Subxiphoid video-thoracoscopy
Introduction
Pleural effusion is an excessive accumulation of fluid in the pleural space. Pleural effusion is not a disease properly speaking, but rather a reflection of underlying abnormalities related to a wide variety of lung, pleural and systemic disorders. To elucidate the aetiology of pleural effusion is crucial to treat it correctly (1).
Asian surgeons described the subxiphoid approach as a useful access to the chest in numerous procedures (2). Subxiphoid pericardioscopy (3), coronary operations, resection of the thymus (4), ablative sympathectomy, pulmonary wedge resection and lobectomies (5) have been described.
Subxiphoid video-thoracoscopy is a minimally invasive technique. Through a single incision right and left mediastinal pleura can be identified and incised. This enables the introduction of a video-thoracoscopy through the open valves of the video-mediastinoscope and into the pleural cavity. With the 30° video-thoracoscopy the pleural cavity can be explored and samples of fluid, lesions of parietal and visceral pleura and lung nodules can be identified and biopsied.
This technique is especially indicated in two situations: (I) in cases where a bilateral pleural effusion is identified. The subxiphoid approach allows us to explore both pleural cavities at the same time through a single incision (6); (II) in critically ill patients who can not tolerate lateral decubitus due to a large amount of pleural or pericardial effusion, this procedure is an alternative to be taken into account.
Surgical technique
Preoperative studies, anaesthetic considerations and patient’s position
Medical history is important to rule out previous pleural diseases, such as empyema. Computed tomography of the chest has to be carefully studied before the surgical procedure in patients with pleural effusion. Previous infectious pleural disease may render the procedure impossible because of the adhesions in the pleural cavity. Coagulation tests should be within normal limits.
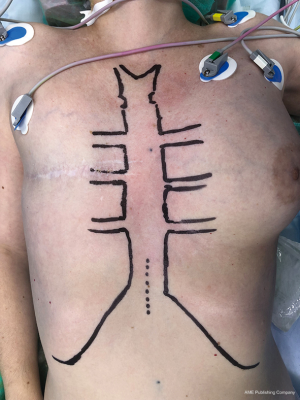
The technique is performed under general anaesthesia with a double-lumen tube to allow single-lung ventilation. The patient is positioned supine on the operating table with a sandbag placed at the level of the xiphoid (Figures 1,2).
Instrumentation
The Linder-Dahan spreadable video-mediastinoscope (Richard Wolf, Knittlingen, Germany) is used because it enlarges the operative field. Regarding instrumentation, the same standard mediastinoscope instruments can be used, such as dissection-suction-coagulation cannula, grasping forceps, endoscopic scissors, biopsy forceps, and endoscopic clipping devices (Figure 3).
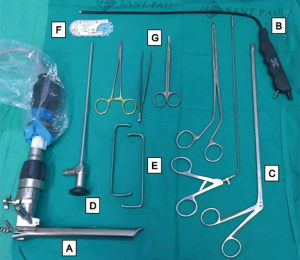
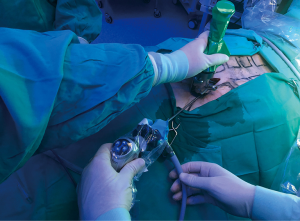
A 30o video-thoracoscopy is used to explore the entire pleural cavity. The same forceps used for mediastinoscope can be used to perform biopsies of parietal pleura. A suction cannula is used to take samples of pleural effusion if it is present.
Surgical procedure
Incision (Figure 4)

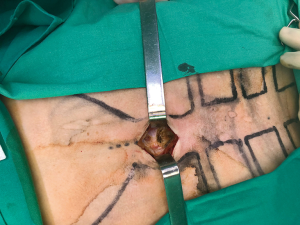
A vertical incision of about 3 cm is performed over the xiphoid (Figure 5). The xiphoid can be removed if it is necessary.
Introduction of the video-mediastinoscope (Figure 6)

Dissection of the subcutaneous tissue is carried out laterally and the insertion of rectus abdominis is divided. The mediastinoscope is introduced to dissect and create a subcostal tunnel under direct vision. The substernal angle between the xiphoid process and the subcostal margin is identified. The right-side mediastinal pleura is identified and grasped with forceps and incised. Samples of fluid are taken for cytopathological studies and cultures. Pleural fluid is completely drained with suction.
Subxiphoid video-thoracoscopy (Figure 7)

The ipsilateral lung is collapsed and a 5-mm 30-degree video-thoracoscopy is inserted through the valves of the video-mediastinoscope (Figure 8). We prefer a video-mediastinoscope to provide an optimal exposure and avoid a sternal lifter. A wound protector can be used instead of video-mediastinoscope. The pleural cavity is explored and biopsies of the parietal, visceral and diafragmatic pleura and lung nodules can be performed.
Talc pleurodesis (Figure 9)

