Uniport versus multiport video-assisted thoracoscopic surgery in the perioperative treatment of patients with T1–3N0M0 non-small cell lung cancer: a systematic review and meta-analysis
Introduction
Over the past two decades, video-assisted thoracoscopic surgery (VATS) has been widely accepted as the preferred method for diagnosing or resecting the early clinical stages of non-small cell lung cancer (NSCLC). VATS was initially applied through multiports in the thoracic wall; however, more than 50% patients treated with VATS report postoperative chest wall paresthesia related to the portal sites (1). Therefore, fewer and smaller ports have been acquired for the surgical procedure.
With the development of surgical techniques and instruments over recent years, more and more surgeons regard uniport VATS as a feasible option since it could be associated with less thoracic invasiveness. Also, other potential advantages have been reported, including a significant reduction of postoperative pain (2,3), a shorter hospital stays (4,5) as well as improved patient satisfaction (6). Therefore, there was a hypothesis that uniport VATS might be superior to multiport VATS. Nevertheless, there were studies reporting that uniport VATS might have potential risks in several clinical outcomes. For example, A study by Han et al. (4) further reported that uniport VATS had a higher rate of major morbidity than multiport VATS. A study by Zhu et al. (7) reported that uniport VATS might be associated with a longer time of operation. In addition to these potential risks, a study by Shen (8) showed that there was no significant difference in terms of blood loss and the duration of hospital stay. Whether uniport VATS is associated with a greater number of potential advantages remains controversial and we found that there was a lack of evaluation of postoperative pain in the previous meta-analysis. Therefore, the purpose of this systematic review and meta-analysis was to compare the perioperative efficacy of uniport VATS and multiport VATS for patients with early-stage NSCLC. Endpoints included operative time, perioperative blood loss, conversion rate, duration of postoperative drainage, length of hospital stay, VAS of postoperative pain, and overall morbidity.
Methods
Data sources
We searched for eligible studies published before 1st October 2017 in PubMed, Embase, Web of Science, and the Wiley Online library. In order to maximize the sensitivity of the search and identify all relevant studies, following groups of key words or MeSH terms were used: (“non-small cell lung cancer” or “non-small cell lung carcinoma” or “non-small cell lung neoplasms” or “lung adenocarcinoma” or “lung squamous cell carcinoma” or “large cell lung cancer”) and (“uniport” or “uniport” or “single port” or “single-incision” or “single incision”) and (“VATS” or “thoracoscope” or “video-assisted” or “video assisted”). Furthermore, the reference lists of the identified papers were scrutinized for other potentially relevant records.
Study inclusion
Studies were eligible for our systematic review and meta-analysis if they were retrospective or prospective studies which featured perioperative data for patients with T1–3N0M0 NSCLC in uniport and multiport VATS cohorts. Clinical staging of NSCLC ranged from I to II. Publications also need to include a date for one of the outcomes (operative time, perioperative blood loss, conversion rate, duration of postoperative drainage, length of hospital stay, visual analogue score of postoperative pain, and overall morbidity). Studies were considered to be ineligible and were excluded if (I) indications were evident that were not in the range of T1–3N0M0 NSCLC; (II) they were case reports, letters, reviews, comments or meta-analyses; (III) they did not contain the relevant data; (IV) if they were based on non-human research; and (V) if they did not feature appropriate controls, overlapped with other studies or duplicated data.
Data extraction and critical appraisal
All relevant data was extracted from the text, figures and tables of identified manuscripts using a standardized form. This was performed independently by two reviewers (M Li and M Zhao). The following information was obtained: author, year, data sources, study period, surgical method, stage, TNM Classification of Malignant Tumors (TNM), age, gender, amount, tumor location, type and size, operative time, perioperative blood loss, conversion rate, duration of postoperative drainage, length of hospital stay, VAS of postoperative pain, and overall morbidity. Disagreements between the two reviewers were resolved by discussion and consensus. The final results were adjudicated and reviewed by a senior investigator (X Yang).
Statistical analysis
Meta-analysis was performed using Review Manager Version 5.3 (Cochrane Collaboration, Software Update, Oxford, UK, http://review-manager.software.informer.com/5.3/). The effective values of dichotomous variables or continuous variables were estimated by odds ratios (OR) or by standardized mean differences (SMD) with 95% confidence intervals (CIs) respectively. Statistical heterogeneity was evaluated using the Chi-square and I2 tests. The significance level for heterogeneity was fixed at P<0.10. Otherwise, heterogeneity was classified as acceptable. An I2 <25% was regarded as low heterogeneity, 25–75% was regarded as medium heterogeneity, and an I2 ≥75% was regarded as high heterogeneity (9,10). A random effects model was used when I2 >50%; otherwise, a fixed effects model was used. For the source of heterogeneity, we carried out sensitivity analysis for each study as a form of secondary analysis. The modified Newcastle-Ottawa scale (NOS) was used to evaluate non-randomized control studies, and the Cochrane Library handbook was used to assess the quality of the controlled trials (9,10). Publication bias was assessed with funnel plots, in which no fewer than 10 studies were included. All P values were two-sided. A significant difference was defined as when P<0.05. The analysis has been reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (11).
