The feasibility and safety of off-pump coronary bypass surgery in emergency revascularization
Introduction
As surgeon proficiency has increased and devices have improved over the past few decades, off-pump coronary artery bypass grafting (OPCAB) has evolved as a widely acceptable procedure (1,2). Recently, OPCAB has expanded its indication to high-risk patients with multiple comorbidities such as old age, renal failure, poor lung function, and impaired left ventricular function, and outcomes are better than those following on-pump bypass surgery (3-7). OPCAB is also useful in patients requiring emergent intervention, purportedly by avoiding the inflammatory reactions and ischemic injury associated with cardiopulmonary bypass (CPB) (8-11). However, OPCAB use in patients with critical preoperative conditions remains debatable because heart manipulation and displacement might result in compromised hemodynamics and cardiac decompensation. The feasibility and safety of OPCAB in patients meeting indications for emergency surgery was therefore assessed in this review of a 10-year single-center experience.
Methods
Patients
Of the 2,825 patients who underwent isolated OPCAB at our institution from January 2003 to April 2015, 113 (4%) underwent an emergency OPCAB according to the following indications: cardiogenic shock with complex anatomy not suitable for percutaneous coronary intervention (PCI) (41, 36.3%); ongoing ischemia despite optimal pharmacotherapy in patients with primary CABG indication (36, 31.8%); PCI complication requiring emergency operation (18, 15.9%); ongoing ischemia despite successful or failed PCI (7, 6.2%); and others, such as left main dissection or plaque rupture (11, 9.7%). The emergency of the procedure was defined and graded according to the European Multicenter Study on Coronary Artery Bypass Grafting (E-CABG) severity classification (class 1: 39, 34.5%; class 2: 43, 38.1%; class 3: 27, 23.9%; class 4: 4, 3.5%) (12). Indication and urgency class are summarized in Table 1. Operations were performed by two surgeons with longstanding experience in OPCAB. To analyze changes in trends of emergency OPCAB over time, the patients were divided into early (<2010) and late (≥2010) period cohorts.

Full table
Surgical procedure
The operation was performed under general endotracheal anesthesia with continuous Swan-Ganz catheter monitoring, transesophageal echocardiography, and arterial pressure monitoring. All operations were performed using the off-pump method through a full sternotomy incision. The left internal thoracic artery (LIMA) was used primarily in all patients, and only if necessary the right internal thoracic artery, radial artery, and saphenous vein were used. The internal thoracic artery was harvested using a semi-skeletonized method and very low voltage unipolar electrocautery. The radial artery was harvested from the non-dominant forearm using a pedicled method and a Harmonic scalpel (Ethicon Endosurgery, Cincinnati, OH, USA). Heparin with papaverine was used to avoid vasospasm of the internal thoracic artery and a calcium channel blocker (diltiazem) was used to prevent spasm of the radial artery during the operation. Heparin was administered at a dose of 100 units/kg to achieve a target activated clotting time of at least 300 seconds during the operation. A deep pericardial traction suture was placed using 1-0 Dexon sutures. Purse-string sutures for cannulation were placed in the aorta and right atrium in preparation for conversion to on-pump as a standby measure. In cases of unstable hemodynamics, LIMA to left anterior descending (LAD) grafting was performed before other heart procedures (such as pericardial traction suture and heart and aortic manipulation). An Octopus tissue stabilizer (Medtronic, Minneapolis, MN, USA) was used for cardiac stabilization during anastomosis construction. In cases of LAD anastomosis, an intracoronary shunt was mainly used, and for anastomosis of other left coronary artery systems the proximal snaring technique with a silicone elastomer was used. For right coronary artery (RCA) anastomosis, an intracoronary shunt was usually used for the main RCA, and the proximal snaring technique was used for the posterior descending or posterolateral artery. To remove blood from the sites of arteriotomy, a mixed carbon dioxide blower and irrigation with warm saline were used. When aortic manipulation was needed, side-bite clamping was used until 2008, and the clampless Heartstring system (Maquet Cardiovascular, San Jose, CA, USA) was used thereafter. All anastomoses were constructed using continuous running 7-0 or 8-0 monofilament sutures.
