Hecheng Li: sticks with the spirit of craftsmanship
Only with high skills, diligence and benevolence can a doctor be wholeheartedly devoted to relieving patients from sufferings. At most time, he is in wards, at operating rooms, or in workshops. Over the past decades, he has been promoted from residence doctor, attending doctor, to chief physician by keeping improving professionalism and upholding the spirit of craftsmanship. This doctor is Professor Hecheng Li, a committed surgeon at the Thoracic Surgery Department of Ruijin Hospital.
—What is your faith as a doctor?
—Prof. Li paused for a while and answered, “Do not forget why you started, and every effort will be paid off when you look back”.
Expert's introduction
Hecheng Li (Figure 1), director of Thoracic Surgery Department of Ruijin Hospital, chief physician, and doctoral supervisor.
Since 1996, he has been engaged in the diagnosis and treatment of thoracic tumors including lung cancer, esophageal cancer, cardiac cancer, and mediastinal tumors. In 2004, supported by the International Anti-Cancer Alliance, he was trained on the multidisciplinary treatment of pleural mesothelioma at the Vanderbilt-Ingram Cancer Center. In 2011, he became a clinical research fellow at Duke University Medical Center and University of Texas MD Anderson Cancer Center learning the minimally invasive surgery for lung cancer and esophageal cancer (VATS and robotic surgery).
He has a solid knowledge in the comprehensive treatment of lung cancer, esophageal cancer, cardiac cancer, and mediastinal tumors based on surgery. He is skilled in the minimally invasive surgery for lung cancer and esophageal cancer and is one of the pioneers in the field of total thoracoscopic esophagectomy with intrathoracic anastomosis for esophageal carcinoma and VATS pulmonary segmentectomy in China. He developed the single-port thoracoscopic radical resection of esophageal cancer with intrathoracic anastomosis.
He has been focused on the basic and clinical translational research on lung cancer and esophageal cancer. He has been the principal investigator of two studies supported by the National Natural Science Fund, five studies supported by Shanghai Municipal Science and Technology Commission, and other two studies. He has published over 50 articles in peer-reviewed journals both in China and abroad, among which over 20 are of SCI-indexed journals. He is the author or contributor of five monographs on oncology. He has obtained 2 national invention patents. He was the winner of the honorable titles of Shanghai Science and Technology Star and Shanghai Science and Technology Star Tracking Plan. Also, he won the seventeenth Meiji Life Science Award and the Scientific and Technological Progress Award of the Chinese Anticancer Association (third grade).
Doctor is a “craftsman” that walks on the line between life and death
In recent years, many people are lured away from their goals set at the beginning of career by “fame” and “wealth”. Against the backdrop, the spirit of craftsmanship, which calls for pragmatism and perfectionism, bucks the trend. People in many industries advocate for the spirit and call themselves “man of cooking”, “man of handiwork”, or “man of teaching”.. Speaking of the spirit of craftsmanship, Prof. Li said, “I think doctors are actually ‘craftsmen’, but our career is just more sensitive. We are “craftsmen” treating disease who walk on the line between life and death”.
When performing a surgery, Prof. Li requires a clean surgical vision and reduces traumas and bleeding as little as possible from incision-making to stitching. He can bring the amount of bleeding down to several milliliters to dozens of milliliters in minimally invasive surgeries. He takes seriously with every surgery, no matter how small it is. “Chinese people emphasize satisfactory conclusion, but this does not mean to only accomplish the last thing perfectly. A doctor should take each surgery as the last one. I love the idea that ‘doctors are craftsmen”, which is a great praise for the career.”
For the spirit of craftsmanship, Prof. Li reckons that it comprises “commitment” and “skill”, and the two are complementary while “commitment” is more important. “For a vicious character in a martial arts novel, the more skilled his martial arts are, the more dangerous he is. Similarly, if a doctor does not have commitment to serving the public, he is not likely to be highly skilled.”
Craftsmanship—“the finest diamond must be cut”
Robot-assisted surgeries
As of March 2018, Ruijin Hospital’s thoracic surgery team had performed more than 600 robot-assisted surgeries. In 2017 alone, the number was 330, which was a considerable figure for any hospital in China or abroad. The great achievements have triggered curiosity about Prof. Li and robot-assisted surgeries.
