Principles and indications of extracorporeal life support in general thoracic surgery
Introduction
The role of extracorporeal life support (ECLS) has expanded rapidly over the past 15 years to become an important tool in advanced general thoracic surgery practice. Intra-operative and in some cases continued post-operative ECLS is redefining the scope of complex surgical care. ECLS encompasses a spectrum of temporary mechanical support that may remove CO2, oxygenate or provide hemodynamic support or a combination thereof. The most common modalities used in general thoracic surgery include extracorporeal membrane oxygenation (ECMO), interventional lung assist device (iLA® Novalung®, Heilbronn, Germany), and extracorporeal CO2 removal (ECCO2R). The ECMO and Novalung® devices can be used in different modes for the short term or long-term support depending on the situation.
History
ECMO has been used for respiratory failure since the 1970s and became an established therapeutic option in neonates with hyaline membrane disease. In adults, however, it was occasionally used for rescue therapy, but the morbidity and mortality were high and thus the option was only considered in desperate situation. The devices that were used for ECMO were typically minimally modified cardiopulmonary bypass (CPB) circuits that were brought to the intensive care unit. Specifically, the oxygenators were designed to work for several hours, not for days. Therefore, the membrane oxygenator would progressively deteriorate leading to an air-blood interface with severe inflammatory reaction and major morbidities.
In the early 2000s, a dramatic change occurred with the development of modern membrane technology that prevented plasma leakage despite prolonged utilization. These new membranes were incorporated into low resistance oxygenators that were, for the first time, designed and approved for the long-term use. This change combined with the widespread introduction of centrifugal pumps and heparin-coated circuits led to a radical change in ECLS practice. The devices could be used much more safely for several days or weeks with limited inflammatory reaction. Studies demonstrated significantly less bleeding, less platelet dysfunction, fewer ECMO circuit malfunctions even with oxygenators that remained in place for up to 4 weeks (1). The use of iLA® devices was initially reported in thoracic surgery as a bridge to lung transplantation in a series of 12 patients between 2003 and 2005 (2). The potential impact of new ECLS devices on outcome in respiratory failure became more apparent during the influenza outbreak of 2009 (3). Contemporaneously, the CESAR trial in the United Kingdom demonstrated a 6-month survival benefit with ECMO use versus optimal conventional ventilator management of ARDS (4). More recently, the feasibility of transporting critically ill patients from outside facilities to specialized ECLS-capable centres was confirmed using streamlined ECLS circuits. The success of ECLS in these settings has led general thoracic surgeons to adapt this technology for elective general thoracic surgery as a tool to manage hypercapnia, provide oxygenation and for hemodynamic support.
Differences between ECLS and CPB
Historically, full CPB has been the most typical form of extracorporeal mechanical gas exchange support for complex thoracic surgery. However, CPB requires full heparinization, potentially increasing transfusion requirements, and can lead to an inflammatory response with the risk of lung injury. In contrast, ECLS technology requires minimal amount of heparinization. In addition, technological benefits with ECMO include the miniaturization of circuits requiring lower priming volumes, limited air/blood contact by closed circuits without cardiotomy suction/reservoir, and improved biocompatibility of material used in circuit components (5) making them suitable for long term use (Table 1).
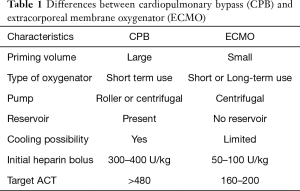
Full table
Components of the ECLS circuit
As previously mentioned, the equipment used for mechanical cardiac or respiratory support has evolved from components of CPB for cardiac surgery. The original ECLS circuits were adapted from CPB and comprised an oxygenator, pump, heater and minimal volume circuit with no reservoir. They were always placed with inflow from a vein and outflow into an artery. While these basic components remain the same, multiple cannulation options and different circuit configurations have been developed for specific clinical requirements.
Oxygenators
Modern oxygenators have a tightly packed hollow fiber design, with oxygen enriched air circulating within the tubing and blood outside of the tubing. This compact structure provides a high membrane area for a short diffusion pathway, and very low resistance to flow, thereby reducing trauma to the cellular element of blood to a minimum. For example, the Novalung® iLA® has reduced the resistance to a minimum with a pressure gradient of 15 mmHg being sufficient to generate a flow of 2.5 L/min across the membrane (6).
When microporous membrane oxygenators replaced bubble oxygenators in the 1970’s, first silicone membranes, then polypropylene membranes were used. More recently, hollow fiber oxygenator membranes are made of polymethylpentene (PMP) that is more resistant to plasma leakage resulting in a much-reduced blood/air interface. This leap in membrane technology has resulted in vastly improved long-term gas exchange and a reduced rate of oxygenator failure (1,2). The rate of gas exchange along the fibres is dependent on both the gas flow (sweep) and blood flow thereby modifying the partial pressure difference of oxygen and carbon dioxide across the membrane. Oxygenation is mainly a function of blood flow, while CO2 removal can be modified by regulating the sweep.
Hollow fiber oxygenators are susceptible to the formation of fibrin clots decreasing their efficiency over time. When clot and fibrin accumulates on the oxygenator, the pressure gradient across the membrane increases, and the pump needs to generate higher pressure to maintain blood flows through the circuit. Formation of clot may be due to inadequate anticoagulation, areas of stasis or low circuit blood flows. This problem may be detected by daily inspection the upstream and downstream membrane surfaces of the oxygenator with the help of a flashlight. Monitoring oxygen content before and after the membrane is also helpful, when efficiency decreases, the oxygenator may be changed at the bedside. In most patients this is required only after weeks of support. If a significant amount of clot forms on the downstream side, there is a risk of embolization to the patient and a switch of oxygenator may be warranted.
Pump (when applicable)
Both roller pumps and centrifugal pumps are in clinical use in CPB circuits. In ECLS centrifugal pumps are used almost exclusively as they cause less hemolysis in long-term use. A centrifugal pump is composed of a disposable cone that sits on top of a spinning magnet and is rotated via magnetic coupling. The centrifugal force generated by this rotation creates a pressure differential across the cone, which drives the blood flow. Pump flow is determined by this pressure difference, as well as preload and afterload, in a non-linear manner. There is limited potential to increase the cardiac output by turning up the revolutions per minute, as decoupling of the magnets may occur. Compared to CPB, the amount of flow is limited much more by technical design of the pump. Centrifugal pump flows are dependent on both preload and afterload conditions. If inflow drops either from decreased preload or from drainage line occlusion, the centrifugal pump generates negative pressure and the cone slows down causing a drop in flow. Clinically this is observed as chattering of the drainage line requiring restoration of either the patient’s intravascular volume, or catheter patency to maintained desired flow. If afterload is suddenly increased, the pressure difference across the pump drops and slows flow. When ECLS flows are drastically reduced, support provided by the device is necessarily nearly halted, potentially resulting in respiratory compromise or hemodynamic collapse until the problem is identified and rectified.
Reservoir, circuit, connectors
A significant step in the evolution of CPB circuits to ECLS systems was the shortening of lines and the removal of components such as the venous reservoir. This has the effect of reducing the priming volume required for an ECLS circuit, minimizing hemodilution. Vascular access catheters and circuit tubing are now heparin-coated. The removal of the venous reservoir eliminates the potential pooling of static blood, and any air/blood interface, resulting in dramatic decrease in anticoagulation requirement (activated clotting times of 160–200 seconds compared to >480 seconds for CPB) (7). As the ECLS circuit is completely closed, the risk of accidental air entrainment is much reduced. Unlike a CPB circuit however, there are no infusion ports therefore all drugs, blood products and intravascular volume replacement must be delivered by direct intravenous access into the patient. Blood shed during surgery cannot be immediately re-transfused but must be processed in a cell saver prior to re-infusion.
