Adenocarcinoma arising from an enteric cyst of the posterior mediastinum
Introduction
Mediastinal enteric cyst is a rare congenital cyst of the mediastinum, and occurs as a result of malformation during embryogenesis. Foregut cysts, which include bronchogenic, esophageal, and enteric cysts, make up 18% of all primary mediastinal masses (1). Mediastinal enteric cysts account for only 1–2% of all mediastinal cysts (2). A total of 60% of these cysts are found before the age of 1 year (3), and most of patients present with symptoms such as dyspnea, stridor, and cough. In adults, mediastinal enteric cysts are usually found incidentally because most of them are asymptomatic. Most of these cysts are benign and malignant changes in foregut cysts are rare (4). We report a rare case of adenocarcinoma arising from a posterior mediastinal enteric cyst.
Case presentation
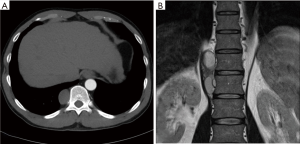
A 52-year-old man was found to have opacification in the right lower lung field on a chest X-ray by his annual check-up. Computed tomography (CT) showed a circumscribed mass measuring 5.8 cm on the major axis, in the right posterior mediastinum in the paravertebral location (Figure 1A). The mass consisted of two lesions, one central and the other peripheral, and the central lesion was slightly enhanced by contrast medium, while the other lesion had no enhancement. Magnetic resonance imaging (MRI) showed a fluid component at lesions without enhancement, which suggested cystic lesions. The central lesion showed a hypointense area in T1-weighted and T2-weighted images, which suggested solid components (Figure 1B). No elevation of serum tumor markers were found. Therefore, this tumor was suspected to be a neurogenic tumor with cystic change. The tumor was thoracoscopically resected with three ports under carbon dioxide insufflation (8 mmHg pressure at 4 L/min flow rate).
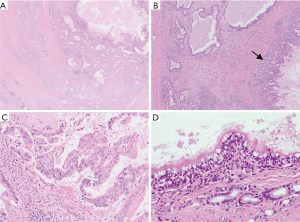
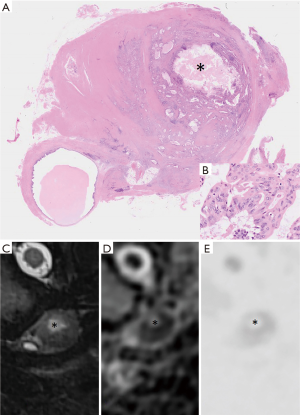
The resected mass was an oval-shaped cyst measuring 5.0 cm × 2.8 cm × 2.0 cm, with a white solid component, and had no continuity with the bronchus or the esophagus. The wall of the cyst had no cartilage and there was a smooth muscular layer. The inner surface of the cyst consisted of three parts; simple columnar epithelium, ciliated columnar epithelium and adenocarcinoma. And also, gastric mucous grands were identified in the cyst wall. Furthermore, grands formed by adenocarcinoma were extensively infiltrated over the cyst wall (Figure 2). Immunohistochemically, the tumor showed caudal-type homeobox protein (CDX) 2(+), cytokeratin (CK) 7(+), CK20(+), and thyroid transcription factor (TTF)-1(−), which indicated that this adenocarcinoma did not originate from the lungs. Besides, simple columnar epithelium showed CDX2(+), CK7(+), CK20(−), and TTF-1(−), while ciliated columnar epithelium showed CDX2(+), CK7(+), CK20(−), and TTF-1(+). These results indicated that the former epithelium had gastrointestinal origin, and the latter had respiratory origin. Based on operative findings and histological and IHC profiles, this specimen was finally diagnosed as adenocarcinoma originating from an enteric cyst. Comparing the microscopic findings of the specimen with MRI findings of the corresponding lesion, a hyperintense area in diffusion-weighted imaging (DWI) and a decline in apparent diffusion coefficient (ADC) values was matched with the distribution of atypical cells (Figure 3).
The patient had a good course and recovered uneventfully, and remained well 14 months postoperatively with no evidence of recurrence.
Discussion
We experienced a rare case of adenocarcinoma arising from an enteric cyst of the posterior mediastinum that was successfully resected with video-assisted thoracoscopic surgery (VATS).
Kirwan et al. (5) reported 41 patients with intrathoracic foregut cysts and classified them into three types: bronchogenic, esophageal, and enteric cysts. Bronchogenic cysts occur from extra lung buds, which develop from the primitive foregut. Esophageal cysts arise from isolated vacuoles, which also arise from the primitive foregut and usually fuse to form the lumen. Enteric cysts are thought to arise from persistence of the endodermal tube to the notochord, and form the traction diverticulum, which develops into enteric cysts (4). Enteric cysts are often associated with vertebral anomalies and usually located in the posterior mediastinum with attachment to the dorsal vertebra, and have no connection with the esophagus. These cysts are lined by either gastric mucosa with parietal and chief cells; duodenal, small intestinal, or large intestinal mucosae; or squamous or ciliated columnar epithelium (5).