End points and definitions
The primary end points of this study were in-hospital mortality and late all-cause mortality. The secondary end points were perioperative morbidity and late major adverse cerebral and cardiovascular events (MACCE). Perioperative morbidities included: low cardiac output syndrome, perioperative myocardial infarction (MI), neurologic complication, prolonged mechanical ventilation, pulmonary complication, renal failure, and reoperation for bleeding. Prolonged mechanical ventilation was defined as ventilator therapy administered for more than 7 days. Postoperative renal failure was defined as requirement of continuous veno-venous hemofiltration. MACCE were defined as death from any cause, nonfatal MI, reintervention, or stroke. MI was defined as occurrence of wall motion abnormality or CK-MB elevation with appearance of new Q waves or ST segment elevation of more than 2 mm on electrocardiogram. Reintervention was defined as PCI after surgery or redo coronary bypass surgery irrespective of clinical symptomatology. Complete revascularization was defined as a number of distal anastomoses exceeding the number of diseased coronary segments or systems.
Data collection
Preoperative and perioperative data were collected prospectively from the cardiac research databases at our institution. Follow-up data were obtained from reviewing hospital charts, conducting telephone interviews, and searching the National Death Index. Our study was conducted following approval by the Institutional Review Board of Yonsei University College of Medicine (No. 4-2015-0461). Individual patient consent was waived because of the retrospective nature of the study.
Statistical analyses
Statistical analyses were performed with SPSS for Windows, version 18.0 (SPSS Inc., Chicago, IL, USA). All continuous data are expressed as mean ± standard deviation (SD) and categorical variables are expressed as number and/or frequency. For comparison of characteristics between two groups, continuous variables were compared using the t-test and categorical variables were compared using the χ2 or Fisher’s exact tests. Goodness of fit was assessed by using the Hosmer and Lemeshow χ2 test. Overall survival and freedom from MACCE during 10-year follow up were calculated using Kaplan-Meier methods. Survival curves were compared by the log-lank test. Logistic regression and the Cox proportional hazards method were used to identify independent predictors of early and late outcomes. Variables with a P value <0.05 by univariate analysis were included in the regression model as multinomial variables. Statistical significance was defined as a two-tailed P value of <0.05.
Results
Patient demographics
Preoperative demographics and risk factors are listed in Table 2. The mean age of the population was 67.2±9.0 years. Cardiogenic shock was present in 35% of patients. Ten percent of patients had acute pulmonary congestion requiring preoperative ventilation, and most patients undergoing emergency OPCAB (80.4%) were classified as New York Heart Association class III or IV. The mean logistic EuroSCORE was 14.3±13.5. The late period cohort had a larger percentage of patients with old age, dyslipidemia, chronic renal failure, cardiogenic shock, and intra-aortic balloon pump (IABP) status.
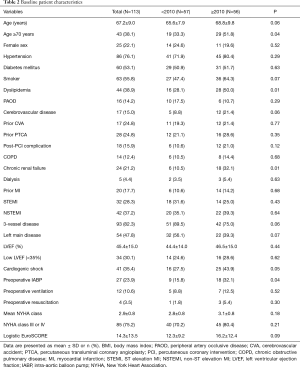
Full table
Operative data
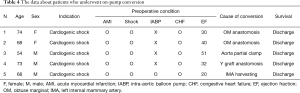
The operative data are listed in Table 3. The mean interval between diagnosis and emergency surgery was 4.20±2.01 hours. The mean number of distal anastomoses was 3.0±0.7. Complete revascularization was achieved in 79.6% of patients. LIMA graft was used in all patients except two who needed revascularization in only the RCA territory. The mean operative time was 245.1 minutes. The late period cohort had more distal anastomoses per patient (3.2±0.7 vs. 2.8±0.8, P<0.01) and a larger percentage of patients with complete revascularization (87.5% vs. 71.9%, P=0.04). There were 5 (4.4%) conversions to on-pump in patients who had profound shock or arrest during the operation, and four of these were in the early period cohort. Data about these on-pump conversion cases are summarized in Table 4.
