Uniportal video-assisted thoracoscopic surgery (VATS) lobectomy with en bloc lymphadenectomy for a large central type carcinoma at right upper lobe
Introduction
Uniportal video-assisted thoracic surgery (VATS) lobectomy has been still in evolution and facing many challenging issues, especially for a large central type tumor. In the past, patients with a tumor larger than 5 cm in diameter were considered as contraindication for VATS. However, the progress of VATS techniques has overcome this limitation (1,2). To confirm the radical manner of the lobectomy, preoperative study of the computed tomography (CT) images is vital to the whole process of the surgical procedure. Meanwhile, utilization of a cranial-caudal single-direction fissureless technique with closer camera view of the targeted structures can often lessen the difficulty of the procedure.
Surgical technique
A 59-year-old man had a persistent cough for 6 weeks. A 7 cm × 6 cm × 6 cm tumor in diameter at the right upper lobe was identified on enhanced chest CT (Figure 1). Preoperative bronchoscopy detected the neoplasm at the orifice to the anterior segmental bronchus of the right upper lobe. The biopsy revealed as adenocarcinoma. Preoperative imaging studies confirmed the clinical diagnosis as lung cancer and defined the disease as stage IIb–IIIa (T3N0–1M0). Neoadjuvant therapy prior to radical treatment is recommended by our multidisciplinary team. However, the patient denied this form of treatment and urged for surgery. It was considered operable according to the pulmonary reserve testing and cardiac work up.
General anesthesia with a double-lumen endotracheal intubation was performed before surgery. The patient was placed at the left lateral position. Only one incision, about 4-cm long, was made at the 4th intercostal space in the mid-axillary line. A lap-protector was then placed at the incision. The surgical procedure was facilitated by aligning the 30° angled view of the camera with the general direction of the dissection. Combined utilization of sharp, blunt or cautery-based instruments, the division and ligation methods of the lobar structures was similar to that during three-portal VATS. For example, bronchial arteries must be cauterized or clipped; lobar structures can be ligated with stapler, suture, as well as hemolocks. In our experience, utilization of a cranial-caudal single-direction fissureless technique with closer camera view of the targeted structures can often lessen the difficulty of the procedure during the uniportal VATS upper lobectomy (Figure 2).

The intraoperative exploration was first carried out under camera view. A large tumor was clearly identified and located at the right upper lobe. The visceral pleura was invaded. The whole surgical procedure was listed as following steps.
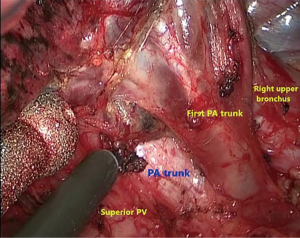
- Pulling the lung caudally, the pleura around the superior, anterior hilum was excised. The first branches of the pulmonary artery (PA) to apical and anterior segment were exposed first, and then the upper bronchus and superior pulmonary vein (PV). Lymph nodes at station 10R were removed, and then station 3R. In this part, the energy instruments should be carefully used to avoid the injury of the phrenic nerve (Figure 3);
- The procedure continued with dissection and ligation of the first branches of the PA with a vascular stapler. Clearance of the space between PA branches and the adjacent lymph nodes was often essential to insert the stapler. Excessive traction of the upper lobe must be avoided when stapling the PA branches;
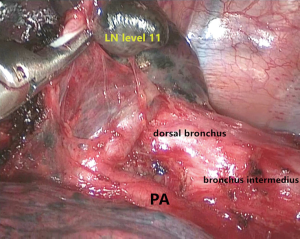
- Continue to divide the upper bronchus, we began the maneuver at the crotch between the upper and middle bronchus. Dividing the lymph nodes in this area will allow the safe isolation of the upper bronchus from the bronchial trunk. Be sure to inflate the lung before stapling the right upper bronchus;
- The lymph nodes along the middle bronchus are removed until visualization of the dorsal bronchus. Small blood vessels including bronchial arteries should be firmly coagulated. Subsequently we continued to remove the soft tissue and any lymph nodes toward a cranial-caudal single-direction (Figure 4). When working on the superior PV, be sure to make enough space surrounding the PV. The surgeon gently made the safe passage of the stapler by retracting the upper lobe forward, which allowed ligation of the PV easily and safely (Figure 5);
- Subsequent dissection along the PA trunk will allow the identification of another artery branch, i.e., the posterior ascending artery. Occasionally, other thin arterial branch might be encountered during this scenario; after stapling the posterior ascending branch, any lymph nodes adjacent to the fissure should be divided and resected (Figure 6). Then the fissure was completed with staplers, the right upper lobectomy was finished. Specimen removal was achieved with an 8# glove;
- The procedure was followed by lymph node dissection. Station 2R and 4R went first, then the pleura covering lymph nodes at station 2R and 4R was incised. We took all lymph nodes and adjacent tissue with an en bloc manner. Pulling the lung forward, dissection of the station 7 lymph nodes was then followed with the same manner as station 4R. During the lymphadenectomy, the energy instruments should be carefully used to avoid the injury of the pneumogastric nerve;
- After the hemostasis and air leak test, a single chest tube was then placed at the rear-end of the incision.
Postoperative pathology report: invasive adenocarcinoma with pleura invasion, acinar type, lymph nodes at station 4R was found metastatic, whereas station 2R/3R/7/10R/11R had no metastasis.
Discussion
With the progress of uniportal VATS technique, it is now feasible to handle a large central type tumor during VATS lobectomy. In our experience, preoperative study of the CT images is very important for a large tumor (≥5 cm in diameter). The surgeon must be sure that the hilar structures can be isolated safely based on the imaging modalities (4). During surgery, a close camera view can often facilitate the operative procedure. Uniportal upper lobectomy offers a better view in comparison to multi-portal VATS. Meanwhile, we advocate the “fissureless” approach in upper lobectomy, the isolation and ligation of the lobar structures were dissected towards a “cranial to caudal” single direction, dividing the fissure last. This technique can be very useful in the management of the large central type tumor during uniportal upper lobectomy. As showed in this case, stapling the PA branch cranially first, then the upper bronchus or PV, followed by the posterior ascending PA branch, and the fissure is left last to be dissected. The fissureless approach can be more advantageous for patients with fissure problem. A surgeon should also be aware that the flexibility with the multiple operative techniques in performing VATS for patients with larger tumors. The last we want to emphasize the radical resection of the carcinoma. Be sure not to press the tumor when pulling the lung to expose the hilar structures. En bloc resection during lobectomy and lymphadenectomy can offer a precise pathologic staging and decreases the recurrence.
Acknowledgements
Dr. Hongbo Guo was granted the Award of Great Potential in the 2017 VATS Lobectomy & Segmentectomy Video Contest.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Vannucci F, Gonzalez-Rivas D. Is VATS lobectomy standard of care for operable non-small cell lung cancer? Lung Cancer 2016;100:114-9. [Crossref] [PubMed]
- Chen HW, Du M. Video-assisted thoracoscopic pneumonectomy. J Thorac Dis 2015;7:764-6. [PubMed]
- Guo H, Jing W, Chen F, et al. Video-assisted thoracic surgery (VATS) uniportal right upper lobectomy. Asvide 2018;5:648. Available online: http://www.asvide.com/article/view/26157
- Guido Guerrero W, Gonzalez-Rivas D, Hernandez Arenas LA, et al. Techniques and difficulties dealing with hilar and interlobar benign lymphadenopathy in uniportal VATS. J Vis Surg 2016;2:23. [PubMed]