ECLS configurations
The choice of ECLS configuration is made depending on the required application, with varying levels of gas exchange capacity and hemodynamic support (Table 2).
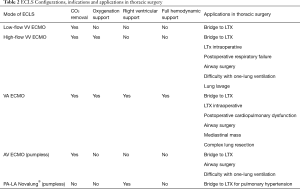
Full table
Veno-venous ECMO
VV-ECMO is used in refractory respiratory failure and requires only peripherally placed venous catheters. Blood is drained from and re-infused into central veins. In the most common configuration with early use of VV-ECMO deoxygenated blood drained via a femoral catheter, was actively pumped though the membrane oxygenator and returned via a jugular catheter. Oxygenated blood is re-infused into the right atrium (RA) and ejected into the pulmonary circulation by the patient’s own cardiac output, mixing with the deoxygenated venous return. VV-ECMO has no direct effect on cardiac function, however myocardial dysfunction associated with hypoxia and respiratory acidosis will improve. Additionally, oxygenated blood entering the pulmonary circulation will reduce hypoxic pulmonary vasoconstriction, increasing the shunt fraction but decreasing right heart afterload. It is not unusual for depressed right ventricular function to improve after institution of VV-ECMO. Trans-esophageal echocardiography (TEE) assessment of the re-infusion cannula is helpful, the recommended position of the tip is in the RA just beyond the SVC/RA junction, a safe distance away from the intra-atrial septum and the tricuspid valve (8).
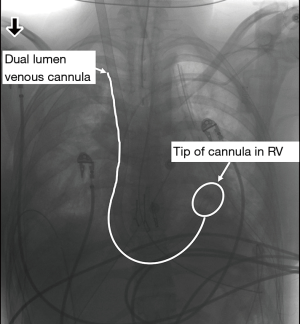
The development of bi-caval dual lumen catheters allowed for inflow and outflow from a single percutaneous site, usually the right jugular vein. Optimal cannula positioning is essential for good oxygenation, specifically the infusion jet should be directed towards the tricuspid valve. TEE assessment of position and flow is very helpful. Fluoroscopy, however, is the optimal mode of placement of the cannula into the IVC to avoid any misdirected cannula ending into the right ventricle with risk of perforation (Figure 1). By avoiding femoral cannulation, patient mobilization is improved and participation in rehabilitation is possible.
In VV-ECMO there is a functional dissociation of decarboxylation and oxygenation. Oxygenation varies primarily with blood flow through the membrane oxygenator, while CO2 removal is dependent of the gas sweep across the membrane. Adequate CO2 removal can therefore be performed at low flow (about 1.0 L/minute) via small sized cannula (9). Oxygenation in contrast varies with the ratio of the circuit blood flow to the patient’s cardiac output and therefore blood flows of 3–6 Liters/minute are typically required to maintain acceptable oxygenation in patients with severe lung injury. Higher range of ECMO blood flow is also required to oxygenate an unventilated surgical patient with a hyperdynamic circulation. VV-ECMO flows of 60% of cardiac output are required to maintain arterial oxygen saturation of over 90% (10). In this situation, two single stage cannulas in the femoral and jugular veins are necessary as the dual lumen cannula may not provide sufficient venous return. If the lungs are not severely injured and can be partially ventilated with oxygen, oxygenation can be maintained with lower flows.
In VV-ECMO, recirculation of blood between the reinfusion and drainage catheters can occur. The intent is for the oxygenated return blood to pass through the tricuspid valve, therefore the reinfusion ports should be in the RA. Oxygenated re-infused blood may flow into a single lumen drainage catheter if the catheters are too close together. Recirculation can also occur with bi-caval dual lumen catheters particularly if malpositioned and when higher flow rates are used, but is less common than with two catheter configurations. Echocardiography using color doppler can be useful for assessing ECMO cannula positions and direction of flows. The IVC cannula should be below the hepatic vein, SVC cannula should be at the SVC-RA border, and double-lumen cannulas should have the return port pointed at the tricuspid valve.
Veno-arterial ECMO
VA-ECMO is used for hemodynamic support with or without respiratory failure. Blood is drained from the venous side and re-infused in the arterial system. The cannulation can be performed either centrally if VA-ECMO is required intra-operatively, or peripherally if VA-ECMO is required pre- or post-operatively. The femoral vessels are most often used for cannulation in peripheral VA-ECMO in adults. Central and peripheral cannulation can be combined with for instance blood drained from the RA and pumped through the membrane oxygenator to be re-infused in the femoral artery. Alternatively, the blood can be drained from the femoral vein and reinfused into the aorta.
Physiological effects include unloading of the right ventricle and pulmonary vasculature; when ECMO blood flows are high, much of the patient’s venous return bypasses the pulmonary circulation. While organ perfusion pressure is improved, left ventricular afterload is increased as blood from the ECMO circuit is re-infused at arterial pressure. Because of the large size of the femoral arterial cannula required, distal limb perfusion may be compromised and a distal arterial perfusion catheter is routinely placed if prolonged peripheral VA-ECMO is required pre- or post-operatively. Disadvantages of VA-ECMO include the risk of arterial cannulation: arterial injury, bleeding and embolism, distal limb ischemia and cardiac thrombus if low flows are maintained through the heart. Another disadvantage is the competing flow ejected from the left ventricle that may be hypoxic if the lungs are severely dysfunctional. This can create a “harlequin syndrome” , which is associated with a risk of cardiac injury or stroke as hypoxic blood perfuses the coronary and the right brachiocephalic artery territory. Hence, oxygen monitoring of the right hand is critical in the setting of peripheral VA ECMO through the femoral vessels. The “harlequin syndrome” can be managed by increasing the flow through the VA-ECMO, thus decreasing the blood flow through the lungs. The replacement of inotropes by purely vasopressor medications may also be helpful. Other alternatives include either adding a new arterial cannula in the right axillary artery (in addition to the femoral artery cannula) to perfuse the right brachiocephalic territory with oxygenated blood, or adding a new venous cannula into the jugular vein (in addition to the femoral vein cannula) in order to configure the system into veno-venous-arterial ECMO thus perfusing the lungs with oxygenated blood via the oxygenated venous return to the jugular vein. TEE can be used to assessing the drainage cannula position, ideally in the lower part of the RA, and decompression of the right side of the heart, as well as overall heart function.
Central cannulation directly in the RA and ascending aorta enables placement of larger cannula and higher ECMO blood flows but requires an open chest and is generally reserved for operative cases that require hemodynamic support, including lung transplantation.
Patients on VV-ECMO for respiratory failure who subsequently develop hemodynamic instability can be supported by the addition of an arterial cannula for a hybrid configuration called veno-veno-arterial ECMO. Both venous catheters are used for drainage into a single ECMO circuit with re-infusion via a third arterial catheter.
