Spontaneous coronary artery dissection with multiple coronary artery aneurysms in a patient with diabetic ketoacidosis
Spontaneous coronary artery dissection (SCAD) is a rare cause of acute coronary syndrome (ACS) found in approximately 0.1-0.28% of all angiographic studies (1,2). Diabetic ketoacidosis (DKA) is a rare presentation for SCAD. While several reports suggest an underlying inflammatory or vascular connective tissue disease as the primary etiology, recent studies have revealed a strong association of SCAD with fibromuscular dysplasia (FMD) (3-5). The association of SCAD with multiple coronary artery aneurysms in this case raises the suspicion of underlying FMD and supports the current reviews, where FMD is considered to be one of the major underdiagnosed etiologies in SCAD.
Case presentation
A 54-year-old African American female with history of HTN presents to the outpatient clinic complaining of generalized weakness, blurry vision, and increased frequency of urination that started a few weeks earlier and became progressively worse. She was found to have critically high blood glucose level, and was sent to the emergency department for further evaluation.
In the emergency department the patient was awake, alert, and oriented with no signs of acute distress, she denied any fever, abdominal pain, nausea, vomiting, or diarrhea, she denied any chest pain, cough, or shortness of breath, palpitations, headache, or loss of consciousness.
Her medical history was significant for essential HTN for the last ten years, for which she has been taking a beta blocker, calcium channel blocker, and an ACE inhibitor, with good compliance and blood pressure control. She had no history of surgery in the past or any drug related allergies. Her family history was significant for myocardial infarction in her father at the age of 52. She did not smoke, drink alcohol, or use illicit drugs. She denied any history of trauma, recent travel, sick contacts, or close contact with animals.
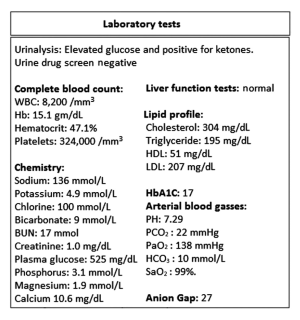
On physical examination, blood pressure: 141/70 mmHg, heart rate: 80 beats per minute, temperature: 98.6 °F, respiratory rate: 18 breaths per minute, oxygen saturation: 98% breathing room air. There was evidence of dehydration as she had dry mucus membranes, and excessive thirst, but with no orthostatic changes in her blood pressure or heart rate. Her neurological, respiratory, cardiovascular, abdominal exams were all within normal. 12-lead electrocardiogram (ECG) was normal. Laboratory tests (Figure 1).
She was diagnosed with DKA as the initial presentation of her underlying diabetes, and admitted to the critical care unit. 24 hours later as her Anion Gap (AG) closed, with adequate blood glucose control, and the resolution of her presenting symptoms, she started complaining of pressure like chest pain, retrosternal, non-radiating, 6/10 in severity.
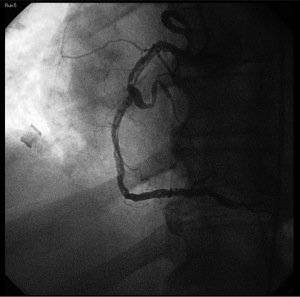
Repeated EKG (Figure 2) showed new onset T wave inversions in lead II, III, aVF, V4-V6.
Initial Troponin level was found to be elevated (troponin I: 2.3 ng/mL), and intravenous unfractionated Heparin was initiated.
2D Echo showed left ventricular inferior wall hypokinesia, a normal ejection fraction, and normal valvular function.
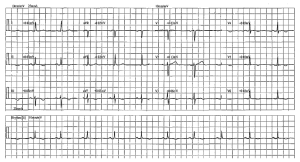
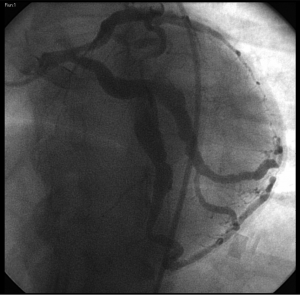
Urgent Left heart catheterization with coronary angiography revealed a long ‘spiral’ complete dissection of the right coronary artery (RCA), with an occlusive intraluminal thrombus (Figure 3), the left main coronary artery angiogram showed multiple aneurismal dilatations in the left anterior descending (LAD) artery and the left circumflex (LC) artery (Figure 4).
