The influence of heparin on coagulation function of patients undergoing video-assisted major thoracic surgery
Introduction
Lung cancer and esophagus cancer are the two most common cancers, surgical resection is viewed as the standard therapy (1). Venous thromboembolism (VTE), including deep vein thrombosis and pulmonary embolism, is a severe complication which increases hospital stay, hospital costs, mortality, with an incidence of 1.3% to 24% (1-3). The development of VTE is associated with surgery, malignant cancers, age, immobilization, obesity, history of VTE, infection, radiotherapy (1,4). So there is no doubt that the patients diagnosed with malignant neoplasm have a higher risk suffering VTE, especially those with surgical resection (5). Cancer patients were reported to have around 5- to 7-fold higher risk of VTE compared with normal population (6). Besides, patients suffered from cancer were also found to have more than threefold of risk of fatal PE than non-cancer patients receiving esophagectomy, lobectomy or other similar thoracic surgery (7). Therefore, with such risk factors of elderly, cancer, surgery and immobilization, the patients were in urgent need of sufficient prophylaxis while avoiding hemorrhage. At present, thoracic surgeons usually use heparin or low-molecular-weight-heparin postoperatively for patients. However, there is still a relative high incidence of VTE, it is reported that the incidence of DVT, PE, and VTE within 1 month after esophagectomy for esophageal cancer is 6.1%, 2.4%, and 7.3%, respectively (1). Therefore, there is an urgent need to explore the proper time and dosage of the usage of heparin. As American College of Chest Physicians Evidence-Based Clinical Practice Guidelines advised to administrate heparin for the orthopedic surgery patients 12 or more hours preoperatively (8), we assumed that thoracic surgery was as safe and reasonable as orthopedic surgery. Meanwhile, there is the condition for us to execute the administration of heparin preoperatively owing to the special medical circumstance in China, in which the patients would be admitted to hospital for 3–5 days before surgery intending to complete the related preoperative examination and do the psychological preparation. The patients accepted heparin after admission to hospital. Then we investigate the influence of heparin to coagulation function with administrating heparin preoperatively as thromboprophylaxis for Chinese patients intended for thoracoscopic major thoracic surgery.
Methods
Patients
This was a prospective study and approved by the Ethics Committee of West China Hospital, Sichuan University (approval number: 20160601). All the enrolled patients were provided written informed consent in our study and intended to undergo thoracoscopic major thoracic surgery (including lobectomy, esophagectomy) under general anesthesia in our hospital from June 2016 to May 2017. All those patients were routinely screened for VTEs by ultrasound before hospital admission and received routine blood test, coagulation function test, liver and renal function test. The inclusion criterion: (I) 18–75 years old without any preoperative VTEs in 2 weeks; (II) patients intended for video-assisted thoracoscopic major thoracic surgery (including lobectomy, esophagectomy). The exclusion criterion included: (I) patients with coagulation disorders: preoperative international normalized ratio (INR) >1.5, or blood platelet count <50×109/L; (II) patients receiving any therapeutic anticoagulation preoperatively; (III) patients undergoing planned open thoracic surgery; (IV) patients with severe renal or liver dysfunction.
Trial design and interventions
In the period of June 2016 to May 2017, our study was conducted in one single center, the Department of Thoracic Surgery, West China Hospital, Sichuan University. In total, 91 patients were picked up randomly after admission into our department and all accepted the surgery executed by one surgical team (directed by Dr. Lin). The patients would receive blood test before any therapy after admission to our department immediately. Besides, the postoperative blood test timing was the same time of first day after surgery in the morning. All the patients started heparin sodium (5,000 U, bid) immediately after admission and continued until discharge. After surgery, if the chest drainage volume exceeded 500 mL per day, heparin was ceased temporarily until the drainage volume was less than 500 mL every day, then restarted heparin until discharge. Chest drainage tube could be removed with the following conditions: (I) for lobectomy, the tube would be removed if the chest tube drainage volume was less than 250 mL/day, without air leak; (II) for esophagectomy, the chest tube would be removed if the drainage volume was less than 250 mL/day after oral intake begins (usually on postoperative day 6). All those patients were again routinely screened for VTEs rightly after remove of chest tube.