AV ECMO (pumpless)
The Novalung® interventional lung assist device is a low-resistance gas exchanger designed for pulsatile blood flow driven by the patient’s cardiac output. A drainage catheter is inserted into a femoral artery and reinfusion catheter into a femoral vein. The two are connected to the Novalung® via a short, pumpless circuit. The blood flows generated are dependent on cardiac function and arterial blood pressure and are in the range of 0.5 to 2.5 L/min. This allow full decarboxylation, but only partial oxygenation, so this modality is particularly useful for treating hypercarbic respiratory failure (9). Pumpless configurations have the advantage of simplicity, greater portability, and low priming volumes. They are practical for inter-hospital transport (11). This option however is being replaced by the less invasive ECCO2R technology, which has similar indication but only requires a small venous cannula and allows ambulation.
PA-LA Novalung® (pumpless)
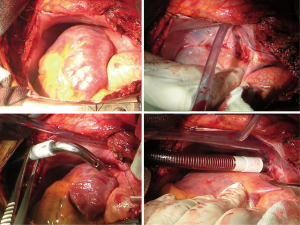
Another pumpless configuration is applicable only to patients with pulmonary hypertension and impending right heart failure. The Novalung® is connected via a short tubing circuit between a drainage cannula placed directly into the main PA and re-infusion catheter inserted in the left atrium via the right upper pulmonary vein (Figure 2). High right sided pressures drive the flow through the low resistance Novalung®. Functionally this creates an oxygenated right to left shunt that has the effect of unloading the right ventricle, reduced septal shift, allowing better left ventricle filling and coronary perfusion and leading to improved right ventricular function. This modality involves central cannulation via a sternotomy; patients who are awake but hemodynamically unstable may need femoral cannulation for peripheral VA-ECMO to safely tolerate the induction of general anesthesia, with planned weaning when the right heart is decompressed immediately after implanting the PA-LA Novalung. Intraoperative TEE does not direct the cannula positioning, however is vital for assessing adequate unloading of the right ventricle and the status of left ventricular function. It is essential to verify that the left ventricle is able to tolerate increased blood flow without failing. In the event of left ventricular decompensation, VA-ECMO would be required. At the end of the procedure, the PA and LA cannulae are advanced through the skin of the upper abdomen and the chest closed (Figure 3). Used as a bridge to transplant, many patients can be extubated and subsequently mobilized (12,13).

Applications in thoracic surgery
Currently most applications of ECLS in thoracic surgical practice are described in case reports, small case series and reviews. In some centers lung transplantation is performed by general thoracic surgeons, and only in this patient population are larger case series documented, with long term outcome data available.
Airway surgery
ECMO may be used to support patients with critical airway obstruction. Lesions above the larynx may be managed with awake fibreoptic intubation or tracheostomy under local anesthesia. When severe obstruction is encountered below the larynx, while intubating the vocal cords may not be difficult, ventilation may be impossible. While some lesions may be managed by rigid bronchoscopy and debridement with intermittent ventilation; extensive tracheal obstruction, need for prolonged debridement and significant bleeding into the airway present formidable problems. Historically full CPB support was instituted via femoral venous and arterial catheters placed under local anesthesia (14). More recently, VV-ECMO support has been reported for endotracheal tumor resection (15,16), dislodged stents (15,17), foreign body removal (18), control of hemoptysis (19), debridement of papillomatosis (20) and relief of external compression (15,21,22) in adults. A variety of cannulation strategies have been reported: femoral and jugular single lumen catheters (15,18,20) and bi-caval dual lumen catheter in the right jugular vein (16,22) have been described. Death as a result of post resection hemoptysis has been reported and was likely exacerbated by anticoagulation for ECMO (15). Relief of airway obstruction in small children has been performed with both VV and VA ECMO (23).
Emergency VA and VV ECMO has been reported after resuscitation from cardiopulmonary arrest due to airway obstruction (16,17). While VV support was successful in a hypoxic patient where hemodynamic stability had been restored, if there is post arrest myocardial dysfunction, VA ECMO is a better choice. In both reports, ECMO support was maintained during restoration of airway patency followed by conversion to conventional mechanical ventilation, a short period of observation to assess for neurological sequelae, and eventually successful extubation.
An additional challenge presented by tracheal resection and reconstruction is continued oxygenation intra-operatively with an open airway. Distal airway management typically involves cross-field ventilation with an endotracheal tube or jet ventilation with a tracheal catheter, both of which may obstruct the surgical field. Complex reconstruction may be facilitated with ECMO support, as can open airway procedures in patients with limited respiratory reserve (24,25). Advanced tumors requiring extensive en-bloc resection have been managed with VA ECMO due to the need for vigorous retraction of the heart and great vessels. Both central and peripheral cannulation has been described (24) VV ECMO support is more often reported and is suitable for tracheal and carinal resection including carinal pneumonectomy (26-28). An unusual case of repair of a complex tracheoesophageal fistula was reported using pumpless AV ECMO for CO2 removal. Apneic oxygenation was provided via a small endotracheal tube at the carina, allowing 12 hours of surgery without ventilation of the lungs (29). Tracheal resection has also been described with AV ECMO (30). When VV-ECMO provides insufficient oxygenation during tracheal surgery, supplemental catheter oxygen insufflation had also been used (27). ECLS during airway surgery has been recently described in an extensive review (31). While ECLS was noted to facilitate optimal exposure while maintaining oxygenation, this was at the cost of increased bleeding due to heparinization.
Difficult or impossible one lung ventilation (OLV)
Patients under consideration for thoracic surgery may have limited pulmonary reserve, making oxygenation with one lung ventilation impossible. Post pneumonectomy patients have undergone contralateral wedge resection and segmentectomy for second malignancies (28,32), VATS bullectomy (33) and esophagectomy (34) with VV ECMO support. A low-flow VV ECMO was noted to occasionally be sufficient in patients at risk of severe hypercapnia. Pumpless AV ECMO has also been used to facilitate wedge resection and decortication in post pneumonectomy patients (30).
There are no guidelines to determine which patients will need extracorporeal support, and who will tolerate the procedure without. Arterial PaO2 on two lung ventilation, FEV1/FVC ratio and side of operation are usually good predictors of hypoxia on one lung ventilation (35), however this information may be limited on critically ill patients and may not reflect new pulmonary co-morbidities such as empyema or air leak. For instance, patients with necrotizing pneumonia may require VV ECMO intraoperatively to allow aggressive decortication of the empyema (36). Bilateral decortication of critically ill patients on VV ECMO may also be a crucial step to facilitate weaning from ECMO, followed by successful extubation (37).
Patients with emphysema are prone to ruptured bullae and prolonged air leaks. Thus, VATS resection of bullae has been performed with both VV-ECMO support (28,38) and AV-ECMO (30). In the late 1990’s elective intraoperative initiation of ECMO was used to support three COPD patients with severe hypercapnia undergoing lung volume reduction surgery (LVRS), who did not meet standard selection criteria for this procedure (39). VA ECMO was chosen due to the anticipated hemodynamic instability often seen with positive pressure of patients with pulmonary hyperinflation. This must be described as a controversial treatment plan as severe hypercapnia is a risk factor for perioperative mortality. This practice has not been reported by other surgical centers. VV ECMO has been used to facilitate LVRS/major bullectomy to liberate COPD patients from mechanical ventilation (40,41). Additionally VV-ECMO has been used to enable patients with significant loss of lung parenchyma to tolerate resections: metastasectomy after prior extensive lung resection (28) and resection of aspergilloma (42) after scarring from tuberculosis have been reported.
