Non-intubated anaesthetic technique in open bilobectomy in a patient with severely impaired lung function
Introduction
Minimally invasive surgical and anaesthetic techniques have become increasingly popular and undergone major developments over the last decade. One of these is non-intubated thoracic surgery (NITS), especially for video-assisted thoracic surgery (VATS) (1). This technique enables the maintenance of spontaneous ventilation throughout the operation, which has several theoretical advantages as compared to intermittent positive pressure ventilation (IPPV), including the avoidance of baro-, and volu-trauma (2). This may become even more important in patients with long standing history of chronic obstructive pulmonary disease (COPD), which requires particular protection from the harmful effects of IPPV. In the current case report we present the perioperative course of a patient scheduled for open bilobectomy.
Case presentation
A 73-year-old man (height: 178 cm, weight: 62 kg, BMI: 19.6) visited his local hospital due to extensive weight loss of more than 20 kg over 2 months and repeated serious hemoptysis. His past medical history included coronary artery bypass operation after an acute myocardial infarction, aortic abdominal aneurysm and hypertension. He was also a heavy smoker with two packs per day for 50 years.
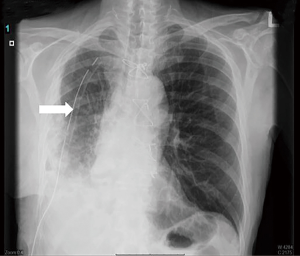
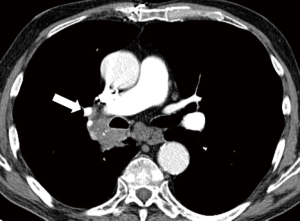
During the course of routine investigations, the chest computed tomography (CT) indicated bilateral emphysema and a 4.0 cm × 2.8 cm irregular solid tumour, which compressed the right main bronchus (Figure 1). The lower lobe was atelectatic, and the tumour infiltrated also the intermedial bronchus. Tissue mass was found in the right lower lobe and the intermedial bronchus with bronchoscopy and cytology showed basaloid adenocarcinoma (p40 positive, CK7 and TTF1 negative), which was later diagnosed—after surgery—as carcinoma epidermoides cornescens with peribronchiolar metastatic lymph nodes. The bone scintigraphy did not show any metastases. The results of pulmonary function test indicated severely impaired lung function with the forced expiratory volume in 1 second of 27%, the Tiffeneau index of 43% and the carbon monoxide diffusing capacity (DLCO) of 26%. The maximal oxygen consumption (VO2max) was 13.9 mL/kg/min. However, the calculated postoperative DLCO—preopDLCO × [1− (total number of segments to be resected/total number of lung segments)]—worked out of 19.16% and the predicted postoperative VO2max—preopVO2max × [1− (total number of segments to be resected/total number of lung segments)]—was 10.24 mL/kg/min indicating high postoperative risk for cardio-respiratory complications (3,4).
As we have gained substantial experience with NITS over the last year (more than 80 cases so far) with good results, we decided to choose this approach in order to avoid intubation and positive pressure one lung ventilation. Once this decision was made and discussed with the patient he was then scheduled for NITS open bilobectomy because of the previous frequent massive hemoptysis and due to the location and the extended infiltration of the tumour.
On arriving at the operating room standard monitoring of non-invasive blood pressure, electrocardiogram (ECG) and pulse oximetry was complemented with bispectral index (BIS) analysis. For continuous arterial blood pressure measurements and arterial blood sampling an indwelling arterial catheter was placed in the left radial artery. The patient was sedated with midazolam, fentanyl and asked to turn onto his left side. Anaesthesia was induced and maintained with propofol, which was administrated via target-controlled infusion titrated to a BIS of 40 to 60 throughout surgery. When the target BIS was achieved the airway was secured with a size 5.0 laryngeal mask. Spontaneous breathing was maintained throughout. Oxygen and air mixture was supplemented via T-piece at a fraction of inspired oxygen (FiO2) of 50% starting at flow rate of 6 L/min. FiO2 had to be increased to 100% before the resection. End tidal CO2 and FiO2 was continuously monitored via a side stream gas sampling, with the sampling line inserted into the laryngeal mask through an elastic seal on the T-piece.
Surgery
After skin infiltration with 2% lidocaine, the utility incision for VATS exploration at the 5th intercostals space was performed, followed by the 2–6th intercostal and vagal nerve infiltration above the azygos vein with 20 mL 0.5% bupivacaine under direct vision. Performing the block is facilitated by the total collapse of non-dependent lung, which takes place within a few minutes after opening the chest. On exploration the lower lobe seemed atelectatic and the tumour invaded the intermedius bronchus till beginning of the upper lobe bronchus containing the middle lobe bronchus as well, therefore the previously planned anterolateral thoracotomy and lower bilobectomy was performed. The intermedius bronchus was closed with hand sutures, at the level of the upper lobe. A mediastinal radical lymphadenectomy was also performed. The thorax was closed over a chest drain and a catheter was placed by the surgeons for continuous serratus anterior blockade in order to complement paravertebral blockade as our standard practice in NITS for postoperative pain relief.