Data for analysis
There was not baseline data comparison in our study, since it was only one group that the baseline data such as weight, age, sex ratio need not to be compared. The end points were coagulation function data [blood platelet count, prothrombin time (PT), activated partial thromboplastin time (APTT), thrombin time (TT), fibrinogen (FIB) and INR] (collected by other colleagues in our department who were outside of the trial). Moreover, we counted the average hospital stay, chest drainage tube maintaining time and drainage volume.
Statistical analysis
Statistical analysis was conducted with SPSS 22.0 software (SPSS Corp., Chicago, IL, USA). Data presented by mean value ± standard deviation for continuous variables or number (%) for categorical data. For continuous variables, Student’s t-test was applied; as for categorical data, the chi-square or Fisher’s exact test was used. A P value of <0.05 (2-sided) was considered to be statistically significant.
Results
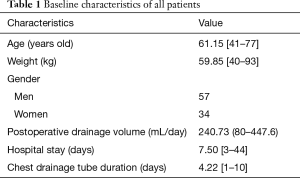
A total of 111 patients were enrolled, according to the inclusion and exclusion criterion preoperatively, besides some refused to join the trial or gave up surgery owing to the stage condition of neoplasm. Finally, 91 patients took part in the trial in all, and all received video-assisted major thoracic surgery from June 2016 to May 2017. All the patients entirely underwent video-assisted major thoracic surgery without any uncontrollable situation which could result in shifting surgery method to open thoracic surgery. The baseline characteristics of the patients were shown (Table 1). In total, 19 patients underwent esophagectomy, while 72 patients received lobectomy in our study. Mean drainage volume of all the patients were 240.73 mL for each patient every day, the patients were in hospital for 7.50 days in average, with chest drainage tube 4.22 days each patient.
Full table
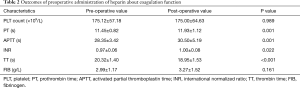
The preoperative and postoperative parameters of the patients were listed in Table 2. The mean values of preoperative and postoperative blood platelet count (175.12 and 175.00 respectively), PT (11.45 and 11.93 respectively), APTT (28.35 and 30.50 respectively), TT (20.32 and 18.95 respectively), INR (0.97 and 1.00 respectively), FIB (2.99 and 3.27 respectively) were all in clinically normal range. Administrated with heparin sodium preoperatively, blood platelet count was similar between pre-operation and post-operation (P=0.989). Besides, there were no significant difference concerning FIB (P=0.161) either. However, significant difference were observed in PT (P=0.001), APTT (P=0.001), INR (P=0.022) between the two time points, respectively. The three postoperative parameters of coagulation function all increased compared to pre-operation. What was a little interesting about TT was that it showed significant difference between the two time points (P<0.001) with decreasing after operation, however, both values of before and after operation were in clinical normal range, so there was not any significance for the change in clinical. In summary, the result may be consequence of the small sample.
Full table
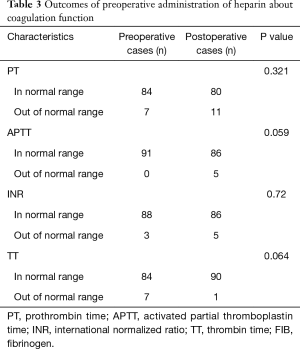
Since one of our exclusion was preoperative INR >1.5, or blood platelet count <50×109/L, the normal clinical range of INR and PLT count were 0.88–1.15, 100×109–300×109/L, in our hospital respectively. Some coagulation parameters of the patients were not normal preoperatively, though not too far from the normal range, they were more likely to develop worse. And the mean values of postoperative coagulation parameters were so near to preoperative parameters. Then we used Chi-square or Fisher’s exact test to assess the ratio (number of abnormal cases/all cases) between preoperative and postoperative cases in Table 3. PT showed no significant difference (7/91 and 11/91, respectively; P=0.321) between the two points. And there was not significantly different for INR (3/91 and 5/91, respectively; P=0.72). Still, postoperative APTT was similar to preoperative APTT (0/91 and 5/91, respectively; P=0.059). Moreover, no significant difference was also observed in postoperative TT (7/91 and 1/91, respectively; P=0.064).
