Endostapling the aberrant artery filled with embolized coils for intralobar pulmonary sequestration: a report of two cases
Introduction
Intrapulmonary sequestration is a rare congenital bronchopulmonary malformation. Surgery is generally standard treatment, and thoracoscopic resection has been accepted recently. It is an important procedural step to cut the aberrant artery safely. Some patients have inflammatory change of the sequestrated lung and adhesion to the adjacent organs, such as the parietal pleura, esophagus, and diaphragm. In those cases, it is difficult to identify the aberrant artery. In thoracoscopic surgery cases, simple stapling using an endostapler has been reported, but many reports described fatal intraoperative hemorrhage because of encircling or stapling failure. Therefore, occlusion of the aberrant artery before the surgery can prevent fatal intraoperative hemorrhage. However, the suitable method to cut the aberrant artery filled with metallic coil is controversial.
We describe two cases of intrapulmonary sequestration in which endostapling of the aberrant artery with coils was used to prevent intraoperative hemorrhage and to easily identify the aberrant artery.
Case presentation
Case 1
A 28-year-old man was admitted to our hospital for right back pain and fever. Although the family physician treated the patient with antibiotics, his symptoms reoccurred for a few months. The chest computed tomography (CT) scan revealed consolidation and fluid collection in the right lower lobe (Figure 1A). The aberrant artery originated from the celiac trunk, measured approximately 10 mm in diameter and 75 mm in length, and returned to the right inferior pulmonary vein (Figure 1B). We diagnosed him as having intralobar pulmonary sequestration. After the systemic inflammatory reaction disappeared, we decided to perform coil embolization before the surgery to prevent intraoperative bleeding from the aberrant artery.
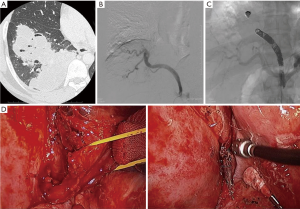
Radiologists performed angiography and coil embolization (Figure 1C). They placed a 4-French (Fr) long sheath in the right femoral artery. A microcatheter (Prowler Select Plus, Johnson and Johnson, Tokyo, Japan) was positioned in the aberrant artery as the branch of the celiac trunk. The most distal side was embolized with a fibered pushable coil as an anchor and six Tornado coils (Cook, Inc., Tokyo, Japan) measuring 8 mm × 9.5 mm. Subsequently, they placed one fibered 14 mm × 30 cm Interlocking Detachable Coil (IDC) (Boston Scientific, Tokyo, Japan), three 12 mm × 30 cm IDCs, three 8 mm × 9.5 cm Tornado coils, and one 7 mm × 9 cm Tornado coil in the middle part of the aberrant artery; and one 14 mm × 30 cm IDC and one 8 mm × 9.5 cm Tornado coil 6 cm in the proximal side of the aberrant artery. Finally, they placed one 10 mm × 30 cm IDC and eight 7 mm × 9 cm Tornado coils in the most proximal side at the diaphragm level.
On the next day, we performed video-assisted thoracoscopic right lower lobectomy with access incisions plus four port sites. The right lower lobe with sequestered lung was expanded and hardened with adhesion to the parietal pleura, esophagus, and diaphragm. The aberrant artery was identified on the inferior edge of the pulmonary ligament measuring 12 mm in diameter. We stapled the aberrant artery with coils using an endostapler (Powered-Echelon 45 white, Ethicon, Tokyo, Japan) after the stay sutures were placed (Figure 1D). Some coil fragments exposed the stump of the aberrant artery, and there was no bleeding. Afterward, a standard thoracoscopic right lower lobectomy was performed. The patient was discharged 7 days postoperatively.
The CT scan 6 months postoperatively revealed the coil-embolized aberrant artery.
Case 2
A 51-year-old woman was admitted to our hospital for recurrent episodes of fever, productive cough, and hemoptysis. The CT scan revealed consolidation with multiple cystic components, fluid collection, and bronchiectasis in the right posterior basal segment of the lower lobe (Figure 2A). The aberrant artery originated from the right inferior phrenic artery (Figure 2B). We diagnosed her as having intralobar pulmonary sequestration. We decided to perform coil embolization before the surgery to prevent hemoptysis and intraoperative bleeding from the aberrant artery.