Results
Selection process
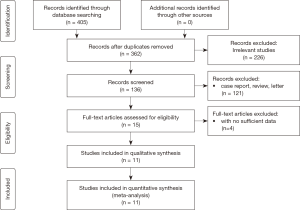
This study followed the guidelines for systematic reviews and meta-analyses. A total of 405 studies, from four electronic databases, were identified by our electronic search strategy. After removing duplicates, irrelevant articles, case reports, letters, reviews, comments or meta-analyses, 15 references were identified and assessed further by screening the full texts. After the exclusion of four studies which did not provide the appropriate data, 11 studies (2-5,7,8,12-16) were included for final assessment and were deemed to be suitable for quantitative meta-analysis. The process of article selection is summarized in Figure 1.
Study characteristics and risk of bias assessment
The included studies were published before 1st October 2017. All 11 studies were retrospective observational studies and included a total of 1,521 patients, of which 629 (41.3%) patients underwent uniport VATS and 892 (58.7%) patients underwent multiport VATS. Among these studies, three articles used a propensity score or a matched pair method (2,8,13). NOS quality scale was the standard for evaluation in all of the eligible studies and scores ranged from 5 to 7. For most included studies, the methodological quality in terms of cohort selection and comparability was adequate. However, the follow-up periods were limited. A detailed summary of the study characteristics is presented in Table 1.
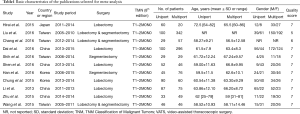
Full table
Publication bias for this meta-analysis was assessed using Review Manager Version 5.3, in which no fewer than 10 studies were included. Publication bias was evaluated for the duration of operation, number of lymph nodes retrieved, length of hospital-stay, and rate of overall morbidity. The results are summarized in Figure 2; symmetrical funnel plots showed that there was less publication bias in our meta-analysis.

Operative outcomes
Duration of operation
Ten studies included comparable data relating to operative time with a combined total of 1,392 patients. High heterogeneity was detected between the uniport and multiport VATS groups (P<0.00001; I2=80%), and a random effects model was used for analysis. A forest plot suggested that compared with multiport VATS groups, uniport VATS was associated with a reduced operative time (uniport: 155.1±40.3 vs. multiport: 176.0±47.0 min); however, there was no significant difference between the uniport and multiport VATS groups (SMD = −0.05; 95% CI: −0.31, 0.22; P=0.72). The results of this analysis are summarized in Figure 3A.
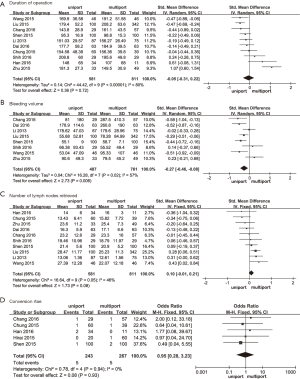
Bleeding volume
A total of eight studies included comparable data relating to bleeding volume, with a combined total of 744 patients. Moderate heterogeneity was observed between the uniport and multiport VATS groups in the random effects model (P=0.02; I2=57%). As shown in Figure 3B, there was a statistically distinct increase in bleeding volume, compared with multiport VATS approach (uniport: 97.7±60.0 vs. multiport: 116.7±99.7 mL, SMD = −0.27; 95% CI: −0.46, −0.08; P=0.006).
Number of lymph nodes retrieved
Comparable data from a combined total of 1,392 patients from 10 studies was for statistical analysis. Moderate heterogeneity was observed between the uniport and multiport VATS groups (P=0.05; I2=46%) and a fixed effects model was therefore used for analysis. The mean number of lymph nodes retrieved for the uniport and multiport VATS groups were 20.2±7.6 and 21.8±9.2, respectively. However, there was no significant difference between the uniport and multiport VATS groups (SMD=0.10; 95% CI: −0.01, 0.21; P=0.08). The results of this analysis are given in Figure 3C.