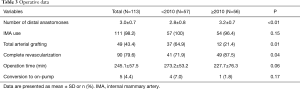
Full table
Full table
Early operative results
Six patients (5.3%) died during the hospital stay period: two from heart failure, three from pulmonary complications, and one from ventricular fibrillation. The other major postoperative complications observed after emergency OPCAB are summarized in Table 5. Reoperation for excessive bleeding was performed in only one patient (0.9%). Three patients required extracorporeal membrane oxygenation during the postoperative period, and all survived. Ten (8.8%) patients experienced pulmonary complications, and 7 (70%) of those needed tracheostomies. Length of intensive care unit (ICU) stay (4.7±6.1 days) and length of hospital stay (14.9±9.6 days) were acceptable. The late period cohort had a smaller percentage of patients with mortality, stroke, perioperative MI, renal failure, pulmonary complication, transfusion, and wound complication, but none of these differences reached statistical significance. The late period cohort had a significantly shorter duration of ICU stay (5.7±8.0 vs. 3.8±2.8, P=0.05) and hospital stay (17.3±12.1 vs. 12.8±6.0, P=0.02). In multivariate analysis, COPD [odds ratio, 30.2 (95% CI: 1.79–509.48); P=0.02] and preoperative cardiogenic shock [4.16 (1.21–8.64); P=0.01] were independent predictors of operative death.
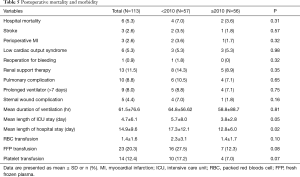
Full table
Long-term survival
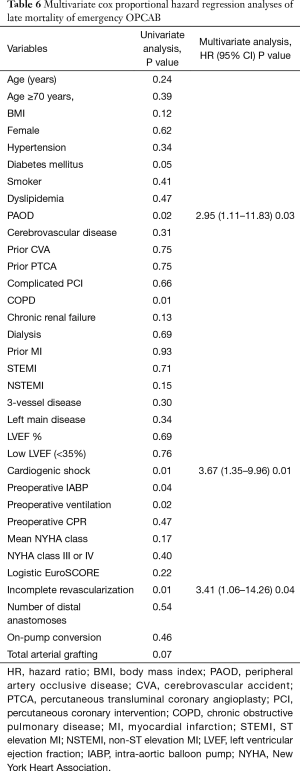
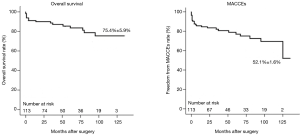
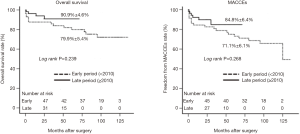
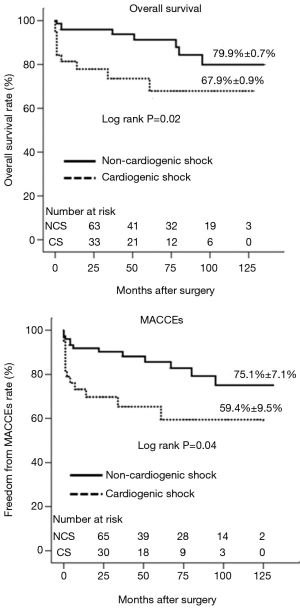
The mean follow-up duration was 51.1±40.3 (range, 1–135) months. The completion rate of follow up was 94.6% (107/113). Survival rate at 1, 5, and 10 years was 91.0%, 85.4%, and 75.4%, respectively. Rate of freedom from MACCEs at 1, 5, and 10 years was 85.6%, 78.9%, and 52.1%, respectively (Figure 1). The late period cohort showed a higher rate of survival (90.9% vs. 79.9%) and freedom from MACCEs (84.8% vs. 71.1%) at 5 years compared to the early period cohort (Figure 2). Peripheral arterial occlusive disease (PAOD), incomplete revascularization, and cardiogenic shock were independent predictors of late mortality. Among these risk factors, cardiogenic shock had the strongest association with late mortality [odds ratio, 3.67 (95% CI: 1.35–9.96); P=0.01; Table 6]. At 10 years, the overall survival and freedom from MACCEs rates were 67.7% and 59.4%, respectively, for patients with preoperative cardiogenic shock compared to 79.9% and 75.1%, respectively, for patients without cardiogenic shock (Figure 3).
Full table
Discussion
Although the applicability off-pump technique in coronary artery bypass surgery has expanded to high-risk patients, OPCAB has not traditionally been considered an option for emergent interventions. Several retrospective studies reported the promising potential of emergency OPCAB, but these were relatively small studies (8-11), and it remained unclear whether OPCAB could be successfully applied in patients requiring emergency coronary bypass surgery. Since 2003, two experienced surgeons at our institution have performed OPCAB in emergency situations; the present study reviewed more than 100 such experiences to analyze the feasibility and safety of this technique.