If malignancy is confirmed by frozen-section or by macroscopic evidence of intrapleural tumour infiltration or implants, a pleurodesis can be performed.
Chest tube (Figure 10)

After the procedure, a 28-F chest tube is inserted through the video-mediastinoscope. After a complete lung re-expansion is confirmed, the video-mediastinoscope is removed, the chest tube is fixed and the incision is closed in layers.
Discussion
The subxiphoid approach was introduced in the 1970’s for the diagnoses and treatment of pericardial effusions including haemopericardium in patients with heart trauma and pericarditis (12). The subxiphoid video-thoracoscopy is a variant of uniportal video-assisted thoracoscopic surgery (VATS) approach without opening the intercostal space. It can be combined with other minimally invasive incisions like intercostal or subcostal VATS ports, or the transcervical incision. In case of oesophageal resection, it can be combined with laparoscopy (13).
At present, it is gaining a special importance for thymectomy and minimally invasive uniportal VATS procedures like resections of other mediastinal tumours or metastases, cardiac procedures (14,15), thoracic sympathectomy (6), laparoscopic diaphragmatic hernia repair (16), oesophageal resections (17), surgery for primary spontaneous pneumothorax (18) and pulmonary resections (19).
Although this approach can offer different utilities, the purpose of this article is to emphasize its role in diagnoses and treatment of pleural effusion, because to elucidate the aetiology of pleural effusion is crucial to treat it correctly. With this approach, both mediastinal pleura can be identified and incised through a single incision. This enables the introduction of a video-thoracoscopy through a subxiphoid approach. We prefer to use a video-mediastinoscope to enlarge the operative field and then a 30° video-thoracoscopy is introduced through the open valves of the video-mediastinoscope and into the pleural cavity. With the 30° video-thoracoscopy, the pleural cavity can be explored and samples of fluid, lesions of parietal and visceral pleura and lung nodules can be identified and biopsied. If malignancy is confirmed by frozen-section or by macroscopic evidence of intrapleural tumour infiltration or implants, a pleurodesis to avoid recurrence can be performed prior to chest tube insertion and closure. Although many agents can be used, magnesium sulphate (talc) is effective and cheap (20).
In cases with unilateral or bilateral pleural effusion with or without pericardial effusion, lateral decubitus could not be well tolerated. The subxiphoid video-thoracoscopy allows the exploration of both pleural cavities and pericardium in the supine decubitus, a point to have in mind in critically ill patients (21).
Several studies have compared the intensity of self-reported postoperative pain and chest wall neuralgia between patients who underwent single-incision thoracoscopic surgery and those who underwent multiple-incision thoracoscopic surgery (22). In some of those studies, acute postoperative pain was reported. Nonetheless, even small chest wall incisions cause intercostal neuralgia and can result in chronic pain (23). Contrary to traditional thoracoscopy, subxiphoid video-thoracoscopy does not require intercostal incisions and, thus, it avoids potential injury to the intercostal nerves and subsequent intercostal neuralgia (24).
The exploration of the posterior mediastinum is limited by the subxiphoid approach. To control an important bleeding by the subxiphoid approach could be difficult (25). When an emergency conversion is necessary, an extension of the subxiphoid incision is unlikely to be useful and additional standard VATS or opened approach must be performed (2).
Conclusions
In conclusion, subxiphoid video-thoracoscopy is efficient and safe to study pleural effusions with an unknown aetiology. A single incision will be able to answer many questions about diagnosis, staging and prognosis, and probably decreases the risk of postoperative pain.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Karkhanis VS, Joshi JM. Pleural effusion: diagnosis, treatment, and management. Open Access Emerg Med 2012;4:31-52. [Crossref] [PubMed]
