Is laryngeal mask airway general anesthesia feasible for minimally invasive esophagectomy?
Introduction
Esophagectomy is the cornerstone of the curative treatment of esophageal carcinoma. In the two decades, minimally invasive esophagectomy (MIE) has emerged as an oncological approach with lower mortality and morbidity. Traditionally, thoracoscopic operations are performed under general anesthesia with double-lumen endotracheal intubation and single-lung ventilation. However, conventional general anesthesia may result in numerous adverse effects, such as airway trauma associated with the double-lumen endotracheal tube, ventilator-induced lung injury, and cognitive dysfunction, especially in susceptible elderly patients (1-3). In recent years, some studies indicate that thoracoscopic operations without tracheal intubation can be used for numerous diseases, including pneumothorax, resection of pulmonary nodules, resection of solitary metastases, lung volume reduction and resection of pulmonary lobectomy, to avoid tracheal intubation and associated anesthesia complications (4,5). Here, we report the tentative application of laryngeal mask airway (LMA) anesthesia for MIE procedure in our institution.
Case presentation
Three patients with esophageal carcinoma underwent MIE using non-intubation anesthesia approach via LMA in December of 2012. The three patients were selected carefully: besides regular preoperative test, MVV%, FEV1 and DLCO must be above 70%, 1.6 L/s and 75%. And they must had no cardiac disease history and with normal ECG. Before operation, communication with patients was performed on the anesthesia approach and consent forms were signed.
All the patients were pre-medicated with 50 mg of fentanyl intravenously, and electrocardiography (ECG), oxyhemoglobin saturation, respiratory rate, blood pressure, central venous pressure (CVB) and arterial blood gas analysis were monitored during the MIE procedure. Sedation was then started by intravenous administration of propofol (10 mg/mL) using a target controlled infusion method, with incremental fentanyl injection to maintain the patients in a mildly sedation. During the procedure, atracurium will be added as the manipulation needed and the patients breathed oxygen through LMA and ventilator (tidal volume 5 mL/kg, respiratory rate 18–25/min, FiO2 1.0) to keep oxygen saturation above 90%.
All the patients underwent MIE (two-field lymph nodes dissection) with extracorporeally gastric conduit creation and two-layer hand-sewn cervical esophagogastric anastomosis. During the thoracic phase of MIE procedure, the patient was put in semi-prone position (left lateral decubitus position with 30° forerake) and artificial CO2 pneumothorax (intrathoracic CO2 pressure =8 mmHg) was established. Following that, the patient was put in supine position and the stomach was dissected and made into a gastric tube. The MIE procedure was performed without pyloroplasty.
Results
Three selective patients (2 males, 1 female) at the age of 58, 53 and 65 respectively underwent MIE. Their general clinical data is showed in Table 1. In all cases, the lung of operation side collapsed partly and the visualization was satisfied. Atracurium was needed to be used as the manipulation needed. MIE manipulation and lymph nodes resection were easily performed during the procedure. The number of dissected in the operation is equal as usual and the operative time and the bleeding volume did not increase than that in the procedure using intubation. So, technical feasibility was considered excellently in all cases. Intraoperative laryngeal mask displacement occurred in one patient because of the cervical esophageal traction and the position of head during anastomosis procedure. But the SPO2 was stable and above 90% because the anesthetist observed this condition and modified the LMA position timely. And the monitoring index was showed in Table 2, which indicated that patients’ physical signs were stable during the operation. The information of Table 1 reveals the detailed perioperative surgical data, which indicated that there were no postoperative complications occurred and all of three patients were discharged smoothly. After 18-month follow-up, the three patients are alive without recurrence and other complications related to operation.