Finally, patients with alveolar proteinosis with progressive hypoxia require whole lung lavage of both lungs with large volumes of saline to remove lipoprotein deposits. Most often this is performed sequentially via a double-lumen tube, but patients with critically impaired gas exchange may not tolerate this, and there are many case reports describing the use of VV ECMO support in this situation (43,44).
Mediastinal masses
Large masses occupying the anterior mediastinum have the potential to cause compression of the trachea, great vessels and RA following induction of general anesthesia. In the awake patient, the negative pressure generated by inspiration reduces this effect so that compression is minimal until surgical disease is advanced. This is abolished by muscle relaxants, and positive pressure ventilation can precipitate central airway obstruction or catastrophic reduction of cardiac output and cardiopulmonary arrest. This is a particular risk for children with large anterior lymphomas. Historically this has been treated with CPB support (45,46). More recently, pre-induction femoral VA-ECMO while maintaining spontaneous ventilation has been described in children (47) and adults (48). The VA configuration is warranted by the potential for cardiovascular collapse.
Advanced surgical resections
Tertiary referral centres are increasingly undertaking resection of advanced lung and esophageal malignancies as part of multimodal therapy and reporting reasonable survival (49-53). Resection of lung malignancies with reconstruction of superior or inferior vena cava, left atrium, distal aorta, and carina has been described with VA ECMO support (52) as have esophageal malignancies invading the carina (5). Cannulation sites are chosen according to the planned resection and may be central or peripheral (52). Resection of complex thoracic malignancies with extension into the pulmonary trunk, the aortic arch or the heart requiring opening of a cardiac chamber are only amenable to traditional CPB (52,54-56).
Thoracic emergencies
ECMO has been described as a lifesaving emergency treatment of massive hemoptysis (19,57,58). In thoracic surgery, iatrogenic injury to large vessels with massive bleeding is most often managed with CPB, which provides the advantages of rapid infusion, auto-transfusion and delivery of cardioplegia for cardiac arrest or deep hypothermic circulatory arrest if needed (5). In the event of pulmonary artery (PA) injury the reduction of blood flow through the pulmonary trunk enables surgical repair (5,59). ECMO can be of benefit in tracheal injuries to facilitate tracheal repair without tension (25,60).
ECMO for primary graft dysfunction is frequently required after lung transplantation, to support the lungs while reperfusion injury abates, but has also been instituted emergently for other peri-operative etiologies of lung failure. These include hemodynamic stabilisation in patients with acute severe pulmonary embolism (61) to allow pulmonary embolectomy (62,63), reperfusion injury after pulmonary thrombendarterectomy (64,65) for chronic thromboembolic pulmonary hypertension, the indications and methodology of which have recently been reviewed (12). Support for postoperative transfusion-associated lung injury (TRALI) is also well-described (66,67). The importance of advanced planning for emergencies and effective multidisciplinary team-working has recently been emphasised in maintaining good patient outcomes (5). In addition, ECMO has been used outside the thoracic operating rooms as part of resuscitation and surgical repair for thoracic trauma (36,68,69).
The choice of VV versus VA ECMO in emergency circumstances dependent on the need for primarily oxygenation versus the need for concomitant hemodynamic support. When urgent ECMO is instituted intraoperatively, available venous and arterial cannulation sites may be dictated by patient position and available vessels (5) (Table 3).
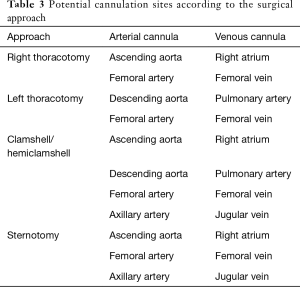
Full table
Lung transplantation
ECMO is being used at an increasing number of specialized centers to bridge deteriorating patients with end-stage lung disease to lung transplant surgery. ECMO bridged patients are at increased risk of peri-operative morbidity and mortality, but do have acceptable one-year survival (70). Many patients with hypercapnic respiratory failure can be bridged with pumpless AV ECMO or preferably low flow VV ECMO. Those with significant hypoxia will require full flow VV or if hemodynamically unstable, peripheral VA ECMO. In the subgroup with severe pulmonary hypertension VA ECMO or PA-LA Novalung® is used (13).
Lung transplant surgery is characterized by hemodynamic and respiratory compromise, the most challenging being systemic hypotension, pulmonary hypertension and hypoxemia. ECMO is supplanting CPB as the favored form of ECLS to stabilize patients. Typically, when ECMO is initiated intraoperatively, a VA ECMO configuration via central cannulation sites is used. In a recent case control cohort study of patients requiring intra-operative cardiopulmonary support, those managed with ECMO had better early outcomes including duration of mechanical ventilation, ICU and hospital length of stay than patient who went on CPB. Blood product usage was significantly less in the ECMO patients (71).
Patents bridged to lung transplantation on VV-ECMO can occasionally be adequately supported with continued VV support during their transplant. Many though require higher flows or increased hemodynamic support with a hybrid configuration. Patients bridged with a jugular dual lumen catheter can be switched to veno-venous-arterial support by adding an arterial cannula. Venous drainage is performed via the bi-caval lumen and oxygenated blood is reinfused into the aorta. Alternately the VV ECMO can be maintained unchanged via the jugular catheter and additional venous and aortic cannulas can be placed as separate circuit for simultaneous VA ECMO. The VV ECMO is maintained at a low flow during the surgery to avoid any thrombotic problem in the circuit and thus can be resume postoperatively after weaning VA ECMO if necessary.
Upon completion of the transplant, ECMO will be weaned for assessment of graft function. While desirable to de-cannulate the patient, the function of the allograft dictates the withdrawal of support. Patients with hypoxemia may be converted to VV, and those with pulmonary hypertension or severe myocardial dysfunction need continued VA ECMO, requiring a later return to the operating room for de-cannulation. Any form of postoperative ECMO has the disadvantage of increased bleeding risk from continued anticoagulation after major surgery. Bridge to recovery with VA ECMO has a higher 30-day mortality than VV ECMO (72).
Weaning ECMO
VA-ECMO
At the end of the surgical procedure, if ECMO support is not planned into the postoperative period, VA-ECMO can be weaned by sequentially dropping the flows on the pump over a period of 10-20 minutes, with the lungs well recruited, suctioned and ventilated at protective tidal volumes. In preparation for this, the anesthesiologist must ensure adequate filling, afterload, and inotropy, and be prepared to react quickly to deterioration. The right heart in particular is at risk of failure, as no cardio-protection is used during ECMO, and coronary perfusion may be threatened by the differential hypoxia phenomenon described above. Pulmonary vascular resistance may be altered by the surgical procedure, and clots can form in the relatively empty heart on ECMO. A thorough TEE evaluation prior to and during weaning ECMO, monitoring right ventricular size and function in real time as flows are reduced, should be considered. Once flows are reduced to around 1 L/min, the ECMO pump is stopped altogether and the arterial line clamped. Hypotension may occur requiring volume infusion and/or inotropes. If the patient is stabilized and the arterial blood gases are consistently adequate, the patient may be de-cannulated.
VV-ECMO
Weaning VV-ECMO takes place with full flows running, and the sweep gas speed and FiO2 slowly decreased. This gradually reduces the diffusion gradient of oxygen and carbon dioxide across the oxygenator membrane to zero, allowing the lungs to assume full gas exchange. As blood flows are maintained, this procedure can be executed very gradually if necessary, with time for serial arterial blood gases, bronchoscopy and pulmonary toilet, lung recruitment manoeuvres and trials of increasing PEEP to optimize gas exchange. If blood gases are adequate on low sweep flows, the pump can be stopped and de-cannulation can take place.
