Resurgence of therapeutically destitute tuberculosis: amalgamation of old and newer techniques
Introduction
Most of thoracic surgery developed in late 19th century and early 20th century specifically to deal with the management of tuberculosis (TB) patients (1,2). The same challenges were also encountered while dealing with various infective lung conditions. The management strategy progressed from the isolation, fresh-air sanatoria to various surgical collapse techniques to surgical resection. Surgical therapy was perfected in the mid-1950s, but subsequently declined with the emergence of effective anti-tubercular chemotherapy. Thereafter, reports of surgical intervention for TB have been extremely rare especially from the Western countries. In fact, most of the literature in thoracic surgery after 1960s deals with neoplasm of the lung, with occasional reports focussing on TB and other infective lung conditions. However, the problem of TB continued to exist in developing countries in sizable numbers. For the last five decades, caseloads of thoracic surgeons working in developing countries and recently, emerging economies, have been much higher than those working in Europe, USA and advanced countries. After globalization in 1990s, many case reports from former Soviet states, African countries, Italy, Japan, India and Pakistan are being published with regular frequency (3).
The spectre of human immune deficiency virus (HIV)-AIDS has added new dimensions, challenges and complexities in the last two decades. However, TB with or without HIV remains the single most important challenge. Since there are no randomized prospective studies, surgical recommendations for surgery are based primarily on case reports, retrospective studies, experience and consensus (1). The management of TB as well as other infective lung conditions is primarily medical, with surgery being indicated only occasionally.
Main indications for surgical intervention (2,3)
- Diagnostic procedures to confirm TB and to rule out other causes including cancer.
- Excision surgery to remove worrisome disease in drug resistant cases.
- Symptom control for conditions like haemoptysis, empyema or recurrent chest infections.
History of surgery for TB
There is a fascinating history of development of surgery for these conditions. This helps us to better understand their rationale and changing role in the present scenario. A Roman physician, Gorgio, in 1696, reported that a TB patient had improved dramatically after he suffered a sword wound in his chest, which produced a pneumothorax. This started the concept of collapse therapy. Carson, in 1822, suggested that something must be done in order to force artificially, by external means, the diseased lung to rest. Forlanini, an Italian physician, observed in 1890 that lung collapse tended to have a favourable impact on the outcome of the disease. This ended the depressing era of helplessness in the face of advanced TB and active therapy had begun. Later many other surgical procedures, e.g., artificial pneumo-peritoneum, phrenic crush, plombage, thoracoplasty and resection followed. In the postsurgical era, introduction of successful anti-tubercular chemotherapy decreased the need of surgical intervention. Most TB surgeons took to developing cardiac surgery. The need for surgery in India, on the other hand, always remained considerable because of sheer number of cases. With multi drug resistant tuberculosis (MDR-TB) and HIV, the west rediscovered interest in the subject. In the post-globalization phase, publications of interest are coming from former Soviet republics, Japan, Italy, Hungary, Turkey, Argentina, Peru, Pakistan and elsewhere (3-8).
Types of surgical procedures performed for TB (1)
There have been many surgical procedures which have been or are being currently used for diagnosis and management of TB. They can be classified as under:
- Procedures of historical interest
- Sandbag/diseased side down;
- Pneumothorax, artificial;
- Intra-pleural pneumonolysis; apicolysis (injection of air, or paraffin-oleo thorax), utilizing open or Thoracoscopic approach of Jacobaeus;
- Pneumo-peritoneum;
- Multiple intercostal neurectomies to decrease costal excursions;
- Scalenectomy to decrease upper costal excursions and to depress the lung apex;
- Phrenic nerve crush or paralysis;
- Transection of accessory muscles of respiration (scalenotomy);
- Extra pleural plombage of pneumothorax (space between parietal pleura and endo-thoracic fascia); (injection of air, nitrogen, paraffin wax);
- Sub costal and extra periosteal plombage (“bird cage”) (periosteal stripped from upper five ribs) Lucite balls used most commonly;
- Caverostomy (monaldi procedure);
- Thoracoplasty (staged).
