Total thoracoscopic high-position sleeve lobectomy of the right upper lobe of the lung
Introduction
Total thoracoscopic lobectomy with systematic lymphadenectomy is a well-documented and widely used procedure. With continuous improvement of minimally invasive techniques and instruments, the indications of thoracoscopic surgery have been expanded based on the concept of anatomical resection. In 2002, Santambrogio et al. (1) reported the first endoscopic bronchial sleeve resection and bronchoplasty. However, due to the difficulty of operation and high surgical risk, this procedure has not been rapidly popularized in clinical practice. In addition, no agreement has been reached regarding indications, incision design, and bronchial anastomotic methods. Based on the skills and experience with thoracoscopy and thoracotomy in our center, we performed total thoracoscopic surgeries to treat patients with central lung cancer. The surgical procedure and the short-term prognosis were satisfactory.
In this case study, a 50-year-old man preoperatively diagnosed with central squamous cell carcinoma of the right upper lobe underwent a successful total thoracoscopic high-position sleeve lobectomy of the right upper lobe via the “three-port approach”.
Surgical technique
A 50-year-old man was admitted to the hospital due to a 2-month history of coughing. Chest CT scan revealed a mass of the right upper lung near the lung hilum, atelectasis of right upper lobe, and enlarged right hilar lymph nodes. No significantly enlarged mediastinal lymph node was noted. Bronchoscopy revealed occlusion of the right upper lobe bronchus by the tumor. The pathological examination of the obtained biopsy reveled squamous cell carcinoma. The required preoperative examinations were completed, and no distant metastasis was evident. Total thoracoscopic sleeve resection of the right upper lobe was performed (Figure 1). This video demonstrates the entire procedure of sleeve lobectomy of the right upper lobe, including mediastinal lymph node dissection, anatomical right upper lobectomy, and right upper lobe bronchial sleeve anastomosis.

General anesthesia was administered with dual-lumen endotracheal intubation and ventilation of the non-affected lung. The patient was placed in a lateral recumbent position on his left side with soft pillow support under his waist. The “three-port approach” was used for the procedure. A 1-cm incision was made at the right axillary midline in the seventh intercostal space as the observation channel. A 3-cm incision was made at the right anterior axillary line in the fourth intercostal space as the main operating channel. A 1-cm incision was made at the right subscapular angle line in the seventh intercostal space to assist the instruments. The surgeon stood at the front side of the patient; the thoracoscope operator and first assistant stood at back side of the patient.
The thoracoscope was used for exploration. Chest adhesions were separated. Implantation metastasis was excluded. The procedure was performed step-by-step clockwise. Lymphadenectomy and lobectomy were simultaneously performed.
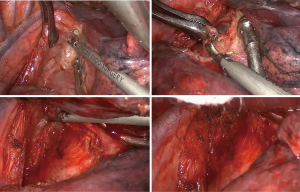
Inferior pulmonary ligament region (Figure 2)
The lower right lung lobe was retracted superiorly. An electrical hook or ultrasonic scalpel was used to incise the plural membrane from the inferior pulmonary ligament to the lower edge of the inferior pulmonary vein. The lymph nodes along the inferior pulmonary ligament (Station 9) were removed. The lower edge of the inferior pulmonary vein was sufficiently exposed.
Subcarinal region (Figure 3)
The right lung was retracted anteriorly to expose the posterior mediastinum, and the mediastinal pleura was incised from the level of the inferior pulmonary veins to the lower margin of the arch of the azygos vein. An electric hook and ultrasonic knife were used alternatively to excise the esophageal bronchial arteries and the perforating branches along the lateral side of the esophagus until visualization of the left main bronchus and the esophagus in the deep and posterior operative fields, respectively, was achieved. Then, along the posterior right main bronchus, the dissection continues from the proximal middle bronchus toward the carina until the level of carinal bifurcation at which the perforating branches of bronchial artery were divided. Thus, the subcarinal and lower paraesophageal lymph nodes were completely removed.
Interlobar region (junctional region between right upper lobe and the intermediate bronchus) (Figure 4)
The right upper lobe was retracted toward the top of the chest and the right middle and lower lobes toward the diaphragm to expose the junctional region between the upper right lobe and intermediate bronchus. An electric hook and ultrasonic knife were used alternatively to continue the dissection along the right middle bronchus toward the junctional region until the lymph nodes in this region appear mobile from the adjacent posterior bronchus. The lymph nodes in this area were not resected at this time.
