Current practice in management of exudative pleural effusions—a survey of American Association of Bronchology and Interventional Pulmonology (AABIP)
Introduction
The development of an interventional pulmonary (IP) program with the associated expertise in thoracoscopy and tunneled pleural catheter (TPC) insertion has led to increased management of pleural effusion by pulmonary and to an evolution in practice patterns with respect to pleural disease (1). We postulated that similar shifts have occurred in other institutions with an active IP presence, and sought to understand current beliefs and practice patterns in the IP community with respect to management of exudative pleural effusion and medical thoracoscopy (MT).
Methods
A 26-question survey was created and disseminated to all registered American Association of Bronchology and Interventional Pulmonology (AABIP) members in August, 2017. The questions addressed practitioner demographics, practice types and locations, perceptions with respect to rigid versus Semi-rigid thoracoscopy (also known as flexible or semi-flexible thoracoscope), and the clinical approach to recurrent exudative and malignant effusions. The survey was closed in September, 2017 and the results were tabulated. Some respondents completed only a portion of the survey. For this reason, results are reported as percent of responses to each question and not as absolute numbers, as the absolute numbers don’t contain the relevant denominators. Also, each response was rounded to the nearest percent, and for this reason the summed responses to a question may not always total 100%. The survey also provided avenue for the respondents to elaborate on their response; these were tabulated and included in the results. Student t tests were used when appropriate to compare the responses.
Results
Of the 978 active AABIP members, 388 members accessed the survey out of which 165 responded to the invitation. Eighty-one percent of respondents were from the United States (US), while 19% were from eleven other countries, with largest numbers of non-US responses from Canada and India (see Figure 1A). Geographically within the US, most responders practiced in the mid-west (20%), the southwestern US (20%), or the northeast (16%), with a relative paucity of responses from the southeastern US and the west coast (see Figure 1B).

Eighty-four percent of the respondents were men and 14% women. Seventy-eight percent of respondents were in the 30–49 age range. Only 74% self-identified as “interventional pulmonologist”, but 93% stated that IP was within their scope of practice, the responders also included one advanced nurse practitioner, fellows and two retired alumni. The survey was sent to all members of AABIP; some of these were non-proceduralists. The survey when taken by non-proceduralists was coded to stop when they responded in a negative to the question “did they perform MTs”. Thus, only proceduralists were able to complete the survey. The IPs worked in both academic (56% of respondents) and private practice (26%) settings. Regardless of IP designation, the majority of respondents also worked as general pulmonologists (74%) and/or as intensivists (50%). A majority of respondents (59%) practiced in non-fellowship-affiliated institutions.
Nearly two-thirds (61%) of the respondents personally performed thoracoscopy. For those who did not, the primary reasons were a strong thoracic surgery presence (41% of non-performing respondents) and a lack of training and equipment (10%). The most common reason cited for thoracoscopy was undiagnosed exudative effusion; 93% would perform thoracoscopy for recurrent undiagnosed exudative effusion. Other indications in order of frequency listed were parapneumonic effusion or empyema, recurrent primary spontaneous pneumothorax, secondary spontaneous pneumothorax, chylothorax, and hepatic hydrothorax.
Respondents agreed that a recurrent pleural effusion was one for which more than one thoracentesis was required. Thirty-eight percent would proceed to thoracoscopy for an effusion that recurred after a single thoracentesis led to a diagnosis of undiagnosed exudate, while 52% would wait for a second non-diagnostic thoracentesis. With respect to pleurodesis, most (93%) would perform a pleurodesis if the effusion recurred within 8 weeks, with over half advocating for pleurodesis for an effusion that recurred within a month.
Several questions addressed Semi-rigid thoracoscopy. Of those respondents who did perform thoracoscopy, 27% performed only rigid thoracoscopy, 29% performed only semi-rigid thoracoscopy (P=0.84), and 44% performed both procedures (P=0.17). There were no statistically significant differences. When asked what procedure was preferred for evaluation of a recurrent exudative effusion, 51% preferred Semi-rigid thoracoscopy with 41% in favor of rigid thoracoscopy. Other choices were image-guided needle biopsy of pleura (6%) and CT surgery referral (1%). Respondents were split on whether yield was higher with rigid than with Semi-rigid thoracoscopy, with 41% believing that rigid produced a higher yield, 29% believing that it didn’t (P=0.02) this difference was statistically significant and the remainder of the respondents were noncommittal. A majority of respondents felt that rigid thoracoscopy did not cause more pain and did not leave a larger scar than Semi-rigid thoracoscopy. However, this didn’t seem to have made a difference in the practice of respondents who reported an ability to perform both rigid and semi-rigid MT. They were just as likely to use either of the two techniques for the diagnosis of exudative pleural effusion (P=0.65).
