metastasectomy. J Thorac Cardiovasc Surg 2007;133:960-6. [PubMed]
- Pompeo E, Tacconi F, Mineo D, et al. The role of awake video-assisted thoracoscopic surgery in spontaneous pneumothorax. J Thorac Cardiovasc Surg 2007;133:786-90. [PubMed]
- Katlic MR, Facktor MA. Video-assisted thoracic surgery utilizing local anesthesia and sedation: 384 consecutive cases. Ann Thorac Surg 2010;90:240-5. [PubMed]
- Piccioni F, Langer M, Fumagalli L, et al. Thoracic paravertebral anaesthesia for awake video-assisted thoracoscopic surgery daily. Anaesthesia 2010;65:1221-4. [PubMed]
- Pompeo E, Tacconi F, Mineo TC. Awake video-assisted thoracoscopic biopsy in complex anterior mediastinal masses. Thorac Surg Clin 2010;20:225-33. [PubMed]
- Tacconi F, Pompeo E, Fabbi E, et al. Awake video-assisted pleural decortication for empyema thoracis. Eur J Cardiothorac Surg 2010;37:594-601. [PubMed]
- Pompeo E, Tacconi F, Frasca L, et al. Awake thoracoscopic bullaplasty. Eur J Cardiothorac Surg 2011;39:1012-7. [PubMed]
- Pompeo E, Tacconi F, Mineo TC. Comparative results of non-resectional lung volume reduction performed by awake or non-awake anesthesia. Eur J Cardiothorac Surg 2011;39:e51-8. [PubMed]
- Pompeo E, Rogliani P, Tacconi F, et al. Randomized comparison of awake nonresectional versus nonawake resectional lung volume reduction surgery. J Thorac Cardiovasc Surg 2012;143:47-54. [PubMed]
- Pompeo E, Rogliani P, Cristino B, et al. Awake thoracoscopic biopsy of interstitial lung disease. Ann Thorac Surg 2013;95:445-52. [PubMed]
- Chen JS, Cheng YJ, Hung MH, et al. Nonintubated thoracoscopic lobectomy for lung cancer. Ann Surg 2011;254:1038-43. [PubMed]
- Chen KC, Cheng YJ, Hung MH, et al. Nonintubated thoracoscopic lung resection: a 3-year experience with 285 cases in a single institution. J Thorac Dis 2012;4:347-51. [PubMed]
- Tseng YD, Cheng YJ, Hung MH, et al. Nonintubated needlescopic video-assisted thoracic surgery for management of peripheral lung nodules. Ann Thorac Surg 2012;93:1049-54. [PubMed]
- Wu CY, Chen JS, Lin YS, et al. Feasibility and safety of nonintubated thoracoscopic lobectomy for geriatric lung cancer patients. Ann Thorac Surg 2013;95:405-11. [PubMed]
- Hung MH, Hsu HH, Chen KC, et al. Nonintubated thoracoscopic anatomical segmentectomy for lung tumors. Ann Thorac Surg 2013;96:1209-15. [PubMed]
- Dong Q, Liang L, Li Y, et al. Anesthesia with nontracheal intubation in thoracic surgery. J Thorac Dis 2012;4:126-30. [PubMed]
- Hsu MC, Hung MH, Chen JS, et al. Acute transverse myelitis after thoracic epidural anesthesia and analgesia: should anesthesia and analgesia be blamed? Acta Anaesthesiol Taiwan 2013;51:37-9. [PubMed]
- Mineo TC. Epidural anesthesia in awake thoracic surgery. Eur J Cardiothorac Surg 2007;32:13-9. [PubMed]
- Kao MC, Lan CH, Huang CJ. Anesthesia for awake video-assisted thoracic surgery. Acta Anaesthesiol Taiwan 2012;50:126-30. [PubMed]
- Murthy S. Video-assisted thoracoscopic surgery for the treatment of lung cancer. Cleve Clin J Med 2012;79 Electronic Suppl 1:eS23-5.
