Septicemic melioidosis: a case report and literature review
Introduction
Melioidosis, caused by the Gram-negative bacterium Burkholderia pseudomallei, is an environmental disease prevalent in southeastern Asia and northern Australia (1). In China, this disease is endemic in several provinces and regions, such as Hainan, Guangdong, Guangxi, Hong Kong, and Taiwan (2). Burkholderia pseudomallei infection is also the most common cause of fatal community-acquired bacteremia pneumonia. We recently treated but unfortunately failed to cure a young patient who had been referred to Central Intensive Care Unit, Guangzhou Red Cross Hospital from Hainan Province due to severe septicemia caused by Burkholderia pseudomallei infection.
Case report
A 22-year-old male patient was admitted on September 11, 2013, to a local hospital of Hainan Province after repeated pyrexia up to 41 °C and dry cough lasting for ten days. Upon admission, physical examination found the second toe of the patient’s right foot had been bitten by an insect or a worm 14 days earlier. He was under regular anti-tuberculosis (TB) treatment because had been confirmed to have TB half a year before. Pneumonia and TB were initially diagnosed and he was given ceftazidime, levofloxacin and azithromycin for anti-infection and anti-TB therapy. However, there was no therapeutic efficacy, for his symptoms of fever and cough continued. The next day after further blood culture detected the existence of Burkholderia pseudomallei in him, he was transferred to Guangzhou Red Cross Hospital on September 17, 2013 for further treatment.
His vital signs upon admission were: temperature, 41.2 °C; pulse, 112 beats/min; respiratory rate, 22 breaths/min; blood pressure, 121/88 mmHg; peripheral oxygen saturation, 97%. He was normally conscious, with coarse breathing sounds from both lungs. An abdominal examination was normal. The right arm between the elbow and metacarpal joint showed skin edema and redness, and slightly higher skin temperature. In particular, a scab over a wound (~0.5 cm × 0.5 cm) was observed on the second toe of the right foot. The patient denied a history of trauma. His previous chest computed tomography scan showed secondary double lung TB with lung cavity formation and a few pulmonary bulla complicated at the upper right lung.
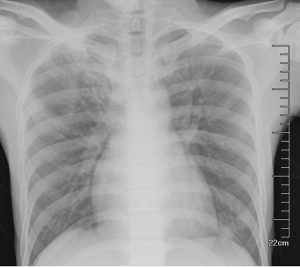
The subsequent laboratory test performed at Guangzhou Red Cross Hospital found: white blood cells, 19.57×109/L; ratio of neutrophils to white blood cells, 91.2%; blood sedimentation, 14 mm/h; high-sensitivity C-reactive protein, 159 mg/L; serum procalcitonin, 132.01 ng/mL; TB antibody, positive; sputum smear examination for mycobacterium TB, negative. A chest radiograph showed exudation, proliferation and cords at double upper lungs and more significant signs at the upper right lung. The preliminary diagnosis was fiber exudative TB at the upper right lung and upper left pulmonary fibrous TB (Figure 1).
The B-mode ultrasound scan image showed no abnormalities at the abdomen or urinary tract. Cardiac color ultrasonography showed mild tricuspid regurgitation and pulmonary artery high pressure (41 mmHg), normal left ventricular systolic and diastolic function and 65% of ejection fraction. After admission, the following diagnoses were made: (I) melioidosis caused by Burkholderia bacteria; (II) pneumonia; (III) secondary pulmonary TB and (IV) right forearm cellulitis. Consequently imipenem was administered for anti-infection, in addition to his ongoing anti-TB therapy.
Unexpectedly, two days post-admission, the patient’s condition did not resolve, with worsening clinical manifestations of tachypnea (respiratory rate rising from 20 times/min on admission to 28 times/min), dropped blood pressure (from 121/88 to 101/78 mmHg), high fever (~41 °C), and poor hemogram (white blood cells decreasing from 19.57×109/L to 4.8×109/L, neutrophilic granulocyte ratio increasing from 91.2% to 92.6% and platelet number decreasing from 290×109/L to 164×109/L). His blood culture was positive for the Gram-negative bacterium Burkholderia pseudomallei, which was subsequently confirmed twice by serial blood culture examinations. The bacterium was sensitive to imipenem, levofloxacin, meropenem, minocycline, trimethoprim-sulfamethoxazole, ceftazidime, amoxicillin/clavulanic acid, and doxycycline.
We judged that the patient had bacteremia, uncontrolled infection and possibly soft tissue cellulitis too. Therefore, the patient was given ciprofloxacin and minocycline for anti-infection. However, the combined antibiotic therapy was once again ineffective. At four days post-admission, the patient had persistent fever, respiratory distress and symptoms related to shock and disseminated intravascular coagulation (DIC). Multiple pus points could be observed on the skin across the shoulder and chest (Figure 2). In addition, his hemogram became worse (white blood cells: 6.36×109/L; neutrophilic granulocyte ratio: 94.5%; platelet number: 88×109/L), and liver and renal dysfunctions developed.
By this time, we had realized that the patient was suffering from septic shock, DIC and multiple organ dysfunction syndromes due to septicemic melioidosis, the causative agent being Burkholderia pseudomallei. However, we had no evidence to rule out the possibility of co-infections by Gram-positive bacteria. Therefore, ciprofloxacin and minocycline were replaced by vancomycin and imipenem was added in the anti-infection algorithm. Simultaneously the patient was supported by ventilator-assisted breathing, anti-shock and DIC therapy and infusion of gamma globulin. Despite all these interventions, the patient’s condition deteriorated progressively. He gradually became delirious, presenting symptoms of multiple organ failure involving the heart, lung, kidney, liver, digestive system, and hematological system. The patient died in hospital on the sixth day post-admission.