Regarding anaesthesia, the NITS technique was well tolerated, hence conversion to endotracheal intubation was not required. The patient remained hemodynamically stable during the whole operation. Respiratory acidosis occurred (Table 1), but it remained in the tolerable range and it did not cause any respiratory distress to the patient. He maintained an oxygen saturation (SpO2) of 97–99% with a respiratory rate of 18–22/min.
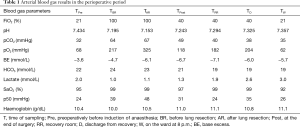
Full table
After the surgery was completed the patient was woken up then asked to cough and breathe deeply to re-expand the collapsed lung. Then he was transferred to the recovery room. Soon after arrival the first blood gas was taken, which showed that his respiratory acidosis was resolving. After one hour he drank water and in bed mobilisation was also started. He was discharged from recovery with stable vital signs 5 hours after the operation.
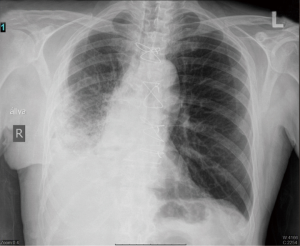
Postoperative pain was well controlled by the serratus anterior blockade with 0.5% bupivacaine infused at 5 mL/h, which was also supplemented with intravenous or oral paracetamol and tramadol as indicated by visual analogue scores (VAS) of more than 4. The VAS varied between 1 to 5 during the first postoperative day. The patient’s mobilisation was continued and the chest tube was removed on postoperative day 5 (Figure 2) and he has transferred to a pulmonology ward on day 7 (Figure 3), fully mobilised and without any oxygen demand after day 2.
Discussion
Minimally invasive surgical and anaesthetic techniques are becoming more and more popular even for major surgery. In thoracic surgery, general anaesthesia with endotracheal intubation and one-lung ventilation (OLV) has been the gold standard technique for decades. However, minimally invasive thoracic surgery has opened up new frontiers, which renders the need for the development of novel anaesthetic techniques.
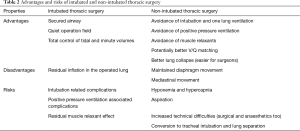
Numerous type of thoracic procedures can be carried out with non-intubated techniques. Patients for NITS should be selected carefully but most of the exclusion criteria are relative contraindications depending on the team’s experience (5) (Table 2). It is important to note that instead of sedation—a technique most often used in previous reports (6)—we aimed for surgical depth of anaesthesia (confirmed by BIS monitoring), hence insertion of laryngeal mask could be performed, which provided airway patency and safer control of the airway.
Full table
General anaesthesia with one-lung IPPV also has several complications, which can increase perioperative morbidity and even mortality (7). Mechanical ventilation itself might cause pressure induced lung injury, damage caused by lung overdistension, shear stress of repetitive opening, closing of alveoli and increased inflammatory response due to elevated release of pro-inflammatory mediators (8,9).
In a mechanically ventilated patient, OLV in lateral decubitus position produces ventilation/perfusion (V/Q) mismatch, because the non-dependent lung is perfused but not ventilated. In a spontaneously breathing patient theoretically, there is a better match between ventilation and perfusion due to the more efficient diaphragmatic movements. During OLV the non-dependent lung is not ventilated, its perfusion decreases rapidly due to hypoxic pulmonary vasoconstriction (HPV), which is important to maintain acceptable V/Q results in the dependent lung (10). However, it is often the case that due to lung tissue gravity and surgical manipulations significant right to left intrapulmonary shunt occurs. The effectivity of HPV is influenced by the lung volume. If the delivered tidal volumes and intrapulmonary pressures overstretch the ventilated alveoli, blood flow may be diverted to the non-ventilated alveoli attenuating the HPV response and leading to increased V/Q mismatch and worsening hypoxemia (11).
In non-intubated patients, once the surgical pneumothorax is present, the negative pressure is lost and paradoxical breathing pattern occurs (12). During inspiration the normal atmospheric pressure in the open thorax pushes the mediastinum towards the dependent hemithorax and on expiration a reverse phenomenon occurs. Perfusion to the dependent lung is better as compared to OLV due to the low or negative pressure in this lung. Intrapulmonary shunt may also be reduced due to the intact diaphragmatic movements.
One of the possible complications of this technique is that after resection of the lung, the airway remains open until the bronchi are sutured. During this phase blood can enter into the airways and may cause aspiration pneumonia in the postoperative period. Therefore, to keep the airways clean requests delicate handling of the lung by the surgeon, and the anaesthetist can also perform fiberoptic bronchoscopy via the laryngeal mask if needed.
