Treatment of spontaneous esophageal rupture (Boerhaave syndrome) using thoracoscopic surgery and sivelestat sodium hydrate
Introduction
Esophageal rupture, including spontaneous esophageal rupture [Boerhaave syndrome, first reported in 1724 (1,2)], is a life-threatening disease. Early diagnosis and treatment is needed for good outcome of the disease (3-5). However, the initial diagnostic accuracy rate for spontaneous esophageal rupture is reported to be approximately 30%. Moreover, the mortality rate is 20% to 40% due to severe respiratory failure (5-7). Surgical treatment is performed mainly for the disease, including primary suture with or without reinforcement, such as an omental patch; pleural, pericardial, or diaphragmatic pedicle flap; or fundic patch, and successive lavage and drainage of the thoracic cavity (4,6,8,9). Conservative treatment is selected in limited patients (10-12). There are few reports of thoracoscopic surgery for the disease (13-16). We have performed thoracoscopic surgery for esophageal disease, mainly for esophageal cancer, at our department since 1994 (17). We also have applied this procedure to benign diseases, including spontaneous esophageal rupture.
Sivelestat sodium hydrate is a selective neutrophil elastase inhibitor and known to suppress the inflammation of the lung due to acute lung injury (ALI) following systematic inflammatory response syndrome (SIRS). It also reportedly increases pulmonary function, reduces the duration of mechanical ventilation, and shortens the intensive care unit (ICU) stay in the patients with ALI following the SIRS (18-21). In addition, perioperative administration improves pulmonary function and/or clinical course in patients after thoracic surgery (22-25). SIRS and ALI are significant complications of spontaneous esophageal rupture and typically cause death.
In this study, we retrospectively investigated the usefulness of thoracoscopic surgery and perioperative administration of sivelestat sodium hydrate for spontaneous esophageal rupture.
Methods
Patients
We collected clinical data from our database and medical records of all 12 patients who underwent thoracoscopic surgery for spontaneous esophageal rupture between 2002 and 2014. This study was approved by the ethical committee of Tohoku University (accession number 2017-4-18).
Surgical procedure
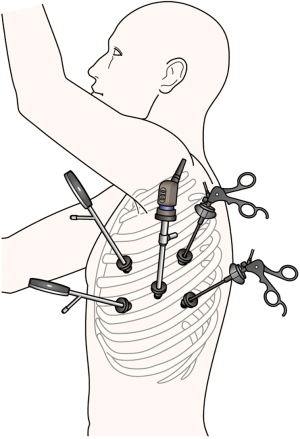
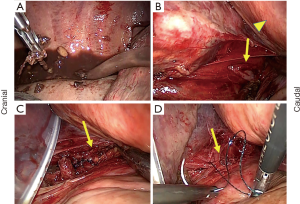
General anesthesia was performed via one-lung ventilation using a double lumen tube. All patients were placed in the right decubitus position for thoracic surgery. Regarding thoracic drainage and/or thoracoscopic suture, we typically performed the procedure with five thoracic ports inserted into the left thoracic cavity. An 11.5-mm thoracic port inserted at the sixth intercostal space in the midaxillary line was used for thoracoscopy. Two thoracic ports were inserted on the dorsal side for the operator at the fifth and seventh intercostal spaces in the posterior axillary line, and two thoracic ports were inserted on the ventral side for the first assistant at the fourth and sixth intercostal spaces in the anterior axillary line. We added another port and/or shifted the position of these ports by one or two intercostal spaces as needed (Figure 1). After irrigation of thoracic cavity, the wound of esophagus was closed using absorbable suture in two layers of the mucous membrane and the muscularis propria with adventitia if possible (Figure 2) and indwelling drainage tubes were placed. In patients requiring transhiatal sutures, we closed the wound similar to the thoracic procedure and reinforced it with an omental patch as needed.
Statistical analysis
All statistical analyses were performed using JMP Pro Version 13 (SAS Institute Japan, Tokyo, Japan). Continuous data were assessed using Student’s t-test or the Mann-Whitney U test and categorical data were analyzed using Pearson’s χ2 test, Fisher’s exact test, or the Mann-Whitney U test as appropriate. A P value of <0.05 was considered statistically significant.