- Terzi A, Viti A. Subxiphoid video-assisted major lung resections: the skeptic’s speech. J Thorac Dis 2016;8:E1741-2. [Crossref] [PubMed]
- Trujillo-Reyes JC, Rami-Porta R, Caja SC, et al. Subxiphoid video-pericardioscopy. Multimed Man Cardiothorac Surg 2015;2015. [Crossref] [PubMed]
- Zielinski M, Rybak M, Solarczyk-Bombik K, et al. Subxiphoid uniportal VATS thymectomy. J Vis Surg 2017;3:171. [Crossref] [PubMed]
- Liu CC, Wang BY, Shih CS, et al. Subxiphoid single incision thoracoscopic left upper lobectomy. J Thorac Cardiovasc Surg 2014;148:3250-1. [Crossref] [PubMed]
- Chen JT, Liao CP, Chiang HC, et al. Subxiphoid single-incision thoracoscopic bilateral ablative sympathectomy for hyperhidrosis. Interact Cardiovasc Thorac Surg 2015;21:119-20. [Crossref] [PubMed]
- Martínez-Téllez E, Trujillo-Reyes JC, Guarino M, et al. Incision. Asvide 2018;5:690. Available online: http://www.asvide.com/article/view/26482
- Martínez-Téllez E, Trujillo-Reyes JC, Guarino M, et al. Introduction of the video-mediastinoscope. Asvide 2018;5:691. Available online: http://www.asvide.com/article/view/26483
- Martínez-Téllez E, Trujillo-Reyes JC, Guarino M, et al. Subxiphoid video-thoracoscopy. Asvide 2018;5:692. Available online: http://www.asvide.com/article/view/26484
- Martínez-Téllez E, Trujillo-Reyes JC, Guarino M, et al. Talc pleurodesis. Asvide 2018;5:693. Available online: http://www.asvide.com/article/view/26485
- Martínez-Téllez E, Trujillo-Reyes JC, Guarino M, et al. Chest tube. Asvide 2018;5:694. Available online: http://www.asvide.com/article/view/26487
- Santos GH, Frater RW. The subxiphoid approach in the treatment of pericardial effusions. Ann Thorac Surg 1977;23:467-70. [Crossref] [PubMed]
- Zielinski M, Rybak M, Solarczyk-Bombik K, et al. Subxiphoid VATS approach for the mediastinum. Video-assist Thorac Surg 2017;2:1. [Crossref]
- Watanabe G, Yamaguchi S, Tomiya S, et al. Awake subxiphoid minimally invasive direct coronary artery bypass grafting yielded minimum invasive cardiac surgery for high risk patients. Interact Cardiovasc Thorac Surg 2008;7:910-2. [Crossref] [PubMed]
- Karagoz HY, Bayazit K, Battaloglu B, et al. Minimally invasive mitral valve surgery: the subxiphoid approach. Ann Thorac Surg 1999;67:1328-32; discussion 1333. [Crossref] [PubMed]
- Borrego Galán JC, Alcázar Montero MC, García García J, et al. Morgagni’s diaphragmatic hernia. Report of 2 cases. Rev Esp Enferm Apar Dig 1989;75:389-92. [PubMed]
- Xu M, Liu C, Guo M, et al. Combined laparoscopic-thoracoscopic esophagectomy and intrathoracic esophagogastric anastomsis. J Thorac Dis 2013;5:895-7. [PubMed]
- Liu CY, Lin CS, Liu CC. Subxiphoid single-incision thoracoscopic surgery for bilateral primary spontaneous pneumothorax. Wideochir Inne Tech Maloinwazyjne 2015;10:125-8. [Crossref] [PubMed]
- Song N, Zhao DP, Jiang L, et al. Subxiphoid uniportal VATS for lobectomy: a report of 105 cases. J Thorac Dis 2016;8:S251-7. [PubMed]
- Lee YC, Baumann MH, Maskell NA, et al. Pleurodesis practice for malignant pleural effusions in five English-speaking countries, survey of pulmonologists. Chest 2003;124:2229-38. [Crossref] [PubMed]
- Moores DW, Allen KB, Faber LP, et al. Subxiphoid pericardial drainage for pericardial tamponade. J Thorac Cardiovasc Surg 1995;109:546-51; discussion 551-2. [Crossref] [PubMed]
- Jutley RS, Khalil MW, Rocco G. Uniportal vs standard three-port VATS technique for spontaneous pneumothorax: comparison of post-operative pain and residual paraesthesia. Eur J Cardiothorac Surg 2005;28:43-6. [Crossref] [PubMed]
- Rogers ML, Duffy JP. Review surgical aspects of chronic post-thoracotomy pain. Eur J Cardiothorac Surg 2000;18:711-6. [Crossref] [PubMed]
- Wang BY, Chang YC, Chang YC, et al. Thoracoscopic surgery via a single-incision subxiphoid approach is associated with less postoperative pain than single-incision transthoracic or three-incision transthoracic approaches for spontaneous pneumothorax. J Thorac Dis 2016;8:272-8. [PubMed]
- Gonzalez-Rivas D, Yang Y, Lei J, et al. Subxiphoid uniportal video-assisted thoracoscopic middle lobectomy and anterior anatomic segmentectomy (S3). J Thorac Dis 2016;8:S540-3. [Crossref] [PubMed]