Conversion rate
Five studies included comparable data related to the rate of conversion to open thoracotomy or need additional ports, with a combined total of 510 patients. No heterogeneity was detected between the uniport and multiport VATS groups (P=0.94; I2=0%) and a fixed effects model was therefore used for analysis. There was no significant difference between the uniport and multiport VATS groups in terms of conversion (uniport: 2.0% vs. multiport: 1.8%), and there was no significant difference between the uniport and multiport VATS groups (OR =0.95; 95% CI: 0.28, 3.23]; P=0.93). The results of this analysis are summarized in Figure 3D.
Postoperative outcomes
Duration of postoperative drainage
Six studies reported comparable data relating to the duration of postoperative drainage, with a combined total of 651 patients. There was low heterogeneity between the uniport and multiport VATS groups (P=0.28; I2 =20%), and we therefore used a fixed effects model. The results of this analysis are summarized in Figure 4A. The forest plot showed that compared with multiport groups, uniport VATS showed a small reduction in the duration of postoperative drainage (uniport: 4.39±2.48 vs. multiport: 4.99±3.24 days). There was a significant difference between the uniport and multiport VATS groups (SMD = −0.27; 95% CI: −0.43, −0.11; P=0.0009).
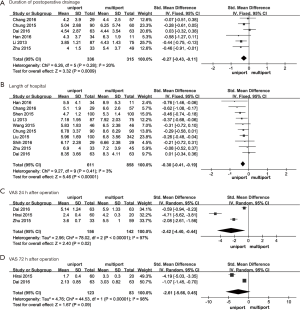
Length of hospital stay
Data relating to hospital stay was obtained from a combined total of 1,469 patients from 10 articles. No significant heterogeneity was detected between the uniport and multiport VATS groups (P=0.41; I2=3%) and we therefore used a fixed effects model for analysis. The results of this analysis are shown in Figure 4B. The mean length of hospital-stay for the uniport and multiport VATS groups were 6.3±2.4 and 7.0±3.6 days, respectively. A significant difference was seen between the uniport and multiport VATS groups (SMD = −0.30; 95% CI: −0.41, −0.19; P<0.00001), indicating that there was a statistically significant reduction with the uniport VATS.
VAS of postoperative pain
We respectively extracted data relating to pain scores 24 h after operation from three articles and after 72 h from two articles. High heterogeneity was detected at both 24 h and 72 h between the uniport and multiport VATS groups (24 h: P<0.00001; I2 =97%; 72 h: P<0.00001; I2 =98%) and we used a random effects model for analysis. Forest plots showed that uniport VATS was significantly associated with lower pain 24 h after operation (uniport: 2.53±0.73 vs. multiport: 4.22±0.71; SMD = −2.42; 95% CI: −4.40, −0.44; P=0.02). Meanwhile, at 72 h after operation, pain scores for uniport VATS were lower than those of patients experiencing multiport VATS, although P=0.09, and was therefore not significant, probably because insufficient data had been extracted (Figure 4C,D).
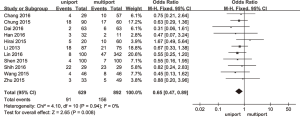
Overall morbidity
Eleven studies included comparable data relating to overall morbidity, with a combined total of 1,521 patients. There was no heterogeneity between the uniport and multiport VATS groups (P=0.94; I2=0%) and a fixed effects model was therefore used for analysis. Uniport VATS was significantly associated with a lower rate of overall morbidity than multiport VATS (OR =0.65; 95% CI: 0.47, 0.89; P=0.008). The forest plot showed that mean overall morbidity for uniport VATS was 14.5%, while that of multiport VATS was 17.5% (Figure 5).
Discussion
There has been an increasing trend for surgeons to use uniport VATS as a minimally-invasive alterative to multiport VATS in the treatment of early stage NSCLC. Our meta-analysis showed that compared with multiport VATS, patients experiencing uniport VATS were associated with a statistically significant reduction in the duration of postoperative drainage, bleeding volume, length of hospital stay, pain score 24 h after operation, and overall rate of complications. However, there were no significant differences between the two treatment groups with regard to operative time, the number of dissected lymph nodes, and the conversion rate. This indicated that compared with multiport VATS, uniport VATS could be performed with relatively similar or improved perioperative outcomes.