Complications of ECLS
Technical complications from ECLS can be serious and should be minimized by careful evaluation and monitoring. Complications are inherent to the need for vascular cannulation and the anticoagulation required for ECLS use (73-75). The overall risk of complications has decreased over the past few years and will continue to improve with increasing experience. Intra-operative ECMO carries less risk than CPB. Among the various complications that can occur on ECMO, neurological complications and complications related to the cannulation site are of particular importance as they are frequent and potentially preventable.
Complications related to cannulation include the risk of bleeding, damage to the vessels and air emboli. These complications are more frequent with peripheral arterial cannulation due to the small vessel size. Peripheral arterial cannulation can also be associated with limb ischemia, particularly in patients that have a short stature (76). The size of the artery should be estimated by ultrasound if possible, and a suitable cannula size should be chosen. The need for distal limb perfusion depends of the length of ECMO requirement and the size of the vessels. In our experience, we routinely use distal limb cannula to exclude any risk of ischemia in patients requiring peripheral VA ECMO for more than a few hours. Percutaneous technique can be used for femoral cannulation but can occasionally be difficult and lead to multiple puncture sites (77).
Fatal air embolism has been associated with performance of tracheostomy while on high flow VV ECMO with drainage via a bi-caval dual lumen jugular catheter (78). Inadvertent breach of the neck veins enabled the negative pressure in the SVC to aspirate air into the ECMO circuit. Suggested measures for avoiding this complication include temporary reduction of ECMO flows, performance of tracheotomy with the patient in a head down position, and coverage of the puncture sites with wet compresses. The risk of air embolism by a similar mechanism could occur during placement of upper body central venous lines.
The risks associated with long term use of ECMO are multiple and depend to some degree of the underlying comorbidities of the patients. As such they are more difficult to prevent. Complications include infection (79), renal failure (80), hemolysis and coagulation disorders (81,82), Heparin Induced Thrombocytopenia (83), or gastro-intestinal bleeding. Neurological complications such as intracranial bleeding, ischemic stroke, brain edema and seizure can occur in 10% to 20% of the patients on ECLS during long term use (84,85). The pathophysiology for brain injury in ECMO patients is not completely elucidated and may differ between VA and VV ECMO. Factors increasing the risk of neurological complications are related to pre-ECMO complications such as hypotension and hypoxemia, reperfusion injury at ECMO implantation, embolic risk and hemostatic disorders related to the cannulas and the use of heparin. Cardiac arrest, renal failure requiring hemofiltration, and hyperbilirubinemia can be associated with increased risks of neurologic injury (84,85). In patients with hypercapnic respiratory failure, a rapid decrease in CO2 level may increase the risk of intracranial bleeding and therefore slow normalization of the PaCO2 should be performed (84). Additionally the rate of gaseous microembolism during ECMO support rivals that of CPB, with intravenous injections being the most common culprit, with potential for postoperative neurological morbidity (86). Better understanding of the risks of neurological complications and anticoagulation strategy will likely decrease the risk of neurological complications in long term use of ECMO in the future.
Planning thoracic surgery procedures with ECLS support
For any patient who requires ECLS, the surgical checklist should include: the planned ECLS configuration, cannulation sites, timing of cannulation (before or after induction of general anesthesia) and anticipated timing of weaning and de-cannulation. Patient position and planned incision will influence cannulation sites (5). If patients are transferred to the operating room already on ECMO any required modification of support or additional cannulation should be discussed. This allows the anesthesiologist to optimize intravenous and arterial access for monitoring and volume infusion.
There is a wide variety of cannula design, length and diameter. Hence, catheters should be chosen with the type of ECLS support required, the flows required and the size of the destination vessel (87). Central cannulation typically allows placement of larger cannulae and consequently higher flows than peripheral ECMO. Central ECLS cannulae are necessarily placed under general anesthesia. Peripheral cannulation for surgical application is also most frequently performed after the induction of general anesthesia in order to minimize patient movement, and optimize patient comfort and sterile technique. The exceptional circumstances where peripheral ECMO is initiated in the awake patient are clinical scenarios where life threatening respiratory or cardiovascular compromise is anticipated if general anesthesia is initiated without ongoing ECLS support. These include near complete central airway obstruction, presence of a large anterior mediastinal mass, and critical right or left heart failure. The challenge of placement of these peripheral (usually femoral) catheters can not be underestimated. Patients are frequently distressed, and have positional dyspnea that prevents them from lying flat. Catheter placement in a semi-sitting position is not only difficult but increases the risk of vessel injury. Generous local anesthesia and judicious sedation may be helpful, with the goal of maintaining spontaneous ventilation until ECLS is established. In the authors’ experience, a vaso-vagal response to awake femoral cannulation can provoke cardiopulmonary arrest, so cannulation should only be done in a fully monitored setting with resuscitative drugs and equipment immediately available.
Once ECLS is established the efficiency of the resulting gas exchange is such that many patients require little or no pulmonary ventilation. Tidal volume and respiratory rates can be reduced far below what is normally feasible. A lung-protective ventilation with decreased respiratory rates, low tidal volumes and maintenance of PEEP is rational, particularly if the lungs have sustained an injury (88,89). Atelectotrauma is prevented by with 5–10 mmHg of PEEP, and alveolar pO2 should be maintained in order to oxygenate remaining pulmonary blood flow. Exceptionally open airway surgery may require complete apnea for prolonged periods.
Monitoring of patients on ECMO has recently been expertly reviewed, with particular emphasis on the importance of echocardiography for cannula positioning (8). Arterial lines are best placed in the right arm to measure pressure and PaO2 downstream from the right brachiocephalic artery, which correlates most closely with conditions in the right carotid artery and coronary arteries. Similarly, peripheral oxygen saturation probes should be placed intermittently on each hand, to monitor for differential hypoxia. Central venous line location is dictated by cannula location and the surgical incision, but care should be taken not to advance the tip of the catheter too far into the central circulation, so that it is not aspirated into the lumen of the ECMO cannula. Once the ECMO is started central venous pressure readings may not be reliable. PA catheters may be difficult to insert if upper body ECMO cannulae are already in place, both in terms of passing the catheter through the occupied SVC, and in floating into the right heart with ongoing drainage into the ECMO circuit. There is potential for the PA catheter balloon to be aspirated into and occlude drainage cannulae. Consideration should be given to cerebral saturation monitoring with near-infrared spectroscopy, as an indicator of cerebral hypoxia (8,90). In a short retrospective case series using this monitor, Wong et al. found a 100% rate of cerebral desaturation on initiation of ECMO, 80% of which were reversible with changes in hemodynamic management (90).
