Clinical significance of skipping mediastinal lymph node metastasis in N2 non-small cell lung cancer
Introduction
Lung cancer is the leading cause of cancer death in the world (1). Lymph node metastasis is one of the most important prognostic factors for non-small cell lung cancer (NSCLC) patients (2,3). Mediastinal lymph node metastasis occurs in 20–40% of NSCLC patients (4). The typical pattern of lung cancer lymphatic metastasis follows a linear model: from the primary tumor, spreading to intrapleural and hilar lymph nodes (N1), then to the ipsilateral mediastinal lymph nodes (N2), then contralateral mediastinal and distance (i.e., supraclavicular nodes) lymph nodes (N3). However, some pN2 patients had no N1 lymph node involvement, a phenomenon called “Skipping mediastinal lymph node metastasis” (5).
Skipping metastasis is not rare in NSCLC. Previous studies reported that around 16–30% of N2 patients had skipping metastasis (6-10). Yet its clinical relevance and relation with patients’ prognosis still remain unknown.
In this study, we retrospectively compared pN2 NSCLC patients with and without hilar lymph node (N1) involvement regarding site and extent of mediastinal lymph node metastasis, the pathological tendency, the location of the primary tumor, and the survival.
Methods
All of the patients with NSCLC, who underwent R0 surgical resection with systematic mediastinal nodal dissection in Cancer Hospital, Chinese Academic of Medical Science (CAMS), from Jan. 1999 to Dec. 2005 were retrospectively reviewed. Patients without systematic lymph node dissection or with palliative surgery were not included. A total of 2,557 patients, 1,611 males and 946 females, aged from 27 to 84 years, were enrolled. Among them, 803 (31.4%) patients who had mediastinal lymph node metastasis (pN2 disease) were enrolled in the final analysis. Medical records and follow-up data were collected for all the patients. TNM (tumor node metastasis) stage was determined based on the seventh edition of the American Joint Committee on Cancer (AJCC) staging system (11). The study was approved by the Institutional Review Board of the Cancer Hospital and Institute of CAMS (No. NCC2017IIT-008).
In statistical analysis, qualitative variables were compared by the chi-square test and quantitative variables by Student’s t-test. Survival analysis was performed using log-rank test. Multivariate analysis for censored data was performed using a Cox regression model. Differences were considered to be significant when P was less than 0.05.
Results
In all the 803 pN2 NSCLC patients enrolled in the study, 137 patients (17.06%) had no involvement in the hilar region and were classified into skip (+) group. The other 666 patients with N1 lymph nodes metastasis were classified into skip (−) or Normal group. The clinicopathologic features of the patients are shown in Table 1.
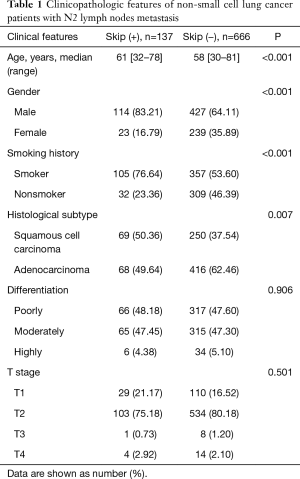
Full table
As shown in Table 1, patients with skipping metastasis had significantly older age than skip (−) patients (median age 61 vs. 58 years, P<0.001). Also, the percentage of male (83.21% vs. 64.11%; P<0.001) and smoker (76.64% vs. 53.60%; P<0.001) patients are significantly higher in the skip (+) group. Plus, patients with skipping metastasis presented significantly more squamous cell lung cancer (50.36% vs. 37.54%; P=0.007). There was no significant difference in cancer cell differentiation and T stage [tumor stage according to the AJCC staging system, seventh edition (11)] between two groups.
The location of the primary lesion was significantly different between two groups. Skip (+) NSCLC are significantly more frequently localized in the right upper lobe (43.07%) than skip (−) disease (23.42%) (P=0.001) (Table 2). The surgical procedures were similar in two groups (P=0.056).
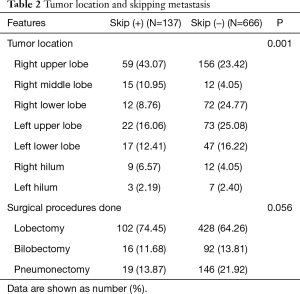
Full table
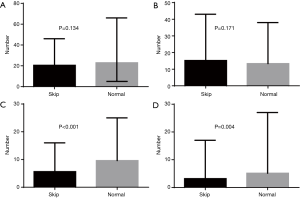
We next analyzed the lymph nodes dissected and the metastatic pattern in the two groups of patients (Table 3). The total number of lymph nodes dissected and the number of N2 lymph nodes dissected were similar in two groups (Figure 1A,B). However, patients with skipping metastasis had significantly fewer N1 lymph node dissection (5.64 vs. 9.62; P<0.001) (Figure 1C) and N2 lymph node metastasis (3.15 vs. 5.13; P=0.004) (Figure 1D).