The benefit of OPCAB in patients requiring emergency revascularization
Numerous studies have already indicated that the off-pump technique is associated with favorable outcomes by avoiding CPB and its associated inflammatory response in coronary bypass surgery (13-15). However, the benefits of OPCAB in emergency situations have been less well defined. Kerendi et al. evaluated 44 patients who underwent emergency OPCAB compared to 570 patients who underwent on-pump CABG and reported the benefits of emergency OPCAB in terms of postoperative morbidity and mortality (9). Likewise, Martinez and colleagues analyzed a series of 68 patients who underwent emergency OPCAB and documented reduced pulmonary complication and ventilator time for emergency OPCAB relative to on-pump CABG (11). These studies emphasize that in emergency situations, use of the off-pump technique can, by avoiding the adverse effects of CPB, be more beneficial than elective surgery. Because most patients who underwent emergency surgery had multi-organ damage and systemic inflammation, the impact of adverse effects of CPB would be higher for emergency surgery than for elective surgery. Our current study also showed benefits of the off-pump technique on postoperative outcomes, with very low rates of in-hospital mortality (6.2%), operative stroke (2.7%), and reoperation for bleeding (0.9%); rates of other complications (e.g., renal failure, prolonged ventilation, wound infection) and length of ICU stay (4.77±6.59 days) and hospital stay (14.98±9.66 days) were also acceptable, despite the emergency nature of the cases. The late period cohort, despite including more high-risk patients, had improved early and late outcomes compared with the early period cohort. Our study showed that the benefits of OPCAB in emergency situations can be substantial if properly used.
Overcoming the disadvantages of off-pump technique in emergency surgery
One of the major concerns regarding emergency OPCAB is how to achieve complete revascularization in situations of unstable hemodynamics. Many studies have found that it is difficult to achieve complete revascularization in OPCAB, especially in emergency situations, and this leads to worse late outcomes (16-18). When OPCAB began being used in emergency situations, many studies reported that the mean number of distal anastomoses of emergency OPCAB was 2–2.5 and the rate of complete revascularization was less than 60% (8-11). These results supported a limited applicability of emergency OPCAB. However, recent studies suggest that complete revascularization can be achieved even in an emergency by experienced surgeons (3,9,19). Puskas and colleagues showed that as surgeons gained more experience with OPCAB, complete revascularization was achieved with rates comparable to on-pump CABG (2). They recommend that a surgeon should attempt emergency cases only after performing 200 elective OPCAB procedures (9). Our study was consistent with these findings. Our mean number of distal anastomoses was 3.04±0.87 and complete revascularization could be achieved in 82.3% patients. Long-term survival and freedom from MACCEs rates were also acceptable (77.0%±0.6% and 52.0%±1.6% at 10 years after surgery). Notably, our investigation showed that the late period patients had more distal anastomoses (2.8±0.8 vs. 3.2±0.7, P<0.01) and a higher rate of complete revascularization (71.9% vs. 87.5%, P=0.04) compared to the early period cohort. These procedures were performed by two surgeons who each had performed more than 1000 elective OPCAB procedures before they began to perform emergency OPCAB. Since 2000, 99% of isolated CABG has been performed off pump at our institution. The accumulation of our surgeons’ and anesthesiologists’ experience with the OPCAB procedure and the resulting improvements in complete revascularization may explain why the outcomes of procedures performed after 2010 were better than the earlier cases, despite the increase in high-risk patients in the late period cohort. Our study supports that emergency OPCAB can achieve complete revascularization if performed by a very experienced surgeon.