Theoretically, a smaller incision is associated with a more difficult surgery. For multiport VATS, the camera and instruments could be placed among the utility thoracotomy and ports for ease of dissection and stapling in case of difficult angle, which is contrary to the case of uniport VATS. In addition, due to single small incision and limited intercostal space, the inevitably intense jamming and interference among thoracoscope and instruments could be expected; hence, this was claimed the major disadvantage of uniport VATS and patients with uniport VATS might have a longer operation time (17). However, our meta-analysis showed that uniport VATS was associated with a reduction in the duration of operation, although this reduction was not statistically significant. A possible reason is that uniport VATS could provide a direct vision, just as that under open thoracotomy. Therefore, eye-to-hand inconsistency would be lower and the speed of the procedure was accelerated. In addition, A shorter operation time was associated with greater experience of surgeons. In Xie’ s study (18), the operation times of the first 100 cases of single-port VAT lobectomy performed by one surgeon were used to evaluate the learning curve. They found that after the first 40 cases, the extent of the reduced time dwindled and the mean operation time reached a plateau, which suggested that the speed of the procedure was accelerated when the number of surgery cases increased and surgeons’ clinical skills improved.
One area of concern is the risk of blood loss with a uniport VATS procedure. Our meta-analysis showed that uniport VATS was associated with a less blood loss. However, only 19mL reduction was shown (uniport: 97.7±60.0 vs. multiport: 116.7±99.7 mL). Therefore, clinical difference might not be obvious although difference was statistically significant (P<0.00001). We also found a less length of hospital-stay and a duration of postoperative drainage in an uniport VATS, which suggested that uniport VATS was benefit for patients’ recovery. However, it was hard to evaluate the accuracy of these parameters because there was no specific criteria and different centers hardly manage the postoperative course with similar protocols.
In our systematic review and meta-analysis, the mortality rate was 0% as reported in both groups. Complication rate for uniport VATS was 14.5%. Complications mainly included air leak, pleural effusion, and wound infection and no serious complications occurred. There was also a low conversion rate for patients experiencing uniport VATS compared to those receiving multiport VATS, suggesting that uniport VATS was not associated with higher operative risks and could meet the requirement of oncology.
Our meta-analysis showed that uniport VATS was associated with a lower pain score. This may be attributed to reduced intercostal nerve injury due to the removal of ports on the mid-axillary and posterior axillary line and reduced compression on the intercostal nerves by scopes. The incision for uniport thoracoscopic lobectomy is usually located on the 4th or 5th intercostal space along the anterior axillary line where a wider intercostal space and fewer muscular layers exist; these features are likely to reduce intercostal nerve injury, at least to some extent. Dai et al. (2) further reported that compared with multiport VATS, uniport VATS had a higher satisfaction score after surgery, which suggested that uniport VATS might get reduced levels of postoperative pain, a lower risk of complication and better postoperative cosmetic results. Although our results showed a reduction in pain scores which were measured by Visual Analogue Score (VAS), it is clear that standardized and objective pain management protocols are required to evaluate benefits of the uniportal approach for pain management.
In 2001, Wilmore and Kehlet proposed “fast track surgery”, which minimized tissue injury and stress response by applying a minimally-invasive technique and improved nursing patterns during the perioperative period in order to accelerate patient recovery (19). Maintaining patient physiology throughout perioperative processes by optimized anesthesiological management and effective pain control represents a crucial aspect of improving efficacy. Our results showed uniport VATS could reduce postoperative pulmonary complications, pain, and hospital stay, which suggested that uniport VATS might have potential benefits in the rapid recovery of patients.
It is important to acknowledge several limitations in our systematic review and meta-analysis. Firstly, the mortality rate was 0% as reported in both groups; however, long-term survival analysis was not possible since most uniport surgery cases were carried out only recently. Secondly, indirect data acquisition methods were used for meta-analysis, such as the extraction of data from the figures of original articles. Thirdly, all the publications selected for meta-analysis are from east Asia (Japan, Taiwan, China, Korea); so, the geographical limitation might heavily bias our results. Another limitation is that there is a variability of technique (lobectomy and segmentectomy) included in the selection criteria, although we found that uniport VATS might have represent a preferable option for the treatment of T1–3N0M0 NSCLC. In addition, it is noteworthy that only studies with pathological nodal negative were included in the meta-analyses, which might mean that the dissection of hilar structure were not so complicated. Therefore, it needs to be further explored whether uniport VATS has potential advantages when patients with pathological nodal positive. Finally, all of the studies involved in our analyses were retrospective; more prospective studies and randomized controlled trials are needed in future.
Conclusions
In conclusion, our meta-analysis provided important evidence that uniport VATS might be more preferable than multiport VATS with regards to bleeding volume, a shorter duration of postoperative drainage and hospital stay, the VAS of postoperative pain and the overall rate of complications. Our results indicated that uniport VATS might have represent a preferable option for the treatment of T1–3N0M0 NSCLC, due to its superior perioperative efficacy.