No intervention was performed during the catheterization procedure, and the patient was referred for immediate coronary artery bypass grafting.
Intraoperatively multiple LAD and LC artery aneurismal formations were noted. A triple coronary artery bypass was performed and three days later the patient was discharged home on insulin and oral medications.
Discussion
Epidemiology
SCAD is a very rare condition, which is particularly prevalent in young women who are pregnant, or in the puerperal period (6-8).
The earliest report of SCAD was published Pretty in 1931 (9). At that time the disease entity was referred to as “dissecting aneurysm of the coronary artery.” Coronary artery dissection is termed spontaneous once secondary causes such as coronary interventions, cardiac surgery, trauma, and aortic dissection have been excluded (10,11).
The incidence of spontaneous coronary dissection occurs at rates of 0.1-0.28% of all angiographic studies (1,2). A recent case series by Pfieffer et al. highlighted the potential underestimation of the true incidence of SCAD, as previous reviews estimated that 20-50% of SCAD cases present with sudden cardiac death, and these cases do not routinely undergo autopsy (12).
Clinical presentation
The most common presentation of SCAD is an acute onset of severe chest pain, it may also present with a clinical spectrum ranging from; stable angina to a myocardial infarction with cardiogenic shock, and in some cases with sudden death. Associated features include; autonomic symptoms such as diaphoresis, palpitations, and hyper- or hypotension (6,13,14). Asymptomatic cases are rare, and DKA is an unusual presentation of SCAD.
In a recent retrospective study by Tweet et al. in 87 patients with angiographically confirmed SCAD, several characteristics were reviewed and concluded that: 71 (82%) were females with a Mean age of 42.6±10 years, ST-Elevation Myocardial infarction (STEMI) was the presenting diagnosis in 49%. The LAD artery was the most commonly affected vessel. Multivessel coronary dissection at presentation was evident in 20 patients (23%) (4).
Blunt trauma (15), cocaine use (16), and extension of aortic dissection (17) have also been reported to result in coronary dissection. There are over fifty cases in the literature reporting spontaneous coronary dissection during late pregnancy and the early postpartum period (18,19). Systemic illnesses may also predispose to coronary dissection such as connective tissue disorders (20), Marfan's syndrome (21), Kawasaki’s disease (19), alpha-1-antitrypsin deficiency (22) and FMD (1). In general, spontaneous coronary dissection is a life-threatening condition; however, in those surviving the initial event, the survival rate is reported to be 78-82% (23,24).
Pathophysiology
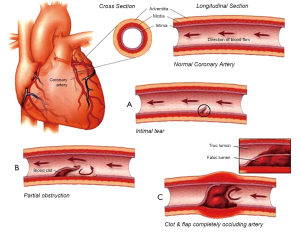
The exact etiology and pathophysiologic mechanism of SCAD remains unknown despite reported histologic features. Proposed theories include; rupture of the vasa vasorum, pregnancy-induced degeneration of collagen in conjunction with the stresses of parturition, and tunica media eosinophilic angiitis. But it is likely that more than one mechanism operates simultaneously in any given case (10,20). The initial mechanical trigger is thought to be a disruption in the intimal layer, and as blood flows beneath the intimal flap it dissects the outer third of the tunica media from the underlying layers and forms a hematoma that grows progressively and eventually occludes the arterial lumen (10,25,26) (Figure 5).
Authors who support the theory of ruptured vasa vasorum however propose that intra tunica-medial hemorrhage is the triggering event for the dissection (5,10,26).
In our patient the SCAD in association with multiple coronary artery aneurysms is a rare finding and raises the suspicion of underlying FMD.
Even though the prevalence of FMD in the general population is not precisely known, it is currently considered to be one of the major underdiagnosed conditions in SCAD. In a recent study by Saw et al. angiograms of SCAD cases over a 6-year period were reviewed and found that most SCAD patients had FMD of ≥1 noncoronary territory (86.0%): renal (58.1%), cerebrovascular (46.5%), intracranial aneurysm (14%) (3). In another study, 25% of the patients with SCAD had changes suggestive of FMD (95% Wilson-confidence interval 9-53%) (5).