Full table
Neither death, VTE including DVT and PE nor major bleeding events occurred in our trial. Moreover, almost patients had no major postoperative complications such as severe pulmonary infection and bronchopleural fistula, except one patient who underwent esophagectomy suffered anastomosis leakage and secondary pulmonary infection. Treated with conservative therapies including mixed nutrition of enteral and parenteral alimentation, thoracic cavity drainage, anti-infection, electrolyte balance and other symptomatic treatments, the patient recovered well and discharged with stable vital signs and ability to have half-fluid food. Another one experienced right pneumothorax when the chest drainage tube was removed, then chest drainage tube was administrated again until the symptoms disappeared and the DR image of chest showed well.
Discussion
To our knowledge, there have been many studies exploring thromboprophylaxis after major thoracic surgery with heparin or other agents. However, preoperative administration of thromboprophylaxis agents was relatively lacking in video-assisted major thoracic surgery, owing to consideration of the risk of bleeding. In this study, comparison between preoperative and postoperative coagulation function for the same group patients was conducted solely, which was viewed as an innovative method, it deeply investigated the influence of preoperative administration of heparin on coagulation function when there was only one group doing self-longitudinal comparison. In our study, we found that the usage of preoperative heparin 5,000 U BID after admission to hospital made the postoperative coagulation parameters significantly different from preoperative factors. However, the mean values of all parameters still located in normal range, both before and after operation. Therefore, the preoperative administration of heparin demonstrated no influence on coagulation function clinically. In our previous study, study group (preoperative heparin 5,000 U BID) showed no significant difference compared to control group (postoperative heparin 5,000 U BID), which similarly supported the outcome that preoperative heparin was not only feasible but safe (5). Previous study reported that the frequency of DVT ranges from 19–26% after thoracic surgery (9). However, no VTE or major bleeding event occurred in our patients with the preoperative use of heparin, demonstrating the efficacy and safety of our method.
In our study, a total of 91 patients consist of 34 women and 57 men, with a mean age of 61.15 years old and a mean weight of 59.85 kilograms, it demonstrated the characteristics of the patients, which seemed high age, male were prone to suffer the disease. All the patients received video-assisted major thoracic surgery without anyone surgery method shift to open thoracic surgery. All the patients had a mean drainage volume of 240.73 mL per day and in-hospital duration for 7.5 days in average. What else chest drainage tube duration was 4.22 days in average. In actual, the data was acceptable and reasonable for major thoracic surgery which was even superior to average level. It was interesting that postoperative outcome of TT, it decreased significantly compared to preoperative value, while both mean values were located in clinically normal range. However, the decrease of TT value was not meaningful in clinical practice. Besides, one patient who stayed hospital for 45 days suffered anastomosis leakage and secondary pulmonary infection. Another one experienced pneumothorax when the chest drainage tube was removed resulting in 29 days of hospital stay. But both of them recovered completely when discharged. What we concerned more was that neither major bleeding event occurred to all patients nor thromboembolism happened.
Cancer, age, surgery, immobilization, thromboembolism history, duration of surgery were several factors that made patients in increased high risk of suffering from acute PE and DVT (2,10). Specifically in terms of chest surgery, Ziomek et al. conducted a trial in which 77 patients underwent lung resection for lung cancer, reporting 20 patients (26%) suffered a thromboembolic episode in the postoperative period, 15 cases of DVT and 5 cases of PE (9). In spite of wide use of prophylaxis of VTE, Gómez-Hernández et al. found the risk of VTE for patients receiving lung resection, especially Pneumonectomies was still not inconsiderable, and as soon as the patients presented acute respiratory episode, this complication should immediately be taken into account as a priority suspected diagnosis (11). Besides, the risk of VTE varies among different cancers, which is especially high for malignant esophagus neoplasm resection. The patients with esophagus cancer were often exposed to related risk factors, resulting in high risk of VTE that could descend up to 13.2% (12-14). Hence, the current administration of heparin intending to solve the issue of VTE prophylaxis for the malignant neoplasm patients who were ready to undergo surgery was not sufficient, especially for thoracic surgery. What’s more, there was still no consensus on the specific time and dosage of heparin for VTE prophylaxis before and after thoracic cancer surgery. Therefore, more studies were in urgent need.