- Diagnostic procedures
- Thoracocentesis;
- Trans thoracic needle aspiration;
- Closed/open pleural biopsy;
- Bronchoscopy (flexible/rigid), trans-bronchial needle aspiration;
- Mediastinoscopy/anterior mediastinoscopy (Chamberlain procedure);
- Thoracoscopy (video-assisted thoracic surgery);
- Exploratory/diagnostic thoracostomy-wedge biopsy.
- Therapeutic procedures
- Decortication—with or without lung resection;
- Drainage (closed/open) (temporary/permanent); pleuro-cutaneous window;
- Thoracotomy with resection;
- Segment/wedge
- Lobectomy
- Pneumonectomy (trans-pleural; extra pleural; completion)
- Chest wall/vertebral body-disc resection/stabilization;
- Muscle flaps (myoplasty);
- Thoracoplasty (modified/tailored);
- Omental transfer.
Although many of these procedures are for historical significance in the western world, some of these procedures are still being used, at least in developing countries. These procedures are tailored to address the clinical condition and scenario and form a very important part of the surgeon’s armamentarium.
Although many of these procedures are for historical significance in the western world, some of these procedures are still being used, at least in developing countries. These procedures are tailored to address the clinical condition and scenario and form a very important part of the surgeon’s armamentarium.
Summary of surgical options in different clinical conditions of TB
Persistently active disease
The decision about proper case selection is the most important one in this situation. There is a justified indication for surgery in only some of the selected cases in this category. These situations are:
- The disease is sufficiently localized;
- Adequate trial of anti-tubercular treatment (ATT) has been given;
- There has been drug failure (drug resistance);
- Patient is a chronic secretor;
- Life-threatening complications.
These are broad indications for surgery in patients having persistently sputum positive status in spite of supervised therapy. Some of these patients may be drug-resistant TB cases.
However, there are specific situations listed below where surgery is a good adjuvant in the management (3):
- When sputum smear or culture is positive for AFB, despite four to six months of appropriate and supervised ATT;
- When there have been two or more relapses;
- One or more relapse while on therapy;
- The organism has been shown to be resistant on culture and sensitivity;
- When the patient is likely to relapse in the judgment of the physician;
- Anticipated non-compliance in an admitted patient after discharge.
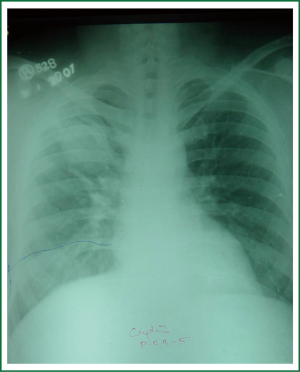
Surgery plays an important role in the overall management of MDR-TB with acceptable mortality and morbidity (9-15). Surgical interventions, in carefully selected cases, along with 2nd line ATT appears as the most favourable option since even the best available medical therapy alone only provides bacteriological cure in the order of 44-77% vis-à-vis more than 90% success rate with adjuvant surgery (12). Operative mortality is no longer a prohibitive issue, with most series reporting fewer than 3% early mortality (4,9). Though operative mortality has decreased, significant morbidity continues to be a nagging problem, broncho-pleural fistula (BPF) with empyema formation being the most distressing manifestation. In thoracic surgery, poor nutritional status and positive sputum are associated with higher rate of complications. Unequivocal consensus is lacking in the literature regarding the application of peri-operative ATT. The rationale behind selecting the exact timing of intervention needs to be logical and scientific, and whereas it appears logical to use surgery after a defined induction phase of chemotherapy, a scientifically defined induction phase has yet to be worked out. Generally accepted timing of surgery is after three months of carefully prescribed 2nd line ATT, achieving optimal bacterial suppression at the time of surgery yet avoiding delaying the surgery to a point where the bacillary load is at a perilous high. Continuation of drugs for 18-24 months postoperatively seems reasonable by most authors, though given the economics involved, completion of this task is frankly daunting, if not utopian. Indications of surgery in MDR-TB remain a contentious issue, however broad consensus is now apparent Bacteriological cure in many series has been fairly impressive, with well over 90% success achieved with adjuvant surgery. Occasionally, thoracoplasty rather than lung resection surgery is justified in some patients having bilateral disease in such a setting (Figure 1).