The underlying mechanism in which acute myocardial ischemia may precipitate DKA as was the case in our patient, can be explained by the surge of stress hormones; catecholamines such as epinephrine, and cortisol which activate the ketogenic pathways, and as myocardial cells oxidize free fatty acids as the major substrate for myocardial energy production a diminished ketolytic capacity caused by the injured myocardium may contribute to further accumulation of Ketones in patients with a myocardial infarction (27-29).
Treatment and prognosis
Tsimikas et al. reviewed 65 cases of spontaneous coronary dissection reported in the literature since 1993 and suggested that outcomes have improved due to earlier recognition of this entity. Of the 65 patients reported 78% were described as surviving the acute event. Therefore, the inferred acute mortality rate was 22% (24).
Shamloo et al. did a systematic analysis of all published cases and concluded that about 20% of cases were diagnosed postmortem and the rest by coronary angiogram, early intervention (either stent or bypass graft surgery) strategy had a superior outcome compared to conservative management; and administration of thrombolytics (before diagnosis of SCAD) resulted in worsening of condition in 60% of patients (30).
The optimal treatment for SCAD however remains undetermined. Percutaneous coronary intervention (PCI) with periprocedural use of adjunctive imaging technologies such as intravascular ultrasound (IVUS) and optical coherence tomography both to determine extent of vessel wall disruption (which may be underappreciated at angiography alone) and to provide real-time guidance of interventional strategy is critical for a successful procedure (31,32).
Surgical revascularization in SCAD is usually restricted to hemodynamically unstable cases where PCI has failed (such as complete vessel occlusion due to expanding dissection) or is deemed impossible (such as multivessel long segment dissection with good distal segment suitable for bypass) (33), or a dissection involving the left anterior descending artery (4,5,10,11).
Conclusions
SCAD is a rare condition, often presenting with acute myocardial infarction and cardiogenic shock, however a subtle and non-specific presentation of SCAD may also occur, making it a challenging entity where early diagnosis and management remains critical in order to prevent the significant morbidity and mortality associated with this disease.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Jorgensen MB, Aharonian V, Mansukhani P, et al. Spontaneous coronary dissection: a cluster of cases with this rare finding. Am Heart J 1994;127:1382-7. [PubMed]
- Nishikawa H, Nakanishi S, Nishiyama S, et al. Primary coronary artery dissection observed at coronary angiography. Am J Cardiol 1988;61:645-8. [PubMed]
- Saw J, Ricci D, Starovoytov A, et al. Spontaneous coronary artery dissection: prevalence of predisposing conditions including fibromuscular dysplasia in a tertiary center cohort. JACC Cardiovasc Interv 2013;6:44-52. [PubMed]
- Tweet MS, Hayes SN, Pitta SR, et al. Clinical features, management, and prognosis of spontaneous coronary artery dissection. Circulation 2012;126:579-88. [PubMed]
- Toggweiler S, Puck M, Thalhammer C, et al. Associated vascular lesions in patients with spontaneous coronary artery dissection. Swiss Med Wkly 2012;142:w13538. [PubMed]
- Nakamura M, Yajima J, Oikawa Y, et al. Vascular Ehlers-Danlos syndrome--all three coronary artery spontaneous dissections. J Cardiol 2009;53:458-62. [PubMed]
- Xu B, MacIsaac A. Serial spontaneous coronary artery dissections: a transient predisposition affecting multiple coronary arteries? Int J Cardiol 2013;165:544-8. [PubMed]
- Higgins GL 3rd, Borofsky JS, Irish CB, et al. Spontaneous peripartum coronary artery dissection presentation and outcome. J Am Board Fam Med 2013;26:82-9. [PubMed]
- Pretty HC. Dissecting aneurysm of coronary artery in a woman aged 42: rupture. Br Med J 1931;1:667.
- Iturbe JM, Banerjee S, Brilakis ES. Exertional dyspnoea due to spontaneous coronary artery dissection in a 55-year-old man. BMJ Case Rep 2009;2009:bcr2006100982.