According to the conditions of VTE related to malignant thoracic neoplasm surgery, our study administrated heparin sodium to patients after admission to our department until discharge for providing adequate VTE prophylaxis. Heparin inhibits the coagulation function by prohibiting the activation of thrombin, factor Xa and other clotting enzymes (15). The anticoagulant function of heparin deeply depended on antithrombin III by binding it and developing an anticoagulant complex, which could increase the anticoagulant function more than one thousand times. APTT and TT would be prolonged significantly in ten minutes after venous injection with heparin while PT was not affected significantly in theory. Heparin was widely used to do prophylaxis for VTE, treat DIC, be extracorporeal anticoagulant and after cardiac infarction. However, some related adverse effects did exist, bleeding which was the most common complication, presenting various mucosa, joint cavity or wounds bleeding. Heparin-induced thrombocytopenia occurs when patients develop antibodies to the platelet factor 4 (PF4)/heparin complex following exposure to heparin products and could result in serious complications (3). Besides, there was a very low incidence of hypersusceptibility to heparin, long duration of heparin administration could also result in osteoporosis and bone fracture. All these side effects did not appear in our study. Recent years, there were many studies exploring the efficacy and safety profile of low- molecular-weight-heparin, showing a well outcome of low-molecular-weight-heparin even better than heparin (16,17). Therefore further prospective studies should be conducted to offer more strong evidence about low-molecular-weight-heparin and this would be a hot study point in future in major thoracic surgery for VTE prophylaxis.
The prophylaxis of VTE has been investigated much in all kinds of methods so far. Some studies found that the incidence of proximal deep-vein thrombosis for critically ill patients with medical or surgical admissions did not decrease, for comparison between dalteparin and unfractionated heparin. While a significant reduction was detected in the secondary end point of pulmonary embolism in the dalteparin group compared to unfractionated heparin group (18,19). Similar study design to ours for femoral neck fracture surgery operated with hemiprostheses, Leer-Salvesen et al. thought that postoperative start of LMWH resulted in a higher risk of postoperative death and reoperation than a preoperative start of prophylaxis (20), which supported early prophylaxis. As for the dosage of prophylaxis, there was a study finding that LMWH twice a day could provide more enough VTE prophylaxis efficacy but equal safety compared to once a day for patients undergoing selective esophagectomy. What was interesting was that a study showed not all patients with lung cancer including before and after surgery were in hypercoagulable states, however, either once or twice a day of LWWH was insufficient for those patients who were really in hypercoagulable states, therefore the cancer patients with real hypercoagulable states should be screened and accept sufficient thrombosis prophylaxis (21). Then other than heparin, there should be more studies to explore efficacy and safety of LMWH for thrombosis prophylaxis.
The strengths of this study are as follows. First, our study aimed to investigate the influence of preoperative usage of heparin on coagulation function after surgery and validated the safety of preoperative administration of heparin to supplement the relative black study area. Second, this is a prospective study which has a higher evidence grade. However, there are some limitations of our study that are inevitable. First of all, the amount of patients is small which relatively limits our data analytical power. What’s more, the result of our study is that postoperative coagulation function is differing significantly from preoperative data, though either preoperative data or postoperative result are all locating in normal range, which need more further study to prove with large sample. Further, because of lack of blank control group, the efficacy of preoperative administration of heparin cannot be compared and ensured. At last, the study is conducted is Chinese patients that the result is not applicable to other race owing to some study support the rate of thromboembolism may relate to race. In the future, more prospective randomized control trials are urgently asked to validate the proper administration of heparin.
Conclusions
In conclusion, this prospective study investigated the influence of preoperative administration of heparin on coagulation function of Chinese patients treated with thoracoscopic major thoracic surgery. Our study demonstrated that the preoperative usage of heparin did affect the coagulation parameters of the patients, but the postoperative coagulation parameters were all in normal range clinically, so this method did not actually influence the postoperative coagulation function clinically.
Acknowledgements
Funding: This work was supported by National Natural Science Foundation of China (No. 81672291, No. 31071210) (to YD Lin).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Ethics Committee of West China Hospital, Sichuan University (approval number: 20160601) and written informed consent was obtained from all patients.