Anti-coagulation strategy and monitoring should be adapted to the planned procedure. Patients on ECLS long-term can develop a complex coagulopathy which can include low platelet function and numbers, fibrinogen deficiency, loss of vitamin K-dependent clotting factors and acquired Von Willebrand’s disease (91). The Extracorporeal Life Support Organisation (ELSO) has made recommendations for effective anticoagulation during ECLS applications as well as the management of patient bleeding and circuit clotting. These guidelines are available on the ESLO website. Intraoperative use of ECLS for a period of hours likely has a much lower risk of thrombotic complications. Heparin -coated circuits can reduce the heparin requirement substantially for the first six hours of its use. Similarly, patients undergoing thoracic procedures with major blood loss will also develop a deficiency of platelets, fibrinogen and other clotting factors, which will prolong coagulation in the absence of heparin. There are multiple reports of surgical interventions with high bleeding risk using ECLS without heparin (19,30,32,36,37). In our institution, we routinely target an ACT of 160–180 s intraoperatively. Thrombo-elastography, specifically ROTEM™, and platelet function assay are used as adjuncts to ACT to detect causes of bleeding such as factor deficiency, platelet dysfunction or fibrinolysis in ECLS patients who are bleeding intraoperatively, particularly when pre-operative ECLS was required, for example those patients who were bridged to transplant. The role of point of care coagulation monitoring during ECLS is actively being explored (92).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Khoshbin E, Roberts N, Harvey C, et al. Poly-methyl pentene oxygenators have improved gas exchange capability and reduced transfusion requirements in adult extracorporeal oxygenation. ASAIO J 2005;51:281-7. [Crossref] [PubMed]
- Fischer S, Simon AR, Welte T, et al. Bridge to lung transplantation with the novel pumpless interventional lung assist device NovaLung. J Thorac Cardiovasc Surg 2006;131:719-23. [Crossref] [PubMed]
- Dalton HJ. Extracorporeal life support: moving at the speed of light. Respiratory care 2011;56:1445-53. [Crossref] [PubMed]
- Peek GJ, Mugford M, Tiruvoipati R, et al. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. Lancet 2009;374:1351-63. [Crossref] [PubMed]
- Machuca TN, Cypel M, Keshavjee S. Cardiopulmonary Bypass and Extracorporeal Life Support for Emergent Intraoperative Thoracic Situations. Thorac Surg Clin 2015;25:325-34. [Crossref] [PubMed]
- Flörchinger B, Philipp A, Klose A, et al. Pumpless extracorporeal lung assist: a 10 year institutional experience. Ann Thorac Surg 2008;86:410-7. [Crossref] [PubMed]
- Esper SA, Levy JH, Waters JH, et al. Extracorporeal membrane oxygenation in the adult: a review of anticoagulation monitoring and transfusion. Anesth Analg 2014;118:731-43. [Crossref] [PubMed]
- Douflé G, Ferguson ND. Monitoring during extracorporeal membrane oxygenation. Curr Opin Crit Care 2016;22:230-8. [Crossref] [PubMed]
- Gattinoni L, Carlesso E, Langer T. Clinical review: Extracorporeal membrane oxygenation. Crit Care 2011;15:243. [Crossref] [PubMed]
- Formica F, Avalli L, Colagrande L, et al. Extracorporeal membrane oxygenation to support adult patients with cardiac failure: predictive factors of 30-day mortality. Interact Cardiovasc Thorac Surg 2010;10:721-6. [Crossref] [PubMed]
- Zimmermann M, Bein T, Philipp A, et al. Interhospital transportation of patients with severe lung failure on pumpless extracorporeal lung assist. Br J Anaesth 2006;96:63-6. [Crossref] [PubMed]
- Machuca TN, de Perrot M. Mechanical support for the failing right ventricle in patients with precapillary pulmonary hypertension. Circulation 2015;132:526-36. [Crossref] [PubMed]
- de Perrot M, Granton JT, McRae K, et al. Impact of extracorporeal life support on outcome in patients with idiopathic pulmonary arterial hypertension awaiting lung transplantation. J Heart Lung Transplant 2011;30:997-1002. [Crossref] [PubMed]
- Jensen V, Milne B, Salerno T. Femoral-femoral cardiopulmonary bypass prior to induction of anaesthesia in the management of upper airway obstruction. Can Anaesth Soc J 1983;30:270-2. [Crossref] [PubMed]
- Hong Y, Jo KW, Lyu J, et al. Use of venovenous extracorporeal membrane oxygenation in central airway obstruction to facilitate interventions leading to definitive airway security. J Crit Care 2013;28:669-74. [Crossref] [PubMed]
- Ko M, dos Santos PR, Machuca TN, et al. Use of single-cannula venous-venous extracorporeal life support in the management of life-threatening airway obstruction. Ann Thorac Surg 2015;99:e63-5. [Crossref] [PubMed]
- Willms DC, Mendez R, Norman V, et al. Emergency bedside extracorporeal membrane oxygenation for rescue of acute tracheal obstruction. Respir Care 2012;57:646-9. [Crossref] [PubMed]
- Higashi K, Takeshita J, Terasaki H, et al. A case of acute airway obstruction with sharp sawdust particles, successfully treated by extracorporeal lung assist. Kokyu To Junkan 1989;37:329-33. [PubMed]
- Park JM, Kim CW, Cho HM, et al. Induced airway obstruction under extracorporeal membrane oxygenation during treatment of life-threatening massive hemoptysis due to severe blunt chest trauma. J Thorac Dis 2014;6:E255-8. [PubMed]
- Smith IJ, Sidebotham DA, McGeorge AD, et al. Use of extracorporeal membrane oxygenation during resection of tracheal papillomatosis. Anesthesiology 2009;110:427-9. [PubMed]
- Fung R, Stellios J, Bannon PG, et al. Elective use of veno-venous extracorporeal membrane oxygenation and high-flow nasal oxygen for resection of subtotal malignant distal airway obstruction. Anaesth Intensive Care 2017;45:88-91. [PubMed]
- Natt B, Knepler J Jr, Kazui T, et al. The Use of Extracorporeal Membrane Oxygenation in the Bronchoscopic Management of Critical Upper Airway Obstruction. J Bronchology Interv Pulmonol 2017;24:e12-4. [Crossref] [PubMed]
- Park AH, Tunkel DE, Park E, et al. Management of complicated airway foreign body aspiration using extracorporeal membrane oxygenation (ECMO). Int J Pediatr Otorhinolaryngol 2014;78:2319-21. [Crossref] [PubMed]
- Lang G, Ghanim B, Hotzenecker K, et al. Extracorporeal membrane oxygenation support for complex tracheo-bronchial procedures. Eur J Cardiothorac Surg 2015;47:250-5. [Crossref] [PubMed]
- Johnson AP, Cavarocchi NC, Hirose H. Ventilator strategies for VV ECMO management with concomitant tracheal injury and H1N1 influenza. Heart Lung Vessel 2015;7:74-80. [Crossref] [PubMed]