In the present case, the patient was asymptomatic, and the posterior mediastinal mass was incidentally discovered, similar to previous cases. From the location of the mass, following differential diagnosis could be made; neurogenic tumors, lymphomas, teratomas and Mullerian cysts. Considering the patient was a middle-aged male with no elevation of serum tumor markers and fat attenuation or calcification couldn’t be identified on CT or MRI, our preoperative diagnosis was a neurogenic tumor with cystic change. However, pathological findings revealed the mass was an enteric cyst with adenocarcinoma. Immunohistochemical findings of simple columnar epithelium and adenocarcinoma, which were main constituent of the inner surface of the cyst, showed the absence of a lung marker or presence of a positive gastric or intestinal marker, and this supported the diagnosis. Although the cyst wall was ciliated in an extremely small proportion, enteric cysts could have not only gastrointestinal mucosa, but also ciliated or squamous epithelium (6). In addition, mediastinal Mullerian cysts also have ciliated columnar epithelium, but in our case, the cyst had gastrointestinal grands. Furthermore, all reported cases of mediastinal Mullerian cysts were occurred in female (7). Thus, we concluded that the cyst was to be an enteric cyst.
Malignant changes arising in enteric cysts are extremely rare. Only two cases of adenocarcinoma arising in an enteric cyst have been reported. Chuang et al. (8) first reported a 41-year-old man who had a superior posterior mediastinal mass without symptoms. A resected specimen showed an enteric cyst with adenocarcinoma. In the second case, Suzuki et al. (1) reported a 39-year-old man who had cough, back pain, and low-grade fever, and he had a cystic mass in the left posterior mediastinum. A specimen showed adenocarcinoma originating from an enteric cyst involving lung tissue. Furthermore, Tsubouchi et al. (9) reported a 36-year-old man with mucinous adenocarcinoma in the posterior mediastinum. The mass was lined by cuboidal and columnar epithelium with a smooth muscle layer and pools of extracellular mucin. Their immunohistochemical findings were similar to the present case, with CK7(+), CK20(+), and TTF-1(−). Their case was not diagnosed as adenocarcinoma arising from an enteric cyst, but it might be a third case.
CT scans are relatively inaccurate for distinguishing between cystic and solid masses (1). Some reports pointed out that MRI is useful to evaluate inner characteristics of mediastinal cystic masses (10), while there were few reports mentioned about the usefulness for malignant changes in those masses. We usually perform MRI to investigate the inner characteristics of those masses. We believe that MRI may help not only to distinguish between cysts and solid masses, but also to assess whether the mass has malignant changes or not by evaluating the findings of DWI and ADC map.
Although most enteric cysts are benign and malignant changes found in such cysts are extremely rare, clinicians should always keep in mind that these cysts have malignant potential and careful image evaluation, especially in MRI, would be recommended so as not to miss the appropriate chance for surgical resection.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Suzuki K, Koyama S, Yamada S, et al. Adenocarcinoma arising in a mediastinal enteric cyst. Intern Med 2007;46:781-4. [Crossref] [PubMed]
- Davis RD Jr, Oldham HN Jr, Sabiston DC Jr. Primary cysts and neoplasms of the mediastinum: recent changes in clinical presentation, methods of diagnosis, management, and results. Ann Thorac Surg 1987;44:229-37. [Crossref] [PubMed]
- Iglesias Sentís M, Belda Sanchís J, Gimferrer Garolera JM, et al. Mediastinal enteric cyst: unusual clinical presentation and histopathology. Arch Bronconeumol 2004;40:185-7. [Crossref] [PubMed]
- Olsen JB, Clemmensen O, Andersen K. Adenocarcinoma arising in a foregut cyst of the mediastinum. Ann Thorac Surg 1991;51:497-9. [Crossref] [PubMed]
- Kirwan WO, Walbaum PR, McCormack RJ. Cystic intrathoracic derivatives of the foregut and their complications. Thorax 1973;28:424-8. [Crossref] [PubMed]
- Shimosato S, Mukai K, Matsuno Y. Tumors of the Mediastinum. Afip Atlas Of Tumor Pathology Series 4 2010;11:307.
- Kobayashi S, Inoue T, Karube Y, et al. A case of Mullerian cyst arising in posterior mediastinum. Ann Thorac Cardiovasc Surg 2012;18:39-41. [Crossref] [PubMed]
- Chuang MT, Barba FA, Kaneko M, et al. Adenocarcinoma arising in an intrathoracic duplication cyst of foregut origin: a case report with review of the literature. Cancer 1981;47:1887-90. [Crossref] [PubMed]
- Tsubochi H, Kaneko K, Sakaguchi H, et al. Primary mucinous adenocarcinoma of the posterior mediastinum. Ann Thorac Surg 2013;95:2159-61. [Crossref] [PubMed]
- Takahashi K, Al-Janabi NJ. Computed tomography and magnetic resonance imaging of mediastinal tumors. J Magn Reson Imaging 2010;32:1325-39. [Crossref] [PubMed]