Semi-rigid thoracoscopy is performed more frequently in the endoscopy suite (47%) than in the operating room (39%), with 14% of operators using either. A majority of operators used moderate sedation for Semi-rigid thoracoscopy, with the following breakdown: local anesthesia only 9%, moderate sedation with local anesthesia 54%, monitored anesthesia care (MAC) 26%, general anesthesia with intubation 9%, and general anesthesia with double-lumen intubation 4%. The majority (64%) of respondents who perform semi-rigid thoracoscopy do not perform cryobiopsies, only one respondent who performed rigid thoracoscopy reported interest in cryobiopsies (P<0.0001). Thirty-eight percent feel that cryobiopsies increase biopsy yield compared to a Semi-rigid thoracoscope, with a majority noncommittal on this issue.
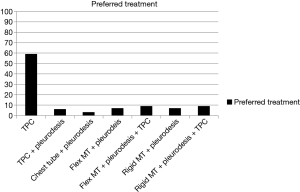
The questionnaire addressed the use of tunneled pleural catheters. As noted earlier, 93% of respondents favored thoracoscopy for the diagnosis of undiagnosed recurrent pleural effusion. When pleural effusions were already felt to be diagnosed (malignant or non-malignant), indwelling pleural catheters became the treatment modality of choice for a large number of respondents. For recurrent non-malignant effusion, 41% would place a TPC (with or without pleurodesis agent), while 51% would favor a thoracoscopic approach with pleurodesis (mechanical or chemical). The remaining 8% would opt for routine chest tube with chemical pleurodesis. TPCs would be placed post-operatively by 51% of respondents who would opt for thoracoscopy as the initial approach to recurrent benign effusion. When asked about a recurrent pleural effusion known to be of malignant etiology, TPC became the most favored primary treatment; 65% chose TPC with or without pleurodesis agent, while 32% favored a pleuroscopic approach with mechanical or chemical pleurodesis (P<0.001) and 6% favored insertion of a standard chest tube and chemical pleurodesis (Figure 2). For those who would opt for thoracoscopy as the initial approach to recurrent malignant effusion, however, 55% would place a TPC post-operatively.
Discussion
Thoracoscopy is a valuable tool in the diagnosis and management of pleural effusion, and the emergence of IP as a subspecialty has abetted a resurgence of “medical thoracoscopy”. Our goal was to survey AABIP membership to better understand the current state of practice and understanding of thoracoscopy in the IP community.
In our opinion, the most striking finding is the fact that only 61% of respondents to this query of an IP community perform thoracoscopy, with the two most common reasons (I) resistance from thoracic surgery within the respondent’s institution; and (II) lack of training. The latter should be a factor of decreasing impact, as current criteria for training in IP through the fellowship process include thoracoscopy. The former is more problematic; the ideal IP program works in partnership with subspecialties including thoracic surgery, head and neck surgery, radiation oncology, and thoracic oncology. Political/financial barriers imposed by other subspecialties are unfortunate, as they impair both the relationship with that subspecialty and the capacity of IP physicians to practice the full range of accredited competence.
Thirty-eight percent would proceed to thoracoscopy after a first thoracentesis with a cytologically negative exudative effusion, while 52% would do so after a second thoracentesis. One could fault the survey question, as whether or not most IPs would proceed to thoracoscopy after a single negative thoracentesis would probably depend upon clinical suspicion for malignancy, and the simplified question did not include any clinical context. In addition, pragmatic aspects of scheduling thoracoscopy may impact clinical decisions. The morbidity of thoracoscopy is very low (<0.01%) (2,3), and the authors support the argument that thoracoscopy is a reasonable second procedure because of (I) its dramatically higher diagnostic yield (than a second thoracentesis) both for cancer and for other diagnoses such as tuberculous pleurisy; and (II) the opportunity to initiate pleurodesis when indicated.