- Kim CW, Kim DH, Son BS, et al. The Feasibility of Extracorporeal Membrane Oxygenation in the Variant Airway Problems. Ann Thorac Cardiovasc Surg 2015;21:517-22. [Crossref] [PubMed]
- Keeyapaj W, Alfirevic A. Carinal resection using an airway exchange catheter-assisted venovenous ECMO technique. Can J Anaesth 2012;59:1075-6. [Crossref] [PubMed]
- Redwan B, Ziegeler S, Freermann S, et al. Intraoperative veno-venous extracorporeal lung support in thoracic surgery: a single-centre experience. Interact Cardiovasc Thorac Surg 2015;21:766-72. [PubMed]
- Walles T, Steger V, Wurst H, et al. Pumpless extracorporeal gas exchange aiding central airway surgery. J Thorac Cardiovasc Surg 2008;136:1372-4. [Crossref] [PubMed]
- Wiebe K, Poeling J, Arlt M, et al. Thoracic surgical procedures supported by a pumpless interventional lung assist. Ann Thorac Surg 2010;89:1782-7. [Crossref] [PubMed]
- Hoetzenecker K, Klepetko W, Keshavjee S, et al. Extracorporeal support in airway surgery. J Thorac Dis 2017;9:2108-17. [Crossref] [PubMed]
- Gillon SA, Toufektzian L, Harrison-Phipps K, et al. Perioperative extracorporeal membrane oxygenation to facilitate lung resection after contralateral pneumonectomy. Ann Thorac Surg 2016;101:e71-3. [Crossref] [PubMed]
- Oey IF, Peek GJ, Firmin RK, et al. Post-pneumonectomy video-assisted thoracoscopic bullectomy using extra-corporeal membrane oxygenation. Eur J Cardiothorac Surg 2001;20:874-6. [Crossref] [PubMed]
- Schiff JH, Koninger J, Teschner J, et al. Veno-venous extracorporeal membrane oxygenation (ECMO) support during anaesthesia for oesophagectomy. Anaesthesia 2013;68:527-30. [Crossref] [PubMed]
- Slinger P, Suissa S, Adam J, et al. Predicting arterial oxygenation during one-lung ventilation with continuous positive airway pressure to the nonventilated lung. J Cardiothorac Anesth 1990;4:436-40. [Crossref] [PubMed]
- Brenner M, O'Connor JV, Scalea TM. Use of ECMO for resection of post-traumatic ruptured lung abscess with empyema. Ann Thorac Surg 2010;90:2039-41. [Crossref] [PubMed]
- Bressman M, Raad W, Levsky JM, et al. Surgical therapy for complications of pneumonia on extracorporeal membrane oxygenation can improve the ability to wean patients from support. Heart Lung Vessel 2015;7:330-1. [PubMed]
- Redwan B, Biancosino C, Giebel F, et al. Perioperative single-site veno-venous extracorporeal CO2 removal for minimally invasive giant bulla resection. Perfusion 2017;32:698-701. [Crossref] [PubMed]
- Tsunezuka Y, Sato H, Tsubota M, et al. Significance of percutaneous cardiopulmonary bypass support for volume reduction surgery with severe hypercapnia. Artif Organs 2000;24:70-3. [Crossref] [PubMed]
- Li X, He H, Sun B. Veno-venous extracorporeal membrane oxygenation support during lung volume reduction surgery for a severe respiratory failure patient with emphysema. J Thorac Dis 2016;8:E240-3. [Crossref] [PubMed]
- Redwan B, Ziegeler S, Semik M, et al. Single-site cannulation venovenous extracorporeal CO2 removal as bridge to lung volume reduction surgery in end-stage lung emphysema. ASAIO J 2016;62:743-6. [Crossref] [PubMed]
- Kim JD, Ko ES, Kim JY, et al. Anesthesia under cardiopulmonary bypass for video assisted thoracoscopic wedge resection in patient with spontaneous pneumothorax and contralateral post-tuberculosis destroyed lung. Korean J Anesthesiol 2013;65:174-6. [Crossref] [PubMed]
- Krecmerova M, Mosna F, Bicek V, et al. Extracorporeal membrane oxygenation to support repeated whole-lung lavage in a patient with pulmonary alveolar proteinosis in life threatening dyspnoe--a case report. BMC Anesthesiol 2015;15:173. [Crossref] [PubMed]
- Cohen ES, Elpern E, Silver MR. Pulmonary alveolar proteinosis causing severe hypoxemic respiratory failure treated with sequential whole-lung lavage utilizing venovenous extracorporeal membrane oxygenation: a case report and review. Chest 2001;120:1024-6. [Crossref] [PubMed]
- Asai T. Emergency cardiopulmonary bypass in a patient with a mediastinal mass. Anaesthesia 2007;62:859-60. [Crossref] [PubMed]
- Tempe DK, Arya R, Dubey S, et al. Mediastinal mass resection: Femorofemoral cardiopulmonary bypass before induction of anesthesia in the management of airway obstruction. J Cardiothorac Vasc Anesth 2001;15:233-6. [Crossref] [PubMed]
- Wickiser JE, Thompson M, Leavey PJ, et al. Extracorporeal membrane oxygenation (ECMO) initiation without intubation in two children with mediastinal malignancy. Pediatr Blood Cancer 2007;49:751-4. [Crossref] [PubMed]
- Felten ML, Michel-Cherqui M, Puyo P, et al. Extracorporeal membrane oxygenation use for mediastinal tumor resection. Ann Thorac Surg 2010;89:1012. [Crossref] [PubMed]
- de Perrot M, Fadel E, Mussot S, et al. Resection of locally advanced (T4) non-small cell lung cancer with cardiopulmonary bypass. Ann Thorac Surg 2005;79:1691-6. [Crossref] [PubMed]
- Langer NB, Mercier O, Fabre D, et al. Outcomes after resection of T4 non-small cell lung cancer using cardiopulmonary bypass. Ann Thorac Surg 2016;102:902-10. [Crossref] [PubMed]
- Shimizu J, Ikeda C, Arano Y, et al. Advanced lung cancer invading the left atrium, treated with pneumonectomy combined with left atrium resection under cardiopulmonary bypass. Ann Thorac Cardiovasc Surg 2010;16:286-90. [PubMed]
- Lang G, Taghavi S, Aigner C, et al. Extracorporeal membrane oxygenation support for resection of locally advanced thoracic tumors. Ann Thorac Surg 2011;92:264-70. [Crossref] [PubMed]
- Byrne JG, Leacche M, Adnithotri AK, et al. The use of cardiopulmonary bypass during resection of locally advanced thoracic malignancies. Chest 2004;125:1581-6. [Crossref] [PubMed]
- Kobayashi S, Sawabata N, Araki O, et al. Dissection of a mediastinal mature teratoma requires replacement of the ascending aorta during cardiopulmonary bypass. J Thorac Cardiovasc Surg 2007;134:1371-2. [Crossref] [PubMed]
- Agathos EA, Lachanas E, Karagkiouzis G, et al. Cardiopulmonary bypass assisted resection of mediastinal masses. J Card Surg 2012;27:338-41. [Crossref] [PubMed]
- Mei J, Pu Q, Zhu Y, et al. Reconstruction of the pulmonary trunk via cardiopulmonary bypass in extended resection of locally advanced lung malignancies. J Surg Oncol 2012;106:311-5. [Crossref] [PubMed]
- Abrams D, Agerstrand CL, Biscotti M, et al. Extracorporeal membrane oxygenation in the management of diffuse alveolar hemorrhage. Asaio J 2015;61:216-8. [Crossref] [PubMed]
- Patel JJ, Lipchik RJ. Systemic lupus-induced diffuse alveolar hemorrhage treated with extracorporeal membrane oxygenation: a case report and review of the literature. J Intensive Care Med 2014;29:104-9. [Crossref] [PubMed]
- Abbas AE. Traumatic injury of the pulmonary artery: Transection, rupture, pseudoaneurysm, or dissection? Sometimes semantics do matter. J Thorac Cardiovasc Surg 2016;152:1437-8. [Crossref] [PubMed]