Hypercapnia is a common phenomenon during NITS procedures, but this is often present during OLV as well. During NITS, alveolar gases may communicate between the dependent and non-dependent lungs while surgical pneumothorax is present, causing carbon dioxide rebreathing causing hypercapnia (13). Another factor is hypoventilation, which is due on the one hand to the collapsed operated lung and on the second hand to anaesthesia related central respiratory depression. Fortunately, accumulation of CO2 is not necessarily harmful in the perioperative period (13,14). PaCO2 levels up to 70 mmHg are likely to be well tolerated by most patients. However, in patients with pulmonary hypertension, severe cardiac comorbidities or in case of increased intracranial pressure, acute hypercapnia should be avoided.
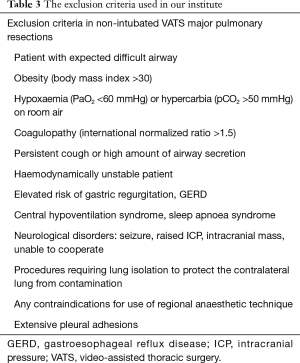
One of the most important message of this report is the risk stratification. According to our experience NITS is a safe approach, but the selection of patients is important. Our general exclusion criteria are summarized in Table 3. In this particular case, although preoperative VO2max of 13.9 mL/kg/min is regarded as borderline by current guidelines, but the calculated postoperative DLCO and VO2max indicated high postoperative risks of complications. To avoid it we decided to proceed with the NITS technique, taking into consideration all of the potential benefits of maintained spontaneous breathing.
Full table
Finally, we also have a “contingency plan” for unforeseen events during the NITS procedures, including fiberoptic intubation via the laryngeal mask and lung separation with a bronchial blocker. Fortunately, there was no need for any rescue interventions in this case.
Conclusions
In the current case report we presented a high-risk patient with severely impaired lung function in whom NITS was applied successfully even during open thoracotomy. To our knowledge this is the first case report to show that NITS is a feasible and safe approach in open thoracotomy.
It is expected that the less invasive non-intubated techniques will gain ground in the future in thoracic surgery for most thoracoscopic interventions but may also become a feasible less invasive alternative in certain procedures requiring thoracotomy. Our case report may serve as some reassurance for those who are willing implement this technique in their practice.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Pompeo E. State of the art and perspectives in non-intubated thoracic surgery. Ann Transl Med 2014;2:106. [PubMed]
- Mineo TC, Pompeo E, Mineo D, et al. Awake nonresectional lung volume reduction surgery. Ann Surg 2006;243:131-6. [Crossref] [PubMed]
- Brunelli A, Charloux A, Bolliger CT, et al. ERS/ESTS clinical guidelines on fitness for radical therapy in lung cancer patients (surgery and chemo-radiotherapy). Eur Respir J 2009;34:17-41. [Crossref] [PubMed]
- Brunelli A, Kim AW, Berger KI, et al. Physiologic evaluation of the patient with lung cancer being considered for resectional surgery: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e166S-e190S.
- Gonzalez-Rivas D, Bonome C, Fieira E, et al. Non-intubated video-assisted thoracoscopic lung resections: the future of thoracic surgery? Eur J Cardiothorac Surg 2016;49:721-31. [Crossref] [PubMed]
- Chen KC, Cheng YJ, Hung MH, et al. Nonintubated thoracoscopic lung resection: a 3-year experience with 285 cases in a single institution. J Thorac Dis 2012;4:347-51. [PubMed]
- Kiss G, Castillo M. Non-intubated anesthesia in thoracic surgery-technical issues. Ann Transl Med 2015;3:109. [PubMed]
- Tacconi F, Pompeo E, Sellitri F, et al. Surgical stress hormones response is reduced after awake videothoracoscopy. Interact Cardiovasc Thorac Surg 2010;10:666-71. [Crossref] [PubMed]
- Vanni G, Tacconi F, Sellitri F, et al. Impact of awake videothoracoscopic surgery on postoperative lymphocyte responses. Ann Thorac Surg 2010;90:973-8. [Crossref] [PubMed]
- Liu YJ, Hung MH, Hsu HH, et al. Effects on respiration of nonintubated anesthesia in thoracoscopic surgery under spontaneous ventilation. Ann Transl Med 2015;3:107. [PubMed]
- Nagendran J, Stewart K, Hoskinson M, et al. An anesthesiologist's guide to hypoxic pulmonary vasoconstriction: implications for managing single-lung anesthesia and atelectasis. Curr Opin Anaesthesiol 2006;19:34-43. [Crossref] [PubMed]
- Kao MC, Lan CH, Huang CJ. Anesthesia for awake video-assisted thoracic surgery. Acta Anaesthesiol Taiwan 2012;50:126-30. [Crossref] [PubMed]
- Kregenow DA, Swenson ER. The lung and carbon dioxide: implications for permissive and therapeutic hypercapnia. Eur Respir J 2002;20:6-11. [Crossref] [PubMed]
- Pompeo E, Rogliani P, Tacconi F, et al. Randomized comparison of awake nonresectional versus nonawake resectional lung volume reduction surgery. J Thorac Cardiovasc Surg 2012;143:47-54, 54.e1.