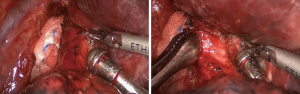
Superior mediastinal region (Figure 5)
The upper right lobe was retracted downward to expose the superior mediastinum. An inversed “T”-incision was made above the arch of the azygos vein and anterior to the vagus nerve to incise the superior mediastinal pleura. First, the lymph nodes and surrounding tissue were dissected along the posterior superior vena cava to the level of posterior right innominate vein. Then, the lymph nodal tissue in this region was retracted upward. The dissection continued inferiorly through the space posterior to the arch of the azygos vein to the level of the anterior carina. Then, the deep sides of the lymphatic and adipose tissues between the venous cava and trachea were mobilized superiorly and excised at the level of posterior right innominate vein. Then, these lymph nodes were retracted and dissected from the anterior trachea until the level of the right subclavian artery. The lymph nodes in this region were completely removed using this procedure.
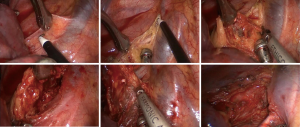
Hilar and lobar region (Figure 6)
Hilar lymph node dissection and lobectomy methods are consistent with those described in the literature. First, the mediastinal pleura anterior and superior to the hilum were incised. The right upper pulmonary vein was mobilized from the vascular sheath and divided by a single-use stapler. The dissection continues superiorly to separate the right upper anterior-apical pulmonary artery, which was divided using a single-use stapler. Then, dissection of the distal pulmonary truncus was initiated. Along with the surface of the pulmonary truncus, a horizontal fissure was dissected and divided by a single-use stapler. Then, the posterior ascending branch of the pulmonary artery became visible and was double ligated by 7- and 4-silk sutures. Then, an ultrasound scalpel was used to divide the artery from the distal end. Then, along with the distal posterior ascending artery, the interlobar tissue can be easily divided to enter the previously exposed junctional region between the right upper lobe and the middle bronchus. The posterior oblique fissure can be divided by the single-use stapler. The right upper lobe was retracted, and the lymph nodes around the right main bronchus, right upper lobe bronchus and right middle bronchus were removed. With the exception of the right upper bronchus, the right upper lobe was completely separated from other structures, i.e., skeletonization of the bronchus.
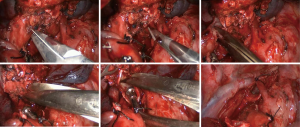
Bronchial resection (Figure 7)
The skeletonized right upper lobe bronchus was retracted. A pointed tip scalpel was used to incise the targeted site of the right middle bronchus and the right main bronchus. Then, endoscopic scissors were used to divide the middle bronchus followed by the right main bronchus, while the right upper lobe was retracted. The bronchial stumps were trimmed. The proximal and distal margins of the bronchus were sent for frozen section. A confirmation of no visible cancer cells in the margin tissue indicates the completion of sleeve resection.
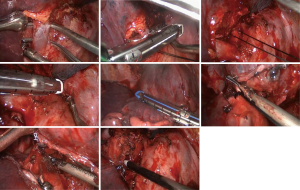
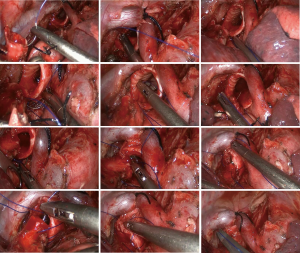
Bronchial anastomosis (Figure 8)
After confirmation of negative margins, bronchial anastomosis was performed using 3-0 prolene sutures with double-armed sutures. In this case, the right main bronchial resection range was long; therefore, the azygos arch needed to be retracted to facilitate visualization for the next step of anastomosis. The first stitch started at the junction between the membrane and the cartilage. The suture pattern was as follows: the needle entered the edge of one bronchial stump wall in external-internal manner and exited the edge of the other bronchial stump wall in internal-external manner. When tying the suture, the proximal and distal bronchial stumps were brought together. The knot was tied outside the bronchial lumen. One needle was introduced out of the main operating port, and the suture was tightly attached to the drape for use in the next step. The other needle was used to posteriorly suture the bronchial membrane in a continuous pattern. At the end of the membrane suture, this needle was introduced out of the assisting port, and the suture was tightly attached to the drape for use in the next step. Then, the needle in the main operating port was used again from posteriorly to anteriorly to continually suture bronchial cartilage parts, including the medial, anterior and lateral walls, until reaching the other junction between the membrane and cartilage. Then, the sutures in the main and assisting ports were tightly knotted. Thus, the bronchial anastomosis was completed. A small amount of saline was injected into the thoracic cavity. Leakage of the anastomosis assessed using saline with expansion of the lung by the anesthesiologists. The leakage of the anastomosis was evaluated at 30 cmH2O of airway pressure. No sign of the anastomotic leakage was noted in this case.