Results
Patient characteristics and surgical outcome
Patient characteristics and surgical outcome are summarized in Table 1. The patient cohort included 11 males and one female (median age, 61 years; range, 43–74 years). The lower left esophageal wall was perforated in all patients. Surgical procedures consisted of thoracoscopic suture and thoracic drainage in six patients, transhiatal suture and thoracoscopic thoracic drainage in five (four with omental patch reinforcement), and thoracoscopic esophagectomy (two-stage reconstruction) and thoracic drainage in one. Median time from onset to surgery was 8 hours (range, 5–48 hours) with a surgical duration of 210 minutes (range, 112–323 minutes), blood loss 260 mL (range, 5–1,320 mL), postoperative ventilator management 1 day (range, 0–26 days), ICU stay 5 days (range, 1–39 days), and interval to restoration of oral ingestion 13 days (range, 5–163 days). Postoperative complications included respiratory failure due to pneumonia or acute respiratory distress syndrome (ARDS) in four patients (33%), pyothorax in three (25%), and leakage in one (8.3%), including duplicated cases. Although long-term respiratory management was required in some patients, there was no instance of perioperative mortality.
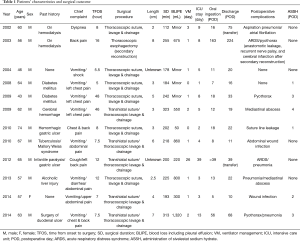
Full table
Administration of sivelestat sodium hydrate and patient outcomes
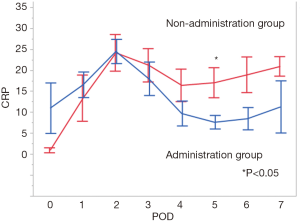
When evaluated according to the perioperative administration of sivelestat sodium hydrate (six administration cases vs. six non-administration cases). There were no significant differences between the groups in sex, age, time from onset to surgery, surgical procedure, surgical duration, and blood loss as background. There was also no significant difference in median time of ventilator management, ICU stay, oral ingestion following surgery, or hospital stay (1 vs. 1, 4 vs. 6.5, 15 vs. 14.5, and 20.5 vs. 30.5 days, respectively). On the other hand, the postoperative arterial oxygen partial pressure-to-fractional inspired oxygen (P/F) ratio decreased over time in the non-administration group, whereas there was no change in the administration group. There was a significant difference in the P/F ratio between the groups on postoperative day 4 (P=0.035; Figure 3). In addition, postoperative C-reactive protein (CRP) levels decreased after an initial increase in both groups, but the decrease was greater in the administration group and differed significantly between the groups on postoperative day 5 (P=0.037; Figure 4). A total of 4.8 mg/kg/day sivelestat sodium hydrate was administrated in each patient intravenously.

Discussion
Recently, thoracoscopic surgery has become widespread and some studies have reported that thoracoscopic surgery for esophageal cancer was less invasive than open surgery, especially regarding pulmonary function after surgery. There was no perioperative death in our study, but one patient (in 2003) died of pneumonia following cerebral infarction within 7.6 months postoperatively. However, the long-term survival rate was 91.7% (11/12), which was higher than that reported previously. It may be considered that, in addition to recent improvement in anesthesia and multidisciplinary treatment, less invasive thoracoscopic surgery contributed to the treatment outcome. The suture line leak rate was 8.3% (1/12), which was considered acceptable. Patients with a greater interval between onset and surgery tended to experience complications, such as pyothorax, and longer intervals to treatment. This reveals that early diagnosis and early treatment are essential, similar to findings of previous reports. For early diagnosis, we believe that recall of the disease name is important. The chief complaint of vomiting and results of diagnostic imaging may help with recall. If you suspect the disease, do the upper gastrointestinal series to confirm it.