- Rocco G, Romano V, Accardo R, et al. Awake single-access (uniportal) video-assisted thoracoscopic surgery for peripheral pulmonary nodules in a complete ambulatory setting. Ann Thorac Surg 2010;89:1625-7. [PubMed]
- Tsai TM, Chen JS. Nonintubated thoracoscopic surgery for pulmonary lesions in both lungs. J Thorac Cardiovasc Surg 2012;144:e95-7. [PubMed]
- Shigematsu H, Andou A, Matsuo K, et al. Thoracoscopic surgery using local and epidural anesthesia for intractable pneumothorax after BMT. Bone Marrow Transplant 2011;46:472-3. [PubMed]
- Noda M, Okada Y, Maeda S, et al. Is there a benefit of awake thoracoscopic surgery in patients with secondary spontaneous pneumothorax? J Thorac Cardiovasc Surg 2012;143:613-6. [PubMed]
- Onodera K, Noda M, Okada Y, et al. Awake video-thoracoscopic surgery for intractable pneumothorax in pregnancy by using a single portal plus puncture. Interact Cardiovasc Thorac Surg 2013;17:438-40. [PubMed]
- Mineo TC, Ambrogi V. Awake thoracic surgery for secondary spontaneous pneumothorax: another advancement. J Thorac Cardiovasc Surg 2012;144:1533-4. [PubMed]
- Rocco G, La Rocca A, Martucci N, et al. Awake single-access (uniportal) video-assisted thoracoscopic surgery for spontaneous pneumothorax. J Thorac Cardiovasc Surg 2011;142:944-5. [PubMed]
- Chen YH, Hung MH, Chen JS, et al. Nonintubated video-assisted thoracoscopic surgery (VATS) for recurrent spontaneous pneumothorax in a pregnant woman: 11AP5-10. Eur J Anaesthesiol 2013;30:180. [PubMed]
- Sugimoto S, Date H, Sugimoto R, et al. Thoracoscopic operation with local and epidural anesthesia in the treatment of pneumothorax after lung transplantation. J Thorac Cardiovasc Surg 2005;130:1219-20. [PubMed]
- Nezu K, Kushibe K, Tojo T, et al. Thoracoscopic wedge resection of blebs under local anesthesia with sedation for treatment of a spontaneous pneumothorax. Chest 1997;111:230-5. [PubMed]
- Pompeo E. Awake thoracic surgery--is it worth the trouble? Semin Thorac Cardiovasc Surg 2012;24:106-14. [PubMed]
- Alrawi SJ, Raju R, Acinapura AJ, et al. Primary thoracoscopic evaluation of pleural effusion with local anesthesia: an alternative approach. JSLS 2002;6:143-7. [PubMed]
- Migliore M, Giuliano R, Aziz T, et al. Four-step local anesthesia and sedation for thoracoscopic diagnosis and management of pleural diseases. Chest 2002;121:2032-5. [PubMed]
- Sakuraba M, Masuda K, Hebisawa A, et al. Thoracoscopic pleural biopsy for tuberculous pleurisy under local anesthesia. Ann Thorac Cardiovasc Surg 2006;12:245-8. [PubMed]
- Sakuraba M, Masuda K, Hebisawa A, et al. Diagnostic value of thoracoscopic pleural biopsy for pleurisy under local anaesthesia. ANZ J Surg 2006;76:722-4. [PubMed]
- Hung MH, Chen JS, Cheng YJ. Epidural catheterisation for empyema thoracis: risk of epidural abscess. Eur J Cardiothorac Surg 2011;39:145-6. [PubMed]
- Gelb AF, McKenna RJ Jr, Brenner M, et al. Lung function 5 yr after lung volume reduction surgery for emphysema. Am J Respir Crit Care Med 2001;163:1562-6. [PubMed]
- Miller JD, Malthaner RA, Goldsmith CH, et al. A randomized clinical trial of lung volume reduction surgery versus best medical care for patients with advanced emphysema: a two-year study from Canada. Ann Thorac Surg 2006;81:314-20. [PubMed]
- Naunheim KS, Wood DE, Krasna MJ, et al. Predictors of operative mortality and cardiopulmonary morbidity in the National Emphysema Treatment Trial. J Thorac Cardiovasc Surg 2006;131:43-53. [PubMed]
- DeCamp MM, Blackstone EH, Naunheim KS, et al. Patient and surgical factors influencing air leak after lung volume reduction surgery: lessons learned from the National Emphysema Treatment Trial. Ann Thorac Surg 2006;82:197-206. [PubMed]
- Pompeo E, Mineo TC. Two-year improvement in multidimensional body mass index, airflow obstruction, dyspnea, and exercise capacity index after nonresectional lung volume reduction surgery in awake patients. Ann Thorac Surg 2007;84:1862-9. [PubMed]
- Tacconi F, Pompeo E, Mineo TC. Duration of air leak is reduced after awake nonresectional lung volume reduction surgery. Eur J Cardiothorac Surg 2009;35:822-8. [PubMed]
- Nagashima K, Sakurai K, Sengoku K, et al. Anesthetic management for thoracoscopic bullae resection using epidural anesthesia. Masui 2001;50:56-8. [PubMed]
- Raghu G, Collard HR, Egan JJ, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med 2011;183:788-824. [PubMed]
- Park JH, Kim DK, Kim DS, et al. Mortality and risk factors for surgical lung biopsy in patients with idiopathic interstitial pneumonia. Eur J Cardiothorac Surg 2007;31:1115-9. [PubMed]
- Matsumoto I, Oda M, Watanabe G. Awake endoscopic thymectomy via an infrasternal approach using sternal lifting. Thorac Cardiovasc Surg 2008;56:311-3. [PubMed]
- Elia S, Guggino G, Mineo D, et al. Awake one stage bilateral thoracoscopic sympathectomy for palmar hyperhidrosis: a safe outpatient procedure. Eur J Cardiothorac Surg 2005;28:312-7. [PubMed]
- Vanni G, Tacconi F, Sellitri F, et al. Impact of awake videothoracoscopic surgery on postoperative lymphocyte responses. Ann Thorac Surg 2010;90:973-8. [PubMed]
- Tacconi F, Pompeo E, Sellitri F, et al. Surgical stress hormones response is reduced after awake videothoracoscopy. Interact Cardiovasc Thorac Surg 2010;10:666-71. [PubMed]
- Ash SA, Buggy DJ. Does regional anaesthesia and analgesia or opioid analgesia influence recurrence after primary cancer surgery? An update of available evidence. Best Pract Res Clin Anaesthesiol 2013;27:441-56. [PubMed]
- Gottschalk A, Sharma S, Ford J, et al. Review article: the role of the perioperative period in recurrence after cancer surgery. Anesth Analg 2010;110:1636-43. [PubMed]
- Snyder GL, Greenberg S. Effect of anaesthetic technique and other perioperative factors on cancer recurrence. Br J Anaesth 2010;105:106-15. [PubMed]