A second major concern regarding emergency OPCAB is how to overcome hemodynamic instability. In the current study, more than a third of patients experienced preoperative cardiogenic shock and about half required support with IABP or extracorporeal membrane oxygenation (ECMO). To overcome hemodynamic instability, our operative strategy is to perform LAD grafting first, before other heart procedures such as pericardial traction suture or manipulation of the heart and aorta. After successful achievement of LIMA to LAD grafting, hemodynamics improved in almost all cases, thereby providing a more stable background for other procedures. We also remained prepared for the sudden application of CPB by keeping the CPB machine on standby. Although on-pump conversion was needed in five patients (4.4%), all quickly received CPB support and survived. In addition, anesthesiological management is very important for successful emergency OPCAB. TEE and pulmonary artery catheter measurements were routinely used to assess hemodynamic compromise. Hemodynamic stabilization was controlled by fluid resuscitation, catecholamine administration, Trendelenburg positioning, and atrial or ventricle pacing. When this conservative management failed, intraoperative placement of an IABP or ECMO was considered for re-stabilization. Our institution has cardiac-specific anesthesiologists with experience in over 1,000 elective OPCAB cases. This collaboration between cardiac anesthesiologists and experienced surgeons may contribute to greater safety of OPCAB in emergency situations.
Selection of indications for the off-pump technique
It is important to properly select patients for use of the off-pump technique in emergency situations. At our institution, the off-pump technique has been performed in 80% of isolated emergency coronary artery bypass cases since 2004, and in over 90% of cases in the last 5 years. However, as noted by Kerendi et al., use of emergency OPCAB cannot be generalized to all complex cases (9). In the current study, five patients (4.4%) underwent on-pump conversion during OPCAB. All of these patients had complex conditions combining severe cardiogenic shock and congestive heart failure with pulmonary edema and desaturation, which precluded maintenance of vital signs within an acceptable range until LIMA to LAD grafting. Our analysis showed that only one of the patients who underwent on-pump conversion had IABP support. This finding indicates that IABP support may be a protective factor to reduce the risks of on-pump conversion. With the exception of patients who absolutely require cardiopulmonary support, emergency OPCAB therefore appears safe and effective in most cases.
Risk factors for late mortality after emergency OPCAB
Our study showed that PAOD, incomplete revascularization, and cardiogenic shock were independent risk factors for late mortality after emergency OPCAB, with cardiogenic shock the most powerful risk factor. Interestingly, cardiogenic shock can be associated with late mortality as well as perioperative outcomes. Rastan et al. mentioned that cardiogenic shock status was associated with significantly worse late mortality after emergency revascularization (20). They indicated that cardiogenic shock was an independent risk factor for late survival regardless of operation method (beating heart or cardioplegic arrest). Our study showed findings consistent with theirs. We found that cardiogenic shock could increase the chance of postoperative morbidities such as pulmonary and neurologic complications and renal failure, as well as operative mortality, which finally led to greater late mortality.
Limitations
Several limitations of the current study are acknowledged. First, this was an observational study with retrospective review. We cannot definitively exclude selection bias, because OPCAB is usually performed in patients with more stable hemodynamic compared to on-pump CABG. However, we performed OPCAB in most emergency patients, and therefore minimized this selection bias. Furthermore, this study does not compare clinical outcomes with those of on-pump CABG. Therefore, we cannot establish the superiority of OPCAB to the on-pump CABG strategy in emergency cases. Finally, this study included a relatively small sample size. However, given the current lack of randomized trials in this patient population, this study is valuable in that it is one of the largest reported series of emergency OPCAB procedures.
Conclusions
In conclusion, the present study suggests that emergency OPCAB can be performed safely and effectively with favorable in-hospital outcomes. With achievement of complete revascularization, long-term outcomes are also acceptable. The OPCAB strategy can therefore be considered a good option in patients who are indicated for emergency surgery.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Our study was conducted following approval by the Institutional Review Board of Yonsei University College of Medicine (No. 4-2015-0461). Individual patient consent was waived because of the retrospective nature of the study.
References
- Society of Thoracic Surgeons Adult Cardiac Surgery Database. Available online: www.sts.org. (accessed June 1, 2015).