- Vicari R, Eybel C, Monson D. Survival following spontaneous coronary artery dissection: surgical repair by extrusion of intramural hematoma. Am Heart J 1986;111:593-4. [PubMed]
- Pfeiffer M, Baquero G, Kozak M. Spontaneous coronary artery dissection: a case series highlighting diagnostic challenges and the potential for underestimating the incidence of this presumed rare disorder. J Invasive Cardiol 2013;25:E159-62. [PubMed]
- Kearney P, Singh H, Hutter J, et al. Spontaneous coronary artery dissection: a report of three cases and review of the literature. Postgrad Med J 1993;69:940-5. [PubMed]
- Harikrishnan S, Ajithkumar VK, Tharakan JM. Spontaneous coronary artery dissection of all major coronary arteries. Can J Cardiol 2007;23:313-4. [PubMed]
- Masuda T, Akiyama H, Kurosawa T, et al. Long-term follow-up of coronary artery dissection due to blunt chest trauma with spontaneous healing in a young Woman. Intensive Care Med 1996;22:450-2. [PubMed]
- Steinhauer JR, Caulfield JB. Spontaneous coronary artery dissection associated with cocaine use: a case report and brief review. Cardiovasc Pathol 2001;10:141-5. [PubMed]
- Virmani R, Forman MB, Robinowitz M, et al. Coronary artery dissections. Cardiol Clin 1984;2:633-46. [PubMed]
- Koul AK, Hollander G, Moskovits N, et al. Coronary artery dissection during pregnancy and the postpartum period: two case reports and review of literature. Catheter Cardiovasc Interv 2001;52:88-94. [PubMed]
- Mckechnie RS, Patel D, Eitzman DT, et al. Spontaneous coronary artery dissection in a pregnant Woman. Obstet Gynecol 2001;98:899-902. [PubMed]
- Borczuk AC, van Hoeven KH, Factor SM. Review and hypothesis: the eosinophil and peripartum heart disease (myocarditis and coronary artery dissection)--coincidence or pathogenetic significance? Cardiovasc Res 1997;33:527-32. [PubMed]
- Bonacchi M, Prifti E, Giunti G, et al. Emergency management of spontaneous coronary artery dissection. J Cardiovasc Surg (Torino) 2002;43:189-93. [PubMed]
- Martín Dávila F, Delgado Portela M, García Rojo M, et al. Coronary artery dissection in alpha-1-antitrypsin deficiency. Histopathology 1999;34:376-8. [PubMed]
- Demaio SJ, Kinsella SH, Silverman ME. Clinical course and long-term prognosis of spontaneous coronary artery dissection. Am J Cardiol 1989;64:471-4. [PubMed]
- Tsimikas S, Giordano FJ, Tarazi RY, et al. Spontaneous coronary artery dissection in patients with renal transplantation. J Invasive Cardiol 1999;11:316-21. [PubMed]
- Shahzad K, Cao L, Ain QT, et al. Postpartum spontaneous dissection of the first obtuse marginal branch of the left circumflex coronary artery causing acute coronary syndrome: a case report and literature review. J Med Case Rep 2013;7:82. [PubMed]
- McCullough JN, Abel RM, Rubenstein H. Polytetrafluoroethylene graft for spontaneous coronary dissection: 7-year follow-up. Ann Thorac Surg 1990;50:663-4. [PubMed]
- Oo YH, Karam JG, Resta CA. Extreme insulin resistance in a patient with diabetes ketoacidosis and acute myocardial infarction. Case Rep Endocrinol 2013;2013:520904.
- Janardhan A, Chen J, Crawford PA. Altered systemic ketone body metabolism in advanced heart failure. Tex Heart Inst J 2011;38:533-8. [PubMed]
- Veech RL, Chance B, Kashiwaya Y, et al. Ketone bodies, potential therapeutic uses. IUBMB Life 2001;51:241-7. [PubMed]
- Shamloo BK, Chintala RS, Nasur A, et al. Spontaneous coronary artery dissection: aggressive vs. conservative therapy. J Invasive Cardiol 2010;22:222-8. [PubMed]
- Jinnouchi H, Sakakura K, Matsuda J, et al. Recurrent spontaneous coronary artery dissection observed with multiple imaging modalities. Int Heart J 2013;54:181-3. [PubMed]
- Gersh BJ, Stone GW, White HD, et al. Pharmacological facilitation of primary percutaneous coronary intervention for acute myocardial infarction: is the slope of the curve the shape of the future? JAMA 2005;293:979-86. [PubMed]
- Motreff P, Souteyrand G, Dauphin C, et al. Management of spontaneous coronary artery dissection: review of the literature and discussion based on a series of 12 young women with acute coronary syndrome. Cardiology 2010;115:10-8. [PubMed]