The operative time was 200 minutes. The intraoperative blood loss was 200 mL. The procedure was uneventful. The drainage tube was removed on postoperative day 5, and the patient was discharged on postoperative day 7. The postoperative pathological stage was T4N1M0 (stage IIIA).
Discussion
The delicate design of the surgical procedure served as the basis to simplify and expedite the procedure with quality assurance. We believed that the key to simplify this type of procedure is to remove mediastinal and hilar lymph nodes at the beginning. Anatomical lobectomy is then performed to achieve “skeletonization” of the bronchus that is prepared for sleeve resection. Then, bronchial sleeve resection and anastomosis were performed. This operating pattern can significantly reduce the surgical difficulty. Bronchial anastomosis is the rate-limiting step of this procedure. Currently, endoscopic bronchial anastomosis methods include intermittent (3,4), continuous (5-7), and continuous mixed with intermittent (8,9) sutures. Intermittent suturing is relatively reliable in theory, but interrupted suturing is more easily achieved due to multiple sutures in the thoracic cavity. Moreover, repeated knotting during interrupted suturing can significantly prolong the operative time. Regarding continuous suturing, tightening the suture at the end may not avoid interference with the loose suture, which can still affect the suture speed. Our experience is as follows: 3-0 prolene sutures (single suture with double needles) can be used for bronchial anastomosis. The suture should be maintained with tension during the operation; the needles should be introduced out of the thoracic cavity via the main or assisting port to avoid suture complications during surgery and ensure reliable anastomosis. In addition, the use of dual-lumen endotracheal intubation can achieve a good single lung isolation and ensure better exposure of the operative field.
Acknowledgements
Funding: This work was financed by Grant-in-aid for scientific research from the Natural Science Foundation for the Youth of Hunan province of China (No. 2018JJ3314).
Footnote
Conflicts of Interest: This video was granted the Award of Great Potential in the 2017 Master of Thoracic Surgery—Video-assisted Thoracoscopic Surgery Video Contest.
Informed Consent: Informed consent was obtained from the patient.
References
- Santambrogio L, Cioffi U, De Simone M, et al. Video-assisted sleeve lobectomy for mucoepidermoid carcinoma of the left lower lobar bronchus: a case report. Chest 2002;121:635-6. [Crossref] [PubMed]
- Yang D, Zhou Y, Wang W. Total thoracoscopic sleeve resection of the right upper lobe was performed. Asvide 2018;5:647. Available online: http://www.asvide.com/article/view/26156
- Mahtabifard A, Fuller CB, McKenna RJ Jr. Video-assisted thoracic surgery sleeve lobectomy: a case series. Ann Thorac Surg 2008;85:S729-32. [Crossref] [PubMed]
- Agasthian T. Initial experience with video-assisted thoracoscopic bronchoplasty. Eur J Cardiothorac Surg 2013;44:616-23. [Crossref] [PubMed]
- Huang J, Li S, Hao Z, et al. Complete video-assisted thoracoscopic surgery (VATS) bronchial sleeve lobectomy. J Thorac Dis 2016;8:553-74. [Crossref] [PubMed]
- Han Y, Zhou S, Yu D, et al. Video-assisted thoracic surgery (VATS) left upper sleeve lobectomy with partial pulmonary artery resection. J Thorac Dis 2013;5 Suppl 3:S301-3. [PubMed]
- Liu K, Jin C, Tian H, et al. Total video-assisted thoracic surgery sleeve lobectomy: suture by both hands. Thorac Cardiovasc Surg Rep 2013;2:43-5. [Crossref] [PubMed]
- Li Y, Wang J. Video-assisted thoracoscopic surgery sleeve lobectomy with bronchoplasty: an improved operative technique. Eur J Cardiothorac Surg 2013;44:1108-12. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fernandez R, Fieira E, Rellan L. Uniportal video-assisted thoracoscopic bronchial sleeve lobectomy: first report. J Thorac Cardiovasc Surg 2013;145:1676-7. [Crossref] [PubMed]