- Puskas JD, Williams WH, Duke PG, et al. Off-pump coronary artery bypass grafting provides complete revascularization with reduced myocardial injury, transfusion requirements, and length of stay: a prospective randomized comparison of two hundred unselected patients undergoing off-pump versus conventional coronary artery bypass grafting. J Thorac Cardiovasc Surg 2003;125:797-808. [Crossref] [PubMed]
- Boyd WD, Desai ND, Del Rizzo DF, et al. Off-pump surgery decreases postoperative complications and resource utilization in the elderly. Ann Thorac Surg 1999;68:1490-3. [Crossref] [PubMed]
- Chamberlain MH, Ascione R, Reeves BC, et al. Evaluation of the effectiveness of off-pump coronary artery bypass grafting in high-risk patients: an observational study. Ann Thorac Surg 2002;73:1866-73. [Crossref] [PubMed]
- Magee MJ, Dewey TM, Acuff T, et al. Influence of diabetes on mortality and morbidity: off-pump coronary artery bypass grafting versus coronary artery bypass grafting with cardiopulmonary bypass. Ann Thorac Surg 2001;72:776-80. [Crossref] [PubMed]
- Darwazah AK, Abu Sham'a RA, Hussein E, et al. Myocardial revascularization in patients with low ejection fraction < or =35%: effect of pump technique on early morbidity and mortality. J Card Surg 2006;21:22-7. [Crossref] [PubMed]
- Al-Ruzzeh S, Nakamura K, Athanasiou T, et al. Does off-pump coronary artery bypass (OPCAB) surgery improve the outcome in high-risk patients?: a comparative study of 1398 high-risk patients. Eur J Cardiothorac Surg 2003;23:50-5. [Crossref] [PubMed]
- Ochi M, Hatori N, Saji Y, et al. Application of off-pump coronary artery bypass grafting for patients with acute coronary syndrome requiring emergency surgery. Ann Thorac Cardiovasc Surg 2003;9:29-35. [PubMed]
- Kerendi F, Puskas JD, Craver JM, et al. Emergency coronary artery bypass grafting can be performed safely without cardiopulmonary bypass in selected patients. Ann Thorac Surg 2005;79:801-6. [Crossref] [PubMed]
- Darwazah AK, Sham'a RA, Isleem I, et al. Off-pump coronary artery bypass for emergency myocardial revascularization. Asian Cardiovasc Thorac Ann 2009;17:133-8. [Crossref] [PubMed]
- Martinez EC, Emmert MY, Thomas GN, et al. Off-pump coronary artery bypass is a safe option in patients presenting as emergency. Ann Acad Med Singapore 2010;39:607-12. [PubMed]
- Biancari F, Ruggieri VG, Perrotti A, et al. European Multicenter Study on Coronary Artery Bypass Grafting (E-CABG registry): Study Protocol for a Prospective Clinical Registry and Proposal of Classification of Postoperative Complications. J Cardiothorac Surg 2015;10:90. [Crossref] [PubMed]
- Wan S, Izzat MB, Lee TW, et al. Avoiding cardiopulmonary bypass in multivessel CABG reduces cytokine response and myocardial injury. Ann Thorac Surg 1999;68:52-6. [Crossref] [PubMed]
- Ascione R, Lloyd CT, Underwood MJ, et al. Inflammatory response after coronary revascularization with or without cardiopulmonary bypass. Ann Thorac Surg 2000;69:1198-204. [Crossref] [PubMed]
- Wan IY, Arifi AA, Wan S, et al. Beating heart revascularization with or without cardiopulmonary bypass: evaluation of inflammatory response in a prospective randomized study. J Thorac Cardiovasc Surg 2004;127:1624-31. [Crossref] [PubMed]
- Locker C, Shapira I, Paz Y, et al. Emergency myocardial revascularization for acute myocardial infarction: survival benefits of avoiding cardiopulmonary bypass. Eur J Cardiothorac Surg 2000;17:234-8. [Crossref] [PubMed]
- Lattouf OM, Puskas JD, Thourani VH, et al. Does the number of grafts influence surgeon choice and patient benefit of off-pump over conventional on-pump coronary artery revascularization in multivessel coronary artery disease? Ann Thorac Surg 2007;84:1485-94. [Crossref] [PubMed]
- Lattouf OM, Thourani VH, Kilgo PD, et al. Influence of on-pump versus off-pump techniques and completeness of revascularization on long-term survival after coronary artery bypass. Ann Thorac Surg 2008;86:797-805. [Crossref] [PubMed]
- Song HK, Petersen RJ, Sharoni E, et al. Safe evolution towards routine off-pump coronary artery bypass: negotiating the learning curve. Eur J Cardiothorac Surg 2003;24:947-52. [Crossref] [PubMed]
- Rastan AJ, Eckenstein JI, Hentschel B, et al. Emergency coronary artery bypass graft surgery for acute coronary syndrome: beating heart versus conventional cardioplegic cardiac arrest strategies. Circulation 2006;114:I477-85. [Crossref] [PubMed]