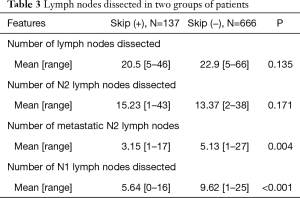
Full table
The number of dissected and metastatic N2 lymph nodes in each station was also summarized (Table 4). Station IV nodes has the highest proportion involvement in the skip (+) group while in the skip (−) group, it is Station V. Station IX had the lowest rate of involvement in both groups. Station VII had significantly lower rate of involvement in skip (+) group compare to skip (−) group (43.12% vs. 68.70%; P=0.017).
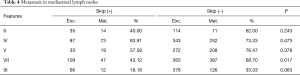
Full table
Most of skip (+) patients had single station mediastinal lymph node metastasis (75.18%), while only 49.55% skip (−) patients had single-station involvement (P<0.001) (Table 5).

Full table
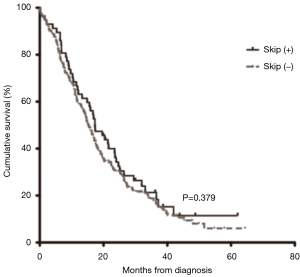
Further, we compared the overall survival of the two groups of patients. Log-rank analysis showed that patients with and without skipping mediastinal lymph node metastasis had similar post-operative overall survival (P=0.379) (Figure 2).
Discussion
Lymph node metastasis is one of the most important prognostic factors for NSCLC patients (12,13). Skipping mediastinal nodal metastasis had been reported in 12–40% of all N2 diseases (8,10). In our present study, skipping metastasis in mediastinal lymph nodes were found in 17% of N2 patients, which was consistent with previous reports.
Patients of both groups in our study have all received lobectomy, bilobectomy, or pneumonectomy plus systematic mediastinal lymph node dissection. The number of lymph nodes dissected and mediastinal lymph node dissected were similar in both groups, and so was the type of surgery. Those results indicate that skipping metastasis was not due to different surgery styles or smaller number of lymph node dissected. Skipping metastasis is an objective phenomenon of lymph node metastasis in NSCLC.
Patients of the skip (+) group also received complete dissection of N1 lymph nodes and these lymph nodes were found to be uninvolved. Our results showed that the number of N1 lymph nodes dissected was significantly smaller in skip (+) group than in skip (−) group. This is not due to incompletely dissection of N1 lymph nodes for the skip (+) group patients, because all patients had received at least lobectomy, and all N1 lymph nodes are removed with the resected lobe. Plus, there was no difference in the amount of lymph nodes dissection and even more N2 lymph node were dissected in skip (+) group. Thus, this result indicates fewer N1 lymph nodes in the skip (+) group. One possible explanation for this is that patients with skipping metastasis had alternative pathways of lymphatic drainage bypassing the N1 nodes, resulting in fewer N1 lymph nodes compared with patients with both N1 and N2 nodes involvement. It has been reported that tumor cells could metastasize to mediastinal nodes through parietal pleura and intrapulmonary lymphatic vessels leaving N1 nodes clear (14). Yet the mechanism behind this still needs further study.
We revealed, in the present study, a higher incidence of skipping metastasis in male, smoker and squamous cell carcinoma patients than in female, non-smoker and adenocarcinoma patients. These were consistent with results reported in previously published studies (7). For the majority of squamous cell carcinoma in male patients are attributed to smoking (15-17), it could be hypothesized that squamous cell carcinoma tend to present skipping nodal metastasis more frequently than other subtypes of NSCLC. The mechanism of this phenomena merits further study.
It has been reported that skipping metastases happens most in patients with right upper lobe NSCLC (18), and our data got similar results. Also, we found that Station IV (lower paratracheal) is the most frequently involved station in skip (+) NSCLC. This is consistent with high incidence of skipping metastasis in right upper lobe. Riquet et al. have reported that direct lymph passages from segmental lymph nodes to mediastinal lymph nodes occurs more commonly in the upper lobe diseases (19). Also noticed is that Station VII (subcarinal lymph nodes) had less involvement in skip (+) group. Misthos et al. reported similar result, and concluded that to be a favorable factor for survival of skip (+) patients. Over 75 percent of skip (+) patients involved one station, which is significantly more than skip (−) group. This finding has also been reported by previous studies (6,18,20,21).
It has been controversial whether there is difference in survival between skip (+) and skip (−) patients. Some studies reported better prognosis for skip (+) patients especially those with single station N2 involvement, compared to skip (−) ones (6,8,9), while others found similar survival (7,18,21,22). Our study showed no significant difference between two groups. However, our finding that skip N2 lymph node metastasis exists makes sense that systematic mediastinal lymph node dissection is necessary for all NSCLC patients even though N1 lymph nodes are found to be clear by frozen section.
Conclusions
In conclusion, skipping mediastinal lymph nodes metastasis occurs in over 10% of N2 NSCLC patients. It is more frequent in male, smoker patients with squamous cell carcinoma and diseases on the right upper lobe. Station IV lymph nodes are most frequently involved. For N2 NSCLC patients, skipping nodal metastasis is not associated with survival. Further study is needed to clarify the basic mechanisms of the phenomenon.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Institutional Review Board of the Cancer Hospital and Institute of CAMS (No. NCC2017IIT-008).