The surgical procedure to be performed is determined by the size of the rupture site, time from onset, brittleness of the tissue due to infection and necrosis, and degree of mediastinitis and intrathoracic contamination. Presently, we believe that thoracoscopic suture will provide adequate results except in the case of intraperitoneal contamination. Direct suture via thoracoscopy is less invasive and thoracoscopy is useful for irrigating the entire thoracic cavity. However, the procedure is relatively advanced and requires practice. In many patients, the laceration width of the mucous membrane was wider than that of the muscularis propria, so we considered that an important point is to watch both edges of the mucous membrane laceration carefully and suture it securely. On the other hand, a transhiatal suture may be considered to increase the security, since it is performed under direct vision, and several reinforcements are made, such as with an omental patch (6,26). At the moment, the appropriate procedure should be selected according to the condition of the patient and experience and condition of the facility. We intend to keep the quality of surgery constant for following years. However, dexterity improvement and experience gain may influence the quality. Selection of the surgical procedure in this long-term research can also influence the quality. These issues are a limitation of this study, which is very difficult to resolve. In any case, with the spread of thoracoscopy, the use of thoracoscopic surgery for esophageal rupture will increase in the future. Currently, we are trying to introduce into this surgery use of the semiprone position to achieve good access to the posterior mediastinum and of barbed suture material for simpler and quicker suturing (16).
The P/F ratio and CRP levels in the sivelestat sodium hydrate administration group progressed favorably compared to those of the non-administration group. Figures 3,4 suggest that sivelestat sodium hydrate may help improve systematic inflammation rates and maintain the patient’s respiratory condition postoperatively. Since this is a retrospective study, there may be bias that sivelestat sodium hydrate was used in patients with relatively bad respiratory conditions. However, this is thought rather to affirm the results above. There would be more difference if sivelestat sodium hydrate had been administered to more patients with good conditions. Instead, our results revealed that, if there was bias, the respiratory condition could be improved even in patients with worse respiratory conditions. In addition, the clinical efficacy of sivelestat for ALI remains controversial. Pu et al. reported that sivelestat administration for ALI/ARDS might increase the P/F ratio, although it had little or no effect on 28–30 days mortality, ventilation days, and ICU stays similar to this study (27). We believe that the improvement of the postoperative respiration and inflammatory response will help the medical doctors and staffs during the treatment of the disease. In addition, study regarding the optimal dose and administration period of sivelestat sodium hydrate is needed. Of course, a randomized controlled trial is necessary to achieve a high level of evidence, although it is very difficult due to the rarity of patients.
Conclusions
Although thoracoscopic surgery requires separate lung ventilation and surgical tolerance varies among individual patients, acceptable results were obtained for all patients, including two with a significant time elapse from onset to treatment. Furthermore, sivelestat sodium hydrate was suggested to help improve postoperative respiration and inflammatory response.
Acknowledgements
The authors thank Mr. Yoshihiko Tsuda, a designer of Davinci Medical Illustration Office (medical-illust.com/index.html) for making Figure 1 and Enago (www.enago.jp) for the English language review.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the ethical committee of Tohoku University (accession number 2017-4-18) and written informed consent was obtained from all patients.
References
- Derbes VJ, Mitchell RE Jr. Hermann Boerhaave’s Atrocis, nec descripti prius, morbi historia, the first translation of the classic case report of rupture of the esophagus, with annotations. Bull Med Libr Assoc 1955;43:217-40. [PubMed]
- Schweigert M, Dubecz A, Solymosi N, et al. Times and trends in the treatment of spontaneous perforation of the esophagus: from Herman Boerhaave to the present age. Am Surg 2013;79:902-8. [PubMed]