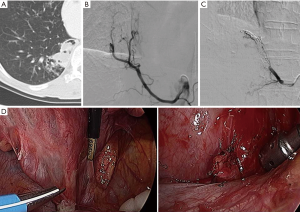
Radiologists performed coil embolization before the surgery (Figure 2C). They placed a 4-Fr long sheath in the right common femoral artery. The aberrant artery was embolized with 23 Tornado coils (Cook, Inc.) (five coils measuring 4 mm × 2 mm, five measuring 6 mm × 2 mm, and six measuring 6 mm × 2 mm) between the most distal side on the right lower lobe level and the most proximal side at the diaphragm level.
On the next day, we performed video-assisted thoracoscopic right lower lobectomy with access incisions plus four port sites. The right lower lobe with the sequestered lung was not expanded or hardened and did not adhere to the parietal pleura, esophagus, or diaphragm. The aberrant artery was identified on the inferior edge of the pulmonary ligament. We stapled the aberrant artery with coils using an endostapler (Powered-Echelon 45 white, Ethicon) after clamping the proximal side (Figure 2D). The stapling process was uneventful. Afterward, a standard thoracoscopic right lower lobectomy was performed. The patient was discharged 7 days postoperatively.
The CT scan 6 months postoperatively revealed the coil-embolized aberrant artery.
Discussion
Pulmonary sequestration is a rare congenital bronchopulmonary malformation. The incidence in an adult population was reported as 0.15–6.4% or less than 0.03% (1). Although symptomatic patients have recurrent pulmonary infection, hemoptysis, and chest pain, 28% of patients are asymptomatic (1). A chest radiograph can show the cystic solid mass and parenchymal infiltration (1,2). In some cases, the pseudo-tumor shadow can be observed with no pathologic sign (2). An enhanced CT scan can reveal the cystic solid mass and aberrant artery (2). However, the preoperative diagnostic rate is not high at approximately 12.5–68% (1,2). Some patients have undergone pulmonary resection for another diagnosis and were diagnosed as having sequestration intraoperatively.
Surgery is generally accepted treatment for pulmonary sequestration. Pulmonary resection and occlusion and cutting the aberrant artery are standard procedures (3). Lobectomy is most often chosen, but some selected patients undergo segmentectomy and wedge resection (3). Thoracoscopic surgery has been reported recently (4,5). Recent studies comparing thoracoscopic surgery and open thoracotomy reported that neither procedure was associated with surgical mortality or a significant difference in the overall morbidity rate of 11.1–23.5% (6,7). Although thoracoscopic surgery may be feasible because the conversion rate to open thoracotomy was low (approximately 7%) (4,5), the main reason for conversion was accidental intraoperative hemorrhage from the aberrant artery. Although average intraoperative blood loss was not significantly different between both approaches, less bleeding occurred during thoracoscopic surgery (117–241 mL), and the rate of misidentification of the aberrant artery was 16.7% in thoracoscopic surgery (6,7). Aberrant arteries are identified in the pulmonary ligament, and those arteries are associated with several conditions, complications, and variations. The aberrant artery can have plural vessels and be complicated by an aneurysm, shunt to the pulmonary artery, and a fistula to the bronchus. Aberrant arteries are hidden in the inflamed, scarred tissue and adhere to the adjacent organs, such as the pleura, esophagus, and diaphragm. Therefore, safe encircling and cutting are important procedures of pulmonary sequestration surgery, especially thoracoscopic surgery. Some studies have reported cases of intraoperative massive bleeding due to injury of the aberrant artery (4,6). To prevent intraoperative bleeding and to control preoperative hemoptysis, preoperative embolization was useful in our cases.
Appropriate timing of surgery after embolization is also controversial. In a case of embolization to control hemoptysis, the symptom disappeared the next day, and surgery was performed 1 month after embolization (8). In another case, surgery was performed immediately after embolization (9). Our purpose of embolization is to prevent intraoperative hemorrhage during thoracoscopic resection. We were able to identify the aberrant artery in the pulmonary ligament when we pressed it with a cotton swab as a hard tubular structure without pulsation. We were also able to cut the aberrant artery with coils using an endostapler. Fragments of the coil appeared from the stump of artery, and there were no bleeding or stapling failure. We placed stay sutures in case 1 and a proximal clamp in case 2 before stapling, but we think that these preparatory steps were not necessary.