References
- Song JQ, Xuan LZ, Wu W, et al. Low molecular weight heparin once versus twice for thromboprophylaxis following esophagectomy: a randomised, double-blind and placebo-controlled trial. J Thorac Dis 2015;7:1158-64. [PubMed]
- Monreal M, Mahe I, Bura-Riviere A, et al. Pulmonary embolism: Epidemiology and registries. Presse Med 2015;44:e377-83. [Crossref] [PubMed]
- Avidan MS, Smith JR, Skrupky LP, et al. The occurrence of antibodies to heparin-platelet factor 4 in cardiac and thoracic surgical patients receiving desirudin or heparin for postoperative venous thrombosis prophylaxis. Thromb Res 2011;128:524-9. [Crossref] [PubMed]
- Caprini JA. Thrombosis risk assessment as a guide to quality patient care. Dis Mon 2005;51:70-8. [Crossref] [PubMed]
- Deng HY, Shi CL, Li G, et al. The safety profile of preoperative administration of heparin for thromboprophylaxis in Chinese patients intended for thoracoscopic major thoracic surgery: a pilot randomized controlled study. J Thorac Dis 2017;9:1065-72. [Crossref] [PubMed]
- Blom JW, Doggen CJ, Osanto S, et al. Malignancies, prothrombotic mutations, and the risk of venous thrombosis. JAMA 2005;293:715-22. [Crossref] [PubMed]
- Di Nisio M, Peinemann F, Porreca E, et al. Primary prophylaxis for venous thromboembolism in patients undergoing cardiac or thoracic surgery. Cochrane Database Syst Rev 2015.CD009658. [PubMed]
- Falck-Ytter Y, Francis CW, Johanson NA, et al. Prevention of VTE in orthopedic surgery patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012;141:e278S-e325S.
- Ziomek S, Read RC, Tobler HG, et al. Thromboembolism in patients undergoing thoracotomy. Ann Thorac Surg 1993;56:223-6. [Crossref] [PubMed]
- Agnelli G, Bolis G, Capussotti L, et al. A Clinical Outcome-Based Prospective Study on Venous Thromboembolism After Cancer Surgery. Ann Surg 2006;243:89-95. [Crossref] [PubMed]
- Gómez-Hernández MT, Rodríguez-Pérez M, Novoa-Valentín N, et al. Prevalence of Venous Thromboembolism in Elective Thoracic Surgery. Arch Bronconeumol 2013;49:297-302. [Crossref] [PubMed]
- Hammond J, Kozma C, Hart JC, et al. Rates of venous thromboembolism among patients with major surgery for cancer. Ann Surg Oncol 2011;18:3240-7. [Crossref] [PubMed]
- De Martino RR, Goodney PP, Spangler EL, et al. Variation in thromboembolic complications among patients undergoing commonly performed cancer operations. J Vasc Surg 2012;55:1035-1040.e4. [Crossref] [PubMed]
- Smith JA. Malignancies, Prothrombotic Mutations, and the Risk of Venous Thrombosis. J Urol 2005;174:1300. [Crossref] [PubMed]
- Holbrook A, Schulman S, Witt DM, et al. Evidence-based management of anticoagulant therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012;141:e152S-e184S.
- Olson EJ, Bandle J, Calvo RY, et al. Heparin versus enoxaparin for prevention of venous thromboembolism after trauma: A randomized noninferiority trial. J Trauma Acute Care Surg 2015;79:961-8; discussion 968-9. [Crossref] [PubMed]
- Geerts WH, Jay RM, Code KI, et al. A comparison of low-dose-heparin with low-molecular-weight heparin as prophylaxis against venous thromboembolism after major trauma. N Engl J Med 1996;335:701-7. [Crossref] [PubMed]
- PROTECT Investigators for the Canadian Critical Care Trials Group and the Australian and New Zealand Intensive Care Society Clinical Trials Group, Cook D, Meade M, et al. Dalteparin versus Unfractionated Heparin in Critically Ill Patients. N Engl J Med 2011;364:1305-14. [Crossref] [PubMed]
- Li G, Cook DJ, Levine MA, et al. Competing Risk Analysis for Evaluation of Dalteparin Versus Unfractionated Heparin for Venous Thromboembolism in Medical-Surgical Critically Ill Patients. Medicine (Baltimore) 2015;94:e1479. [Crossref] [PubMed]
- Leer-Salvesen S, Dybvik E, Dahl OE, et al. Postoperative start compared to preoperative start of low-molecular-weight heparin increases mortality in patients with femoral neck fractures. Acta Orthop 2017;88:48-54. [Crossref] [PubMed]
- Attaran S, Somov P, Awad WI. Randomised high- and low-dose heparin prophylaxis in patients undergoing thoracotomy for benign and malignant disease: effect on thrombo-elastography. Eur J Cardiothorac Surg 2010;37:1384-90. [Crossref] [PubMed]