The semirigid thoracoscope is an instrument developed specifically by interventional pulmonologists and, to our knowledge, used exclusively by interventional pulmonologists. It arose out of familiarity with the bronchoscope and the thought that pulmonologists could transition to thoracoscopy more easily and at less expense than they could transition to rigid thoracoscopy in the operating room (4,5) (some of the reasoning appears to be spurious; the equipment for rigid thoracoscopy is generally available in all operating rooms and thus incurs no additional expense. On the other hand, if semi-rigid thoracoscopy is performed in the endoscopy suite, the overall cost of the procedure is reduced). Biopsies with the Semi-rigid thoracoscope tend to be smaller than those with rigid, with cryoprobe partially bridging the gap between biopsies with rigid instruments and those obtained with Semi-rigid biopsy forceps (6,7). Diagnostic yield with Semi-rigid thoracoscopy has been shown to be similar (6) and inferior (7) to those obtained with rigid tools. The survey demonstrates that over two-thirds of respondents who perform thoracoscopy use a Semi-rigid scope some or all of the time, and there is a slight preference for Semi-rigid thoracoscopy in our community even though with respect to yield more feel that rigid has a higher yield. There is an emerging interest in cryobiopsies, but mostly in respondents who mostly used Semi-rigid thoracoscopy as their primary tool.
Finally, the survey demonstrates a large impact of TPCs upon the management of pleural effusion. Once it has been determined that a recurrent effusion is definitely malignant, TPC (with or without pleurodesis agent) would be the intervention of choice for 65% of respondents, and 55% of those who chose to start with thoracoscopy would leave a TPC in place at the end of the procedure. For recurrent effusion known to be benign, only 41% favored TPC as the intervention of choice. Fifty-one percent would perform thoracoscopy, but a majority (51%) of those performing thoracoscopy would place a TPC at the end of the procedure. Thus in the IP community TPCs play a major role in the treatment of recurrent exudative effusions of all etiologies.
We acknowledge that a 28-question survey cannot yield more than a broad picture of attitudes and practice patterns, and that subtleties of opinion and practice have surely been missed. The incomplete surveys may also have impacted our results but the direction of skew is unknown. Also, as noted above, there are factors such as patient condition and scheduling availability that impact upon management decisions, and these realities can play an important role in decision trees for individual patients. We hope that despite these shortcomings this survey gives some insight into the state of practice in the IP community.
Conclusions
Thoracoscopy is widely but not universally performed in the IP community. The most problematic barriers appear to be competition from thoracic surgeons. Thoracoscopy is seen almost universally as an important tool in the diagnosis and management of recurrent exudative effusion. New graduates may need to be cognizant of the potential reception by the thoracic surgeons at the site of their first IP employment. TPC is increasingly the mainstay of management of recurrent exudative effusion, and current practice patterns indicate a widespread integration of thoracoscopy with TPC in management strategies.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by IRB with IRB No. 205543, and AABIP research committee. Answering the survey was considered to be consent to be included in the study. Patients were not involved in the study.
References
- Raman T, Meena N. A single institution experience for the management of recurrent pleural effusions with tunneled pleural catheter and its evolution. Ther Adv Respir Dis 2017;11:343-52. [Crossref] [PubMed]
- Loddenkemper R. Thoracoscopy--state of the art. Eur Respir J 1998;11:213-21. [Crossref] [PubMed]
- Rodriguez-Panadero F, Janssen JP, Astoul P. Thoracoscopy: general overview and place in the diagnosis and management of pleural effusion. Eur Respir J 2006;28:409-22. [Crossref] [PubMed]
- McLean AN, Bicknell SR, McAlpine LG, et al. Investigation of pleural effusion: an evaluation of the new Olympus LTF semiflexible thoracofiberscope and comparison with Abram's needle biopsy. Chest 1998;114:150-3. [Crossref] [PubMed]
- Ernst A, Hersh CP, Herth F, et al. A novel instrument for the evaluation of the pleural space: an experience in 34 patients. Chest 2002;122:1530-4. [Crossref] [PubMed]
- Rozman A, Camlek L, Marc-Malovrh M, et al. Rigid versus semi-rigid thoracoscopy for the diagnosis of pleural disease: a randomized pilot study. Respirology 2013;18:704-10. [Crossref] [PubMed]
- Wurps H, Schönfeld N, Bauer TT, et al. Intra-patient comparison of parietal pleural biopsies by rigid forceps, flexible forceps and cryoprobe obtained during medical thoracoscopy: a prospective series of 80 cases with pleural effusion. BMC Pulm Med 2016;16:98. [Crossref] [PubMed]