The young male patient with a history of pulmonary TB was eventually diagnosed as suffering from septicemia caused by Burkholderia pseudomallei in our hospital. His septicemic melioidosis, acute and severe at onset, advanced very rapidly, the best timing for intervention was missed because no correct diagnosis was made and no effective antibiotics were administered at the early stage. Consequently, although the powerful and sensitive antibiotics administrated in our hospital but failed to control his condition either. His death was caused by septic shock induced by septicemic melioidosis.
Discussion
Burkholderia pseudomallei, the causative agent of melioidosis, is a Gram-negative aerobic bacterium or saprophyte that spreads widely in tropical and subtropical soils and waters, with a high degree of virulence and strong antibiotic resistance. Humans or other animals may become infected after contacting contaminated water or bitten by blood-sucking insects. Human infectious melioidosis is classified as acute, subacute, chronic, and subclinical septicemia. Acute sepsis is the most serious, accounting for up to 60% of all the infections of its kind. Its mortality rate can reach as high as 90% in absence of effective intervention, and 50% even after antibiotic therapy (3).
In China, the reported mortality of human melioidosis is from 24% to 44.1% (4-6). Current interventions are early intravenous administration of antibiotics, ceftazidime or carbapenems, for 10 to 14 days, followed by oral administration of co-trimoxazole or co-trimoxazole doxycycline for 12 to 20 weeks (7,8). Although ceftazidime was reported to be the most effective antibiotic for melioidosis (9), its therapeutic response is disappointingly slow in most cases, probably because its efficacy is multifactorial and dependent on the properties of the organism and the clinical symptoms and immune status of the host (10). Carbapenem, the minimum inhibitory concentration of which was found to be relatively low in an in vitro experiment (11), is currently considered a preferred antibiotic for this disease. Therefore, administration of carbapenem combined with one or more other antibiotics is expected to lead to a better therapeutic outcome.
There are two possible factors that might have accounted for the development of septic shock in this case. First, the causative Burkholderia pseudomallei might have been insensitive to ceftazidime, because it could have formed a surface biofilm to resist the antibiotic as reported. Secondly, his initial treatment failed to provide him with necessary support therapies. Since melioidosis is prone to hypovolemia at the acute stage (12), adequate fluid resuscitation might have been critical at that time.
It is not easy to distinguish melioidosis from pulmonary TB and arrive at a definite diagnosis of melioidosis at its early stage because the two conditions have many clinical manifestations in common. Now that the patient had been diagnosed with TB six months previously, we reasonably suspected he might have been complicated with lung melioidosis. Based on overall data, we also suspected that the septicemia caused by acute septicemic melioidosis in this victim might have been triggered by the invasion of Burkholderia pseudomallei into his blood via the wound on the second toe of his right foot.
In conclusion, since no specific vaccines are available against Burkholderia pseudomallei, the medical community should be highly alert to the possibility of melioidosis in areas where the bacterium is endemic. Careful investigations into the patient’s history of exposure to polluted water or soil and early bacterial examination of clinical samples are crucial in a correct and timely diagnosis. At the same time, timely administration of effective antibiotics and adequate fluid resuscitation to counteract hypovolemia at the early stage of therapy also helps save life.
Acknowledgements
Funding: Supported by Guangdong Medical Scientific Research Funds (B2012304).
Disclosure: The authors declare no conflict of interest.
References
- Pibalpakdee P, Wongratanacheewin S, Taweechaisupapong S, et al. Diffusion and activity of antibiotics against Burkholderia pseudomallei biofilms. Int J Antimicrob Agents 2012;39:356-9. [PubMed]
- Xuhu M. Progress on melioidosis. Journal of Third Military Medical University 2011;33:1315-7.
- Chen D. eds. Antimicrobial agents and bacterial resistance. Shanghai: East China University of Science and Technology Press, 2001:1.
- Li TJ, Fu HQ, Huang T, et al. Melioidosis Burkholderia infection in the clinical characteristics and drug resistance analysis. Chinese Journal of Laboratory Diagnosis 2011;15:888-90.
- Quan HB, Gao YY, Chen DX, et al. Observation on the clinical features of diabetes mellitus cases complicated with Burkholderia pseudomallei septicemia. China Tropical Medicine 2006;6:1750-2.
- Wu DR, Guo HL, Chen H. Hainan area melioidosis burkholderia bacteria infection characteristics and drug resistance. Shandong Medical Journal 2009;49:79-80.
- Cheng AC, Currie BJ. Melioidosis: epidemiology, pathophysiology, and management. Clin Microbiol Rev 2005;18:383-416. [PubMed]
- Wuthiekanun V, Peacock SJ. Management of melioidosis. Expert Rev Anti Infect Ther 2006;4:445-55. [PubMed]
- White NJ, Dance DA, Chaowagul W, et al. Halving of mortality of severe melioidosis by ceftazidime. Lancet 1989;2:697-701. [PubMed]
- Puthucheary SD, Sam IC. Why is the response rate slow in ceftazidime therapy for melioidosis? Expert Rev Anti Infect Ther 2012;10:5-7. [PubMed]
- Smith MD, Wuthiekanun V, Walsh AL, et al. In-vitro activity of carbapenem antibiotics against beta-lactam susceptible and resistant strains of Burkholderia pseudomallei. J Antimicrob Chemother 1996;37:611-5. [PubMed]
- White NJ. Melioidosis. Lancet 2003;361:1715-22. [PubMed]



