Operation for an anomalous systemic arterial supply to the left lower lobe using an anastomosis procedure in an infant
Introduction
An anomalous systemic arterial supply to a normal lung without a normal pulmonary arterial supply and with a normal bronchial connection is a rare congenital anomaly for which no standard treatment has been established (1). Here, we report a case of an infant who underwent end-to-side anastomosis of an abnormal left pulmonary artery to restore normal circulation, rather than ligation or embolization.
Case presentation
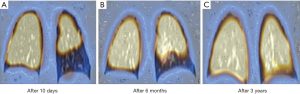
A 7-month-old girl was referred for evaluation of a continuous murmur at the left lower sternal border and on her back. A chest X-ray revealed increased localization of pulmonary vascular markings in the lower left lung. Two-dimensional echocardiography showed a large, abnormal artery arising from the descending aorta at the level of the celiac trunk running to the left lung field. Chest computed tomography (CT) revealed the same abnormal artery and was compatible with a diagnosis of an anomalous systemic arterial supply to the left lower lobe, with the left pulmonary artery supplying only the left upper lung (Figure 1A). To avoid infarction of the left lower lung, we performed an end-to-side anastomosis between the abnormal systemic artery and left pulmonary artery. Postoperative chest CT revealed patency of the anastomosis (Figure 1B). However, a Tc-99m macro-aggregated albumin (MAA) lung perfusion scan performed 10 days after the surgery showed little perfusion of the left lower lung (Figure 2A). Six months postoperatively, there was some improvement in the hypoperfused area on a lung perfusion scan (Figure 2B), and a lung perfusion scan at the 3-year follow-up showed marked improvement and near-complete restoration of the perfusion of the left lower lobe (Figure 2C).

Discussion
Since Pryce et al. (2) classified anomalous systemic arterial supplies in more detail in 1947, several clinical papers have been published. To avoid the risk of massive hemoptysis from pulmonary hypertension, heart failure, or severe infection, these anomalies should be treated in all patients, especially in symptomatic patient. Initially, the main reported treatment was surgical resection of the involved lung after ligation of the anomalous artery; however, the trend shifted towards trans-arterial embolization (3).
Anastomosis of the anomalous systemic arterial supply to the basal segments of the lung has been reported in two papers. In 1970, Hessel et al. (4) reported that anastomosis in a 5-year-old boy resulted in normal blood flow to the left lower lung based on pulmonary angiography, and there was no evidence of pulmonary hypertension. However, they did not perform a lung perfusion scan, which could have proved the improved lung perfusion. In 2003, Iizasa et al. (5) performed anastomosis between the anomalous artery and left pulmonary artery in a 30-year-old man without resecting the basal segments. However, this showed little improvement in perfusion with a lung scan after 6 months. They explained that the unsatisfactory result was due to thickened, sclerotic arterial endothelium caused by prolonged exposure to systemic pressure. To the best of our knowledge, there are no other reports of re-anastomosis.
Our patient is the first reported case of end-to-side anastomosis between the anomalous artery and left pulmonary artery without resection of the lung in an infant. We postulated that an infant would have been exposed to systemic pressure for a relatively short period, enabling reversibility of the sclerotic changes in the pulmonary arterioles. We performed the re-anastomosis, and observed gradual improvement in lung perfusion scans over 3 years postoperatively. We conclude that anastomosis of an anomalous artery to the pulmonary artery is more physiological and feasible than embolization in an infant with pulmonary arterial reversibility.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Albertini A, Dell'Amore A, Tripodi A, et al. Anomalous systemic arterial supply to the left lung base without sequestration. Heart Lung Circ 2008;17:505-7. [Crossref] [PubMed]
- Pryce DM, Sellors TH, Blair LG. Intralobar sequestration of lung associated with an abnormal pulmonary artery. Br J Surg 1947;35:18-29. [Crossref] [PubMed]
- Abe T, Mori K, Shiigai M, et al. Systemic arterial supply to the normal basal segments of the left lower lobe of the lung--treatment by coil embolization--and a literature review. Cardiovasc Intervent Radiol 2011;34 Suppl 2:S117-21. [Crossref] [PubMed]
- Hessel EA 2nd, Boyden EA, Stamm SJ, et al. High systemic origin of the sole artery to the basal segments of the left lung: findings, surgical treatment, and embryologic interpretation. Surgery 1970;67:624-32. [PubMed]
- Iizasa T, Haga Y, Hiroshima K, et al. Systemic arterial supply to the left basal segment without the pulmonary artery: four consecutive cases. Eur J Cardiothorac Surg 2003;23:847-9. [Crossref] [PubMed]