- Jeng EI, Piovesana G, Taylor J, et al. Extracorporeal membrane oxygenation to facilitate tracheal healing after oesophagogastric catastrophe. Eur J Cardiothorac Surg 2018;53:288-289. [Crossref] [PubMed]
- Weinberg A, Tapson VF, Ramzy D. Massive Pulmonary Embolism: Extracorporeal Membrane Oxygenation and Surgical Pulmonary Embolectomy. Semin Respir Crit Care Med 2017;38:66-72. [Crossref] [PubMed]
- Lebreton G, Bouabdallaoui N, Gauduchon L, et al. Successful use of ECMO as a bridge to surgical embolectomy in life-threatening pulmonary embolism. Am J Emerg Med 2015;33:1332.e3-4. [Crossref] [PubMed]
- Kawahito K, Murata S, Ino T, Fuse K. Angioscopic pulmonary embolectomy and ECMO. Ann Thorac Surg 1998;66:982-3. [PubMed]
- Berman M, Tsui S, Vuylsteke A, et al. Successful extracorporeal membrane oxygenation support after pulmonary thromboendarterectomy. Ann Thorac Surg 2008;86:1261-7. [Crossref] [PubMed]
- Chacón-Alves S, Perez-Vela JL, Grau-Carmona T, et al. Veno-arterial ECMO for rescue of severe airway hemorrhage with rigid bronchoscopy after pulmonary artery thromboendarterectomy. Int J Artif Organs 2016;39:242-4. [Crossref] [PubMed]
- Kuroda H, Masuda Y, Imaizumi H, et al. Successful extracorporeal membranous oxygenation for a patient with life-threatening transfusion-related acute lung injury. J Anesth 2009;23:424-6. [Crossref] [PubMed]
- Lee AJ, Koyyalamudi PL, Martinez-Ruiz R. Severe transfusion-related acute lung injury managed with extracorporeal membrane oxygenation (ECMO) in an obstetric patient. J Clin Anesth 2008;20:549-52. [Crossref] [PubMed]
- Swol J, Cannon JW, Napolitano LM. ECMO in trauma: What are the outcomes? J Trauma Acute Care Surg 2017;82:819-20. [Crossref] [PubMed]
- Jacobs JV, Hooft NM, Robinson BR, et al. The use of extracorporeal membrane oxygenation in blunt thoracic trauma: A study of the Extracorporeal Life Support Organization database. J Trauma Acute Care Surg 2015;79:1049-53. [Crossref] [PubMed]
- Hoetzenecker K, Donahoe L, Yeung JC, et al. Extracorporeal life support as a bridge to lung transplantation-experience of a high volume transplant center. J Thorac Cardiovasc Surg 2018;155:1316-28. [Crossref] [PubMed]
- Machuca TN, Collaud S, Mercier O, et al. Outcomes of intraoperative extracorporeal membrane oxygenation versus cardiopulmonary bypass for lung transplantation. J Thorac Cardiovasc Surg 2015;149:1152-7. [Crossref] [PubMed]
- Squiers JJ, Lima B, DiMaio JM. Contemporary extracorporeal membrane oxygenation therapy in adults: Fundamental principles and systematic review of the evidence. J Thorac Cardiovasc Surg 2016;152:20-32. [Crossref] [PubMed]
- Kreyer S, Muders T, Theuerkauf N, et al. Hemorrhage under veno-venous extracorporeal membrane oxygenation in acute respiratory distress syndrome patients: a retrospective data analysis. J Thorac Dis 2017;9:5017-29. [Crossref] [PubMed]
- Geyer M, Gohrbandt B, Sagoschen I, et al. Pitfalls of cannulation for extracorporeal life support: review of the literature and illustrative case presentation. J Artif Organs 2018;21:8-16. [Crossref] [PubMed]
- Reeb J, Olland A, Renaud S, et al. Vascular access for extracorporeal life support: tips and tricks. J Thorac Dis 2016;8:S353-63. [Crossref] [PubMed]
- Park BW, Lee SR, Lee MH, et al. Short stature is associated with the development of lower limb ischaemia during extracorporeal life support. Perfusion 2018. [Epub ahead of print]. [Crossref] [PubMed]
- Rupprecht L, Lunz D, Philipp A, et al. Pitfalls in percutaneous ECMO cannulation. Heart Lung Vessel 2015;7:320-6. [PubMed]
- Lother A, Wengenmayer T, Benk C, et al. Fatal air embolism as complication of percutaneous dilatational tracheostomy on venovenous extracorporeal membrane oxygenation, two case reports. J Cardiothorac Surg 2016;11:102. [Crossref] [PubMed]
- Biffi S, Di Bella S, Scaravilli V, et al. Infections during extracorporeal membrane oxygenation: epidemiology, risk factors, pathogenesis and prevention. Int J Antimicrob Agents 2017;50:9-16. [Crossref] [PubMed]
- Kilburn DJ, Shekar K, Fraser JF. The Complex relationship of extracorporeal membrane oxygenation and acute kidney injury: causation or association? Biomed Res Int 2016;2016:1094296. [PubMed]
- Sy E, Sklar MC, Lequier L, et al. Anticoagulation practices and the prevalence of major bleeding, thromboembolic events, and mortality in venoarterial extracorporeal membrane oxygenation (VA-ECMO): A systematic review and meta-analysis. J Crit Care 2017;39:87-96. [Crossref] [PubMed]
- Reed RC, Rutledge JC. Laboratory and clinical predictors of thrombosis and hemorrhage in 29 pediatric extracorporeal membrane oxygenation nonsurvivors. Pediatr Dev Pathol 2010;13:385-92. [Crossref] [PubMed]
- Pollak U, Yacobobich J, Tamary H, et al. Heparin-induced thrombocytopenia and extracorporeal membrane oxygenation: a case report and review of the literature. J Extra Corpor Technol 2011;43:5-12. [PubMed]
- Luyt CE, Bréchot N, Demondion P, et al. Brain injury during venovenous extracorporeal membrane oxygenation. Intensive Care Med 2016;42:897-907. [Crossref] [PubMed]
- Lorusso R, Gelsomino S, Parise O, et al. Neurologic injury in adults supported with veno-venous extracorporeal membrane oxygenation for respiratory failure: findings from the extracorporeal life support organization database. Crit Care Med 2017;45:1389-97. [Crossref] [PubMed]
- Jiao Y, Gipson KE, Bonde P, et al. Quantification of postmembrane gaseous microembolization during venoarterial extracorporeal membrane oxygenation. ASAIO J 2018;64:31-7. [PubMed]
- Pavlushkov E, Berman M, Valchanov K. Cannulation techniques for extracorporeal life support. Ann Transl Med 2017;5:70. [Crossref] [PubMed]
- Slinger P, Kilpatrick B. Perioperative lung protection strategies in cardiothoracic anesthesia: are they useful? Anesthesiol Clin 2012;30:607-28. [Crossref] [PubMed]
- Schmidt M, Pellegrino V, Combes A, et al. Mechanical ventilation during extracorporeal membrane oxygenation. Crit Care 2014;18:203. [Crossref] [PubMed]
- Wong JK, Smith TN, Pitcher HT, et al. Cerebral and lower limb near-infrared spectroscopy in adults on extracorporeal membrane oxygenation. Artif Organs 2012;36:659-67. [Crossref] [PubMed]
- Raiten JM, Wong ZZ, Spelde A, et al. Anticoagulation and Transfusion Therapy in Patients Requiring Extracorporeal Membrane Oxygenation. J Cardiothorac Vasc Anesth 2017;31:1051-9. [Crossref] [PubMed]
- Bolliger D, Zenklusen U, Tanaka KA. Point-of-care coagulation management algorithms during ECMO support: are we there yet? Minerva Anestesiol 2016;82:1000-9. [PubMed]