Hemoptysis
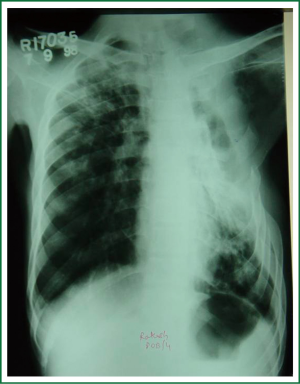
Surgery is not immediately required in cases of hemoptysis caused by pulmonary TB. Massive recurrent hemoptysis is the only justified indication in this setting. Conservative measures like positioning the good lung up after localizing the site, antibiotics, rest and sedation are almost always successful in controlling lung bleeding and surgery can be planned on an elective basis. Very often, post tubercular cavities are colonized by aspergillus fungus (aspergilloma) resulting in recurrent haemoptysis (Figure 2). There are interventional measures other than surgery, which have their selected role in appropriate situations (3):
- - Endo-tracheal intubation to secure airway, suctioning;
- - Endo-bronchial tamponade with Fogarty catheter;
- - Laser photocoagulation (Nd-yag or argon);
- - Endo-bronchial haemostatic agents;
- - Selective bronchial artery embolization.
However, surgical resection of involved portions of the lung is the most definitive and curative modality for treating massive and recurrent haemoptysis (16). These are challenging surgeries involving careful dissection because of dense and unpredictable adhesions. A properly placed double lumen endo-tracheal tube, by which the anaesthesiologist can collapse or inflate the lung depending upon the needs of the surgeon, is crucial. Position of this tube is confirmed with paediatric fibre-optic bronchoscope and the time spent here is time well spent. This also protects the other healthy lung and ensures safety during surgery. The dissection of vascular structures at hilum or in the fissure requires precise combination of sharp and blunt dissection. Adhesions are always a major challenge in this surgery. Use of a trans-fixation suture or double ligature on the proximal side while dividing arteries and veins is crucial to prevent catastrophic post operative haemorrhage. Bronchus is closed with a bronchial stump stapler or interrupted sutures. Equally good results have been shown by either of these techniques.
Empyema
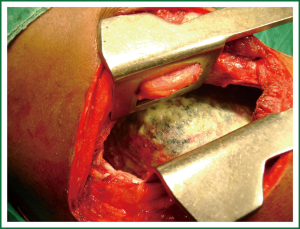
Empyema is a challenge, and requires a common sense approach, for its management (3). The management depends upon the stage of presentation. Most of the cases can be effectively managed with prolonged and expert inter-costal tube management. In the sub acute stage, drainage can be assisted by either video-assisted thoracic debridement or instillation of intra-pleural anti-fibrinolytic agents like streptokinase or urokinase. Decortication is indicated in persistent pleural spaces with late fibrino-purulent stage. Thoracoplasty is partial decostalization of the thoracic cage to obliterate persistent pleural space. Whenever lung is unlikely to expand because of extensive disease or multiple BPF, thoracoplasty is an appropriate intervention (Figure 3) and is required quite often in our setting. Post operative empyema or persisting space problems almost always require thoracoplasty for ultimate resolution.
Other procedures
Open window thoracostomy
Eloesser described a procedure to establish long term open drainage of chronic empyema cavities in 1935. The procedure basically involves creating an open window thoracostomy in the chest wall for facilitating long term open drainage without the need for an indwelling catheter. Various modifications of the procedure have been developed and described in the literature. It is an excellent procedure, the efficacy of the procedure in the management being matched by the beauty of its simplicity. Two to three ribs overlying the empyema cavity in the axillary region are partially resected and the underlying pleura is sutured with the skin using interrupted sutures. With good drainage being established, the empyema cavity slowly heals and many a times closes over a period of months. Kohli and colleagues described complete expansion of lung in 56% of 50 patients treated with open window thoracostomy over a period of 3 to 24 months after creating the flap (17) (Figure 4). Any patient of chronic empyema in whom the lung has not expanded after an adequate period of closed chest tube drainage and who is judged to be not suitable for decortication because of diseased underlying lung can be managed with this procedure with excellent results.