Acknowledgements
Funding: This study was supported by the National Natural Science Foundation of China (Grant No. 81370587, 81672268) (www.nsfc.gov.cn/), Training Programme for the Talents of Zhongshan Hospital, Fudan University (Grant No 2015ZSYXGG03), Zhengyi Scholar Foundation of School of Basic Medical Sciences, Fudan University (Grant No. S18-04) (http://medicine.fudan.edu.cn/), FDUROP (Fudan’s Undergraduate Research Opportunities Program) (Grant No. 15016), and National University Student Innovation Program (Grant No. 15016) (www.fdurop.fudan.edu.cn/). And we would like to thank International Science Editing Co. for editing the language.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Sihoe A, Au S, Cheung M, et al. Incidence of chest wall paresthesia after video-assisted thoracic surgery for primary spontaneous pneumothorax. Eur J Cardiothorac Surg 2004;25:1054-8. [Crossref] [PubMed]
- Dai F, Meng S, Mei L, et al. Single-port video-assisted thoracic surgery in the treatment of non-small cell lung cancer: a propensity-matched comparative analysis. J Thorac Dis 2016;8:2872-8. [Crossref] [PubMed]
- Hirai K, Takeuchi S, Usuda J. Single-incision thoracoscopic surgery and conventional video-assisted thoracoscopic surgery: a retrospective comparative study of perioperative clinical outcomes. Eur J Cardiothorac Surg 2016;49:i37-41. [PubMed]
- Han KN, Kim HK, Choi YH. Comparison of single port versus multiport thoracoscopic segmentectomy. J Thorac Dis 2016;8:S279-86. [PubMed]
- Chang JM, Kam KH, Yen YT, et al. From biportal to uniportal video-assisted thoracoscopic anatomical lung resection. Medicine 2016;95:e5097. [Crossref]
- Ocakcioglu I, Alpay L, Demir M, et al. Is single port enough in minimally surgery for pneumothorax? Surg Endosc 2016;30:59-64. [Crossref] [PubMed]
- Zhu Y, Liang M, Wu W, et al. Preliminary results of single-port versus triple-port complete thoracoscopic lobectomy for non-small cell lung cancer. Ann Transl Med 2015;3:92. [PubMed]
- Shen Y, Wang H, Feng M, et al. Single- versus multiple-port thoracoscopic lobectomy for lung cancer: a propensity-matched study. Eur J Cardiothorac Surg 2016;49:i48-53. [PubMed]
- Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. [Crossref] [PubMed]
- Li M, Yang X, Chen Y, et al. Stereotactic body radiotherapy or stereotactic ablative radiotherapy versus surgery for patients with T1-3N0M0 non-small cell lung cancer: a systematic review and meta-analysis. Onco Targets Ther 2017;10:2885-92. [Crossref] [PubMed]
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. [Crossref] [PubMed]
- Liu CC, Shih CS, Pennarun N, et al. Transition from a multiport technique to a single-port technique for lung cancer surgery: is lymph node dissection inferior using the single-port technique? Eur J Cardiothorac Surg 2016;49:i64-72. [PubMed]
- Shih CS, Liu CC, Liu ZY, et al. Comparing the postoperative outcomes of video-assisted thoracoscopic surgery (VATS) segmentectomy using a multi-port technique versus a single-port technique for primary lung cancer. J Thorac Dis 2016;8:S287. [PubMed]
- Chung JH, Choi YS, Cho JH, et al. Uniportal video-assisted thoracoscopic lobectomy: an alternative to conventional thoracoscopic lobectomy in lung cancer surgery? Interact Cardiovasc Thorac Surg 2015;20:813-9. [Crossref] [PubMed]
- Wang BY, Liu CY, Hsu PK, et al. Single-incision versus multiple-incision thoracoscopic lobectomy and segmentectomy: a propensity-matched analysis. Ann Surg 2015;261:793-9. [Crossref] [PubMed]
- Li C, Ma H, He J, et al. Clinical analysis of thoracoscopic lobectomy in the treatment of peripheral lung cancer with single utility port. Zhongguo Fei Ai Za Zhi 2013;16:487-91. [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal videoassisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [Crossref] [PubMed]
- Xie D, Wang H, Fei K, et al. Single-port video-assisted thoracic surgery in 1063 cases: A single-institution experience. Eur J Cardiothorac Surg 2016;49:i31-6. [Crossref] [PubMed]
- Wilmore DW, Kehlet H. Management of patients in fast track surgery. BMJ 2001;322:473-6. [Crossref] [PubMed]