References
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin 2015;65:5-29. [Crossref] [PubMed]
- Vansteenkiste JF, De Leyn PR, Deneffe GJ, et al. Survival and prognostic factors in resected N2 non-small cell lung cancer: a study of 140 cases. Leuven Lung Cancer Group. Ann Thorac Surg 1997;63:1441-50. [Crossref] [PubMed]
- Okada M, Tsubota N, Yoshimura M, et al. Prognosis of completely resected pN2 non-small cell lung carcinomas: What is the significant node that affects survival? J Thorac Cardiovasc Surg 1999;118:270-5. [Crossref] [PubMed]
- Martini N, Flehinger BJ, Zaman MB, et al. Results of resection in non-oat cell carcinoma of the lung with mediastinal lymph node metastases. Ann Surg 1983;198:386-97. [Crossref] [PubMed]
- Izbicki JR, Passlick B, Hosch SB, et al. Mode of spread in the early phase of lymphatic metastasis in non-small-cell lung cancer: significance of nodal micrometastasis. J Thorac Cardiovasc Surg 1996;112:623-30. [Crossref] [PubMed]
- Riquet M, Assouad J, Bagan P, et al. Skip mediastinal lymph node metastasis and lung cancer: a particular N2 subgroup with a better prognosis. Ann Thorac Surg 2005;79:225-33. [Crossref] [PubMed]
- Tanaka F, Takenaka K, Oyanagi H, et al. Skip mediastinal nodal metastases in non-small cell lung cancer. Eur J Cardiothorac Surg 2004;25:1114-20. [Crossref] [PubMed]
- Yoshino I, Yokoyama H, Yano T, et al. Skip metastasis to the mediastinal lymph nodes in non-small cell lung cancer. Ann Thorac Surg 1996;62:1021-5. [Crossref] [PubMed]
- Prenzel KL, Baldus SE, Monig SP, et al. Skip metastasis in nonsmall cell lung carcinoma: predictive markers and isolated tumor cells in N1 lymph nodes. Cancer 2004;100:1909-17. [Crossref] [PubMed]
- Prenzel KL, Monig SP, Sinning JM, et al. Role of skip metastasis to mediastinal lymph nodes in non-small cell lung cancer. J Surg Oncol 2003;82:256-60. [Crossref] [PubMed]
- Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 2010;17:1471-4.
- Sagawa M, Sakurada A, Fujimura S, et al. Five-year survivors with resected pN2 nonsmall cell lung carcinoma. Cancer 1999;85:864-8. [Crossref] [PubMed]
- Mountain CF. Revisions in the international system for staging lung cancer. Chest 1997;111:1710-7. [Crossref] [PubMed]
- Takizawa H, Sakiyama S, Tsuboi M, et al. Demonstration of the skip metastasis pathway for N2 non-small cell lung cancer. J Thorac Cardiovasc Surg 2014;147:e50-2. [Crossref] [PubMed]
- Gou LY, Niu FY, Wu YL, et al. Differences in driver genes between smoking-related and non-smoking-related lung cancer in the Chinese population. Cancer 2015;121 Suppl 17:3069-79. [Crossref] [PubMed]
- Sun S, Schiller JH, Gazdar AF. Lung cancer in never smokers--a different disease. Nat Rev Cancer 2007;7:778-90. [Crossref] [PubMed]
- Mysikova D, Adkins I, Hradilova N, et al. Case-control study: smoking history affects the production of tumor antigen-specific antibodies NY-ESO-1 in patients with lung cancer in comparison with cancer disease-free group. J Thorac Oncol 2017;12:249-57. [Crossref] [PubMed]
- Misthos P, Sepsas E, Athanassiadi K, et al. Skip metastases: analysis of their clinical significance and prognosis in the IIIA stage of non-small cell lung cancer. Eur J Cardiothorac Surg 2004;25:502-8. [Crossref] [PubMed]
- Riquet M, Hidden G, Debesse B. Direct lymphatic drainage of lung segments to the mediastinal nodes. An anatomic study on 260 adults. J Thorac Cardiovasc Surg 1989;97:623-32. [PubMed]
- Kawano R, Hata E, Ikeda S, et al. Lobe-specific skip nodal metastasis in non-small cell lung cancer patients. Ann Thorac Cardiovasc Surg 2008;14:9-14. [PubMed]
- Benoit L, Anusca A, Ortega-Deballon P, et al. Analysis of risk factors for skip lymphatic metastasis and their prognostic value in operated N2 non-small-cell lung carcinoma. Eur J Surg Oncol 2006;32:583-7. [Crossref] [PubMed]
- Ilic N, Petricevic A, Arar D, et al. Skip mediastinal nodal metastases in the IIIa/N2 non-small cell lung cancer. J Thorac Oncol 2007;2:1018-21. [Crossref] [PubMed]