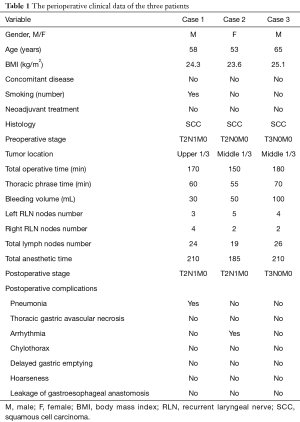
Full table
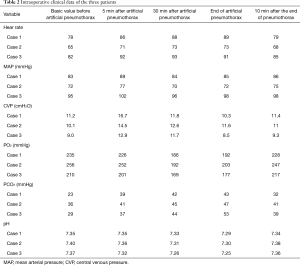
Full table
Discussion
General anesthesia using double-lumen intubation with one-lung ventilation is the standard approach for MIE. However, it may be associated with potential complications related to tracheal intubation and one-lung ventilation. Our team is hammering at fast track surgery of esophageal carcinoma. We have strived for many procedures, including MIE, single-lumen endotracheal intubation anesthesia with two lung ventilation, early oral feeding, shortened postoperative drainage time and nasogastric tube maintain time, to decrease the harmful effect of perioperative iatrogenic manipulation. Non-intubation anesthesia may avoid the potential complications that the intubation may result in, and may be helpful to judge the reason of postoperative hoarseness. The recent study indicated that VATS can be performed with thoracic epidural anesthesia and intrathoracic vagal blockade (6). However, this approach has the potential risk related to epidural hematoma or spinal cord injury. At the same time, Ambrogi and his colleagues successfully applied LMA in VATS for spontaneous pneumothorax (7). So, we reasoned that the application of LMA in MIE could avoid the potential complications of intubation general anesthesia or epidural anesthesia. Despite the displacement of LMA in one patient and a slight increase of the pressure of CO2, the changes of intraoperative index were acceptable and there were no serious complications occurred after operation. The data of the three patients in this study suggests that MIE can be feasibly and safely performed with general anesthesia through the use of LMA. During the MIE thoracic procedure, the patients were put in a semi-prone position and artificial pneumothorax with intrathoracic pressure of 8 mmHg was established. The lung almost underwent a complete deflation because of its gravity and pneumothorax. Therefore, the operating space is adequate for thoracoscopic manipulation. During the MIE thoracic procedure, there was no cough reflex that could hamper the surgical dissection for esophagus and lymph nodes. Nevertheless, this happened in 14% of cases with awake epidural technique, which was described in the study of Pompeo and colleagues (8). During the abdominal procedure, adequate muscle relaxant is necessary for accessing the available surgical manipulating space.
The main problems of using LMA in MIE procedure are the displacement of LMA and management of airway. There was one patient of the three got pneumonia and he just was the one whose LMA displaced in the MIE procedure. We think that careful observation of anesthetist could avoid the displacement of LMA and aspiration. So, the anesthetist needs to pay more attention to prevent the displacement of LMA and aspiration. Additionally, the patients in this study are carefully selected. Even then, our first experience reveals that LMA could be safely used for MIE without the risks associated with intubation. On the basis of our preliminary experience, it is surmised that LMA general anesthesia can be used for more patients with some comorbidities, for whom its advantages would be even more considerable.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patients for publication of this manuscript.
References
- Murphy GS, Szokol JW, Avram MJ, et al. Postoperative residual neuromuscular blockade is associated with impaired clinical recovery. Anesth Analg 2013;117:133-41. [Crossref] [PubMed]
- Fitzmaurice BG, Brodsky JB. Airway rupture from double-lumen tubes. J Cardiothorac Vasc Anesth 1999;13:322-9. [Crossref] [PubMed]
- Gothard J. Lung injury after thoracic surgery and one-lung ventilation. Curr Opin Anaesthesiol 2006;19:5-10. [Crossref] [PubMed]
- Inoue K, Moriyama K, Takeda J. Remifentanil for awake thoracoscopic bullectomy. J Cardiothorac Vasc Anesth 2010;24:386-7. [Crossref] [PubMed]
- Noda M, Okada Y, Maeda S, et al. Successful thoracoscopic surgery for intractable pneumothorax after pneumonectomy under local and epidural anesthesia. J Thorac Cardiovasc Surg 2011;141:1545-7. [Crossref] [PubMed]
- Chen JS, Cheng YJ, Hung MH, et al. Nonintubated thoracoscopic lobectomy for lung cancer. Ann Surg 2011;254:1038-43. [Crossref] [PubMed]
- Ambrogi MC, Fanucchi O, Gemignani R, et al. Video-assisted thoracoscopic surgery with spontaneous breathing laryngeal mask anesthesia: preliminary experience. J Thorac Cardiovasc Surg 2012;144:514-5. [Crossref] [PubMed]
- Pompeo E, Mineo D, Rogliani P, et al. Feasibility and results of awake thoracoscopic resection of solitary pulmonary nodules. Ann Thorac Surg 2004;78:1761-8. [Crossref] [PubMed]