Bronchoscopy
Both rigid and fibre-optic bronchoscopy are excellent procedures and every thoracic surgeon should be able to perform them well. It is required in pre-operative evaluation prior to all these surgical operations. Sometimes, bronchoscopy is needed in post-operative period to remove thick secretions or blood clots from the tracheo-bronchial tree.
Mediastinoscopy
It is required less often nowadays. However, a mediastinal lymphadenopathy, which can be TB, sarcoidosis or lymphoma, is a perplexing clinical situation and if other measures fail to show a conclusive diagnosis, mediastinoscopy is a justified.
Adjuncts to surgery
Pre-operative work up of a thoracic surgical patient
There are some well-established pre-requisites before a patient is taken up for surgery. It is of utmost importance that a detailed discussion is held with the patient and his relatives. This should include an open talk about the natural course of the disease in the absence of any surgical intervention and the exact aim and objective of the proposed surgery in a given case. Risks of surgery and anaesthesia are carefully explained and also the short term and long term results, if surgery is successful. It is of vital importance that a patient of pulmonary TB has taken an adequate course of ATT before the surgical decision is taken. Even an episode of massive hemoptysis as a presenting feature of pulmonary TB in a non-treated case is rarely an indication of surgical intervention. Patient’s cardio-respiratory reserve to withstand surgery of this magnitude or proposed lung resection is carefully assessed. Various criteria have been laid down for different surgeries and decision should be made jointly by the thoracic surgeons and the chest physician about the fitness of a given case after taking into account all the factors. Patients are urged to stop smoking at least three weeks before surgery in order to ensure better post-operative results. Post-operative physiotherapy exercises like deep breathing, coughing and shoulder exercises are taught to the patient in the pre-operative period while forewarning him or her about a certain amount of expected post-operative pain. The patient should be as ‘dry’ as possible before surgery, meaning thereby that sputum or pus production (in cases of empyema) should be minimized by appropriate measures like antibiotics, postural drainage, respiratory exercises, steam inhalation and nebulizers etc. Some of these patients are quite weak and depleted nutritionally. Their nutritional status is built up before surgery by rest and adequate diet ensured by hospitalization.
Post-operative management
Results in surgery for TB and inflammatory lung disease improve if attention to detail is given in post-operative period. Initial management is ideally done in an Intensive Care Unit (ICU). Antibiotics and painkillers are routinely given. Blood is transfused as per requirements. Respiratory exercises should be encouraged and all measures to relieve pain should be taken. Incentive spirometry is a useful tool to achieve these aims. Care of the chest tubes is an essential ingredient of this care and they should be removed only when their output has minimised sufficiently. Persistent air leaks, development of BPF, residual pleural space are the most important issues to be watched for in the post-operative period and onwards. These complications may require various kinds of intervention, including open window thoracostomy and thoracoplasty.
Results after surgery for pulmonary tuberculosis
Recent published series have demonstrated mortality ranging from 0% to 3.1% (3,4,18-22). Morbidity reported in most series ranges from 3% to 53.7%. Postoperative empyema and BPF are best managed by prolonged tube drainage followed by open-window thoracostomy and thoracoplasty, if required.
Conclusions
Surgery for complications and sequel of pulmonary TB still remain an important intervention for alleviation of human misery. It is a high cost and sophisticated intervention, which demands high levels of surgical skill and judgment. There is a continued need to further develop skills and techniques in this area. All these issues require continued commitment from all the stakeholders to improve the results of this highly complicated and complex set of surgical patients (3).
Use of newer technologies like surgical staplers, refined blood transfusion technologies, argon beam coagulation, monitoring devices and safer anaesthesia have improved the results of surgery substantially. The number of surgeons engaged in this specific field of pathology has declined tremendously with the advent of ATT. The ravages of TB are on the rise again especially since drug resistant TB has come to the fore. This calls for a dire need to re-invent the wheel of TB-surgery to adequately address this health hazard. The amalgamation of the older TB surgical techniques with the current developments of surgery in general, is needed.