A previous study described a large artery more than 20 mm in diameter and an aneurysmal artery. Because we have no experience using this method for an artery more than 12 mm, we could not assess the usefulness and safety of this method for such arteries.
Embolic materials vary—metallic coils and gelatin sponges are popular. Use of a vascular plug is a simple method to occlude the most proximal side (10). The advantage of coil embolization is that it can create an embolus at a long distance away from the aberrant artery with a short blind end postoperatively. That may reduce the risk of postoperative aneurysm or hemothorax. The disadvantages are that many coils are needed to occlude the entire length of the artery and the cost is expansive. The number of coils used in our cases was minimal, and the long-term outcome is unknown. In cases of systemic arterial supply to the basal segments of the lower lobe without sequestration, therapeutic transarterial embolization without lung resection can be an alternative treatment option (11,12); however, there is no report about the same therapy in the case of sequestration.
Endostapling with coils for the aberrant artery in pulmonary sequestration is a simple and safe technique of thoracoscopic resection. The coil-embolized artery can be identified easily as a hard tubular structure in the inflamed, scarred pulmonary ligament. The long embolization and short cecum of the artery may prevent postoperative vascular complication.
Acknowledgements
Funding: This work was supported by JSPS KAKENHI grant number 25462171.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patients for publication of this manuscript and any accompanying images.
References
- Polaczek M, Baranska I, Szolkowska M, et al. Clinical presentation and characteristics of 25 adult cases of pulmonary sequestration. J Thorac Dis 2017;9:762-7. [Crossref] [PubMed]
- Gezer S, Taştepe I, Sirmali M, et al. Pulmonary sequestration: a single-institutional series composed of 27 cases. J Thorac Cardiovasc Surg 2007;133:955-9. [Crossref] [PubMed]
- Berna P, Cazes A, Bagan P, et al. Intralobar sequestration in adult patients. Interact Cardiovasc Thorac Surg 2011;12:970-2. [Crossref] [PubMed]
- Kestenholz PB, Schneiter D, Hillinger S, et al. Thoracoscopic treatment of pulmonary sequestration. Eur J Cardiothorac Surg 2006;29:815-8. [Crossref] [PubMed]
- Liu C, Pu Q, Ma L, et al. Video-assisted thoracic surgery for pulmonary sequestration compared with posterolateral thoracotomy. J Thorac Cardiovasc Surg 2013;146:557-61. [Crossref] [PubMed]
- Liu HS, Li SQ, Qin YZ, et al. Surgical treatment of intralobar pulmonary sequestration. Chin Med Sci J 2010;25:53-6. [Crossref] [PubMed]
- Li Q, Xie D, Sihoe A, et al. Video-assisted thoracic surgery is associated with better short-term outcomes than open thoracotomy in adult patients with intralobar pulmonary sequestration. Interact Cardiovasc Thorac Surg 2018;26:284-7. [Crossref] [PubMed]
- Avsenik J, Štupnik T, Popoviča P. Endovascular embolization prior to surgical resection of symptomatic intralobar pulmonary sequestration in an adult. Eur J Radiol Open 2015;3:12-5. [Crossref] [PubMed]
- Goto T, Toya K, Wakaki M, et al. Resection of intralobar pulmonary sequestration after coil embolization of aberrant arteries: report of a case. Surg Today 2013;43:923-5. [Crossref] [PubMed]
- Shibano T, Endo S, Tetsuka K, et al. Aberrant aneurysm of adult-type pulmonary sequestration: report of a case. J Thorac Dis 2015;7:E33-6. [PubMed]
- Abe T, Mori K, Shiigai M, et al. Systemic arterial supply to the normal basal segments of the left lower lobe of the lung--treatment by coil embolization--and a literature review. Cardiovasc Intervent Radiol 2011;34 Suppl 2:S117-21. [Crossref] [PubMed]
- Saida T, Ninomiya H, Hojo F, et al. Systemic arterial supply to the normal basal segments of the left lower lobe treated by coil embolization, with long-term follow-up. Radiat Med 2006;24:365-8. [Crossref] [PubMed]