- Lawrence DR, Ohri SK, Moxon RE, et al. Primary esophageal repair for Boerhaave’s syndrome. Ann Thorac Surg 1999;67:818-20. [Crossref] [PubMed]
- Lázár G Jr, Paszt A, Simonka Z, et al. A successful strategy for surgical treatment of Boerhaave's syndrome. Surg Endosc 2011;25:3613-9. [Crossref] [PubMed]
- Pate JW, Walker WA, Cole FH, et al. Spontaneous rupture of the esophagus: a 30-year experience. Ann Thorac Surg 1989;47:689-92. [Crossref] [PubMed]
- Brinster CJ, Singhal S, Lee L, et al. Evolving options in the management of esophageal perforation. Ann Thorac Surg 2004;77:1475-83. [Crossref] [PubMed]
- Pezzetta E, Kokudo T, Uldry E, et al. The surgical management of spontaneous esophageal perforation (Boerhaave’s syndrome) 20 years of experience. Biosci Trends 2016;10:120-4. [Crossref] [PubMed]
- Goldstein LA, Thompson WR. Esophageal perforations: a 15-year experience. Am J Surg 1982;143:495-503. [Crossref] [PubMed]
- Grillo HC, Wilkins EW Jr. Esophageal repair following late diagnosis of intrathoracic perforation. Ann Thorac Surg 1975;20:387-99. [Crossref] [PubMed]
- Cameron JL, Kieffer RF, Hendrix TR, et al. Selective nonoperative management of contained intrathoracic esophageal disruptions. Ann Thorac Surg 1979;27:404-8. [Crossref] [PubMed]
- Ivey TD, Simonowitz DA, Dillard DH, et al. Boerhaave syndrome. Successful conservative management in three patients with late presentation. Am J Surg 1981;141:531-3. [Crossref] [PubMed]
- Mizutani K, Makuuchi H, Tajima T, et al. The diagnosis and treatment of esophageal perforations resulting from nonmalignant causes. Surg Today 1997;27:793-800. [Crossref] [PubMed]
- Cho JS, Kim YD, Kim JW, et al. Thoracoscopic primary esophageal repair in patients with Boerhaave’s syndrome. Ann Thorac Surg 2011;91:1552-5. [Crossref] [PubMed]
- Ikeda Y, Niimi M, Sasaki Y, et al. Thoracoscopic repair of a spontaneous perforation of the esophagus with the endoscopic suturing device. J Thorac Cardiovasc Surg 2001;121:178-9. [Crossref] [PubMed]
- Landen S, El Nakadi I. Minimally invasive approach to Boerhaave’s syndrome: a pilot study of three cases. Surg Endosc 2002;16:1354-7. [Crossref] [PubMed]
- Nakano T, Sato C, Sakurai T, et al. Thoracoscopic esophageal repair with barbed suture material in a case of Boerhaave’s syndrome. J Thorac Dis 2016;8:E1576-80. [Crossref] [PubMed]
- Akaishi T, Kaneda I, Higuchi N, et al. Thoracoscopic en bloc total esophagectomy with radical mediastinal lymphadenectomy. J Thorac Cardiovasc Surg 1996;112:1533-40; discussion 1540-1. [Crossref] [PubMed]
- Kawabata K, Hagio T, Matsuoka S. The role of neutrophil elastase in acute lung injury. Eur J Pharmacol 2002;451:1-10. [Crossref] [PubMed]
- Kawabata K, Suzuki M, Sugitani M, et al. ONO-5046, a novel inhibitor of human neutrophil elastase. Biochem Biophys Res Commun 1991;177:814-20. [Crossref] [PubMed]
- Tamakuma S, Ogawa M, Aikawa N, et al. Relationship between neutrophil elastase and acute lung injury in humans. Pulm Pharmacol Ther 2004;17:271-9. [Crossref] [PubMed]
- Zeiher BG, Matsuoka S, Kawabata K, et al. Neutrophil elastase and acute lung injury: prospects for sivelestat and other neutrophil elastase inhibitors as therapeutics. Crit Care Med 2002;30:S281-7. [Crossref] [PubMed]
- Kawahara Y, Ninomiya I, Fujimura T, et al. Prospective randomized controlled study on the effects of perioperative administration of a neutrophil elastase inhibitor to patients undergoing video-assisted thoracoscopic surgery for thoracic esophageal cancer. Dis Esophagus 2010;23:329-39. [Crossref] [PubMed]
- Kobayashi M, Irinoda T, Akiyama Y, et al. Effect of a selective neutrophil elastase inhibitor on early recovery from body water imbalance after transthoracic esophagectomy. Dis Esophagus 2010;23:565-71. [Crossref] [PubMed]
- Nagai Y, Watanabe M, Baba Y, et al. Preventive effect of sivelestat on postoperative respiratory disorders after thoracic esophagectomy. Surg Today 2013;43:361-6. [Crossref] [PubMed]
- Suda K, Kitagawa Y, Ozawa S, et al. Neutrophil elastase inhibitor improves postoperative clinical courses after thoracic esophagectomy. Dis Esophagus 2007;20:478-86. [Crossref] [PubMed]
- Sulpice L, Dileon S, Rayar M, et al. Conservative surgical management of Boerhaave’s syndrome: experience of two tertiary referral centers. Int J Surg 2013;11:64-7. [Crossref] [PubMed]
- Pu S, Wang D, Liu D, et al. Effect of sivelestat sodium in patients with acute lung injury or acute respiratory distress syndrome: a meta-analysis of randomized controlled trials. BMC Pulm Med 2017;17:148. [Crossref] [PubMed]