References
- Pezzella AT, Fang W. Surgical aspects of thoracic tuberculosis: a contemporary review--part 1. Curr Probl Surg 2008;45:675-758. [PubMed]
- Pezzella AT, Fang W. Surgical aspects of thoracic tuberculosis: a contemporary review--part 2. Curr Probl Surg 2008;45:771-829. [PubMed]
- Dewan RK. Surgery for pulmonary tuberculosis - a 15-year experience. Eur J Cardiothorac Surg 2010;37:473-7. [PubMed]
- Takeda S, Maeda H, Hayakawa M, et al. Current surgical intervention for pulmonary tuberculosis. Ann Thorac Surg 2005;79:959-63. [PubMed]
- Treasure RL, Seaworth BJ. Current role of surgery in Mycobacterium tuberculosis. Ann Thorac Surg 1995;59:1405-7; discussion 1408-9. [PubMed]
- Chiang CY, Yu MC, Bai KJ, et al. Pulmonary resection in the treatment of patients with pulmonary multidrug-resistant tuberculosis in Taiwan. Int J Tuberc Lung Dis 2001;5:272-7. [PubMed]
- Shiraishi Y, Nakajima Y, Katsuragi N, et al. Resectional surgery combined with chemotherapy remains the treatment of choice for multidrug-resistant tuberculosis. J Thorac Cardiovasc Surg 2004;128:523-8. [PubMed]
- Somocrsio J, Sotomayor A, Furin J, et al. Identifying a subset of MDR-TB with bilateral pulmonary disesase suitable for adjunctive thoracic surgery. website and personal communication
- Pomerantz M, Brown JM. Surgery in the treatment of multidrug-resistant tuberculosis. Clin Chest Med 1997;18:123-30. [PubMed]
- Sharma SK, Mohan A. Multidrug-resistant tuberculosis. Indian J Med Res 2004;120:354-76. [PubMed]
- Dewan RK, Pratap H. Surgical interventions in multi-drug resistant tuberculosis: Retrospective analysis of 74 cases treated at a tertiary care level institution. Ind J Thorac Cardiovas Surg 2006;22:15-8.
- Loddenkemper R, Sagebiel D, Brendel A. Strategies against multidrug-resistant tuberculosis. Eur Respir J Suppl 2002;36:66s-77s. [PubMed]
- MDR-TB Fact sheet, March 2005 American Lung Association.
- Iseman MD, Madsen L, Goble M, et al. Surgical intervention in the treatment of pulmonary disease caused by drug-resistant Mycobacterium tuberculosis. Am Rev Respir Dis 1990;141:623-5. [PubMed]
- Sharma SK, Mohan A. Multidrug-resistant tuberculosis. Indian J Med Res 2004;120:354-76. [PubMed]
- Corey R, Hla KM. Major and massive hemoptysis: reassessment of conservative management. Am J Med Sci 1987;294:301-9. [PubMed]
- Kohli A, Singh G, Vig A, et al. Pleurocutaneous flap: how useful it is in management of chronic empyema. Indian J Chest Dis Allied Sci 2006;48:257-9. [PubMed]
- Naidoo R. Active pulmonary tuberculosis: experience with resection in 106 cases. Asian Cardiovasc Thorac Ann 2007;15:134-8. [PubMed]
- Souilamas R, Riquet M, Barthes FP, et al. Surgical treatment of active and sequelar forms of pulmonary tuberculosis. Ann Thorac Surg 2001;71:443-7. [PubMed]
- Furák J, Troján I, Szöke T, et al. Surgical intervention for pulmonary tuberculosis: analysis of indications and perioperative data relating to diagnostic and therapeutic resections. Eur J Cardiothorac Surg 2001;20:722-7. [PubMed]
- Olcmen A, Gunluoglu MZ, Demir A, et al. Role and outcome of surgery for pulmonary tuberculosis. Asian Cardiovasc Thorac Ann 2006;14:363-6. [PubMed]
- Kim YT, Kim HK, Sung SW, et al. Long-term outcomes and risk factor analysis after pneumonectomy for active and sequela forms of pulmonary tuberculosis. Eur J Cardiothorac Surg 2003;23:833-9. [PubMed]