Prof. Li said he did not know much about robot-assisted surgeries before, and considered them an unrealistic stunt. In 2011, he went to the MD Anderson Cancer Center and the Duke University Medical Center for further study, finding that both medical institutions had been equipped with robotics and doctors were performing robot-assisted surgeries during his visit. At first, he was uninterested in such surgeries, as he deemed that there might be no opportunity to practice at home. However, after he participated in robot-assisted surgeries, he was attracted by the advantages of this technology. Speaking of the feelings at the time, Prof. Li said, “An idea popped up in my mind that robot-assisted surgery is bound to be promising in China. With the improvement of China’s national power, we will make constant progress in such aspects as economy, science and medicine. The medical industry has a strong demand for advanced technologies, and I believe technologies beneficial to patients will take hold in China in the future.”
“I was determined to learn the technology”, Prof. Li said. “Though robot-assisted surgeries are highly operable (Figure 2), with shorter learning curves and higher stability than traditional endoscopic surgery, I was not adapted to it at first. The 3D vision of robot-assisted surgery is demanding on the flexible coordination between hands and eyes, so I practiced a lot in the initial stage. But all goes smoothly after the adaption period.”
As for views on robot-assisted surgeries, Prof. Li said most people hold that doctors should accumulate experience in traditional surgeries and minimally invasive surgeries in order to better perform robot-assisted surgeries. Another view argues that it is advisable to switch from open surgeries directly to robot-assisted surgeries without many obstacles. “In effect, it is hard to say which one is right, but most people are wrong to alienate the technology. Its name may sound like something in a science fiction, but actually it is not the robots but doctors using mechanical arms to perform surgeries. In fact, robots are just extension of human hands, and the effect of surgery mainly depends on doctors’ surgical skills and basic knowledge. A doctor who can perform robot-assisted surgeries must also be skilled at thoracotomy and routine surgeries”.
When tutoring young doctors, Prof. Li stressed, “Surgeons should start with practicing basic skills, including incision-making and knot tying, for steady improvement. One can only perform more demanding and complicated surgeries after mastering these basic skills.” He reckoned that surgeons should not neglect basic skills regardless of the development of medical science and technology; basic skills play a more important role as science and technology advance.
About enhanced recovery after surgery (ERAS)
Prof. Li is not only a master of robot-assisted minimally invasive surgeries but also a pioneer in ERAS. Speaking of the promotion of minimally invasive surgery in recent years, he deemed that the realization of “minimal invasion” is attributable to the progress of science and technology as well as the shift of treatment theory, namely from the pursuit of effective treatment to minimally tolerable treatment. The shift is in line with ERAS.
With the emergence of ERAS, Prof. Li and his team have made much effort. The Thoracic Surgery Department keeps close contact with the Rehabilitation Department since a patient is admitted into Ruijin Hospital, allowing rehabilitation physicians to participate in routine checks, such as ward round (Figure 3), in order to facilitate the patient’s recovery after surgery and enable “seamless connection” between the operating table and rehabilitation room. Besides, Ruijin’s thoracic surgery team conducts preoperative education and works together with psychologists to care for the mental health of patients.
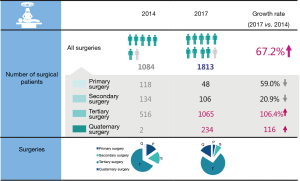
With the relentless efforts made by the thoracic surgery team and the rehabilitation team at Ruijin Hospital, the promotion of ERAS proved fruitful. Prof. Li said, “Since the launch of the ERAS system in 2015, the average duration of hospitalization after surgery has been shortened significantly, while the turnover rate and utilization rate of beds at the hospital have increased considerably (Figure 4). Besides, the number of patients receiving surgeries was much larger than before. Prior to 2015, the number of patients discharged from our department was about 600 to 800 annually, but now the combined number of Ruijin Hospital North and the headquarters is 1,600 to 1,800.” Prof. Li said the rise of ERAS is a mega-trend, and will be popular at medical institutions across China, and the hospital’s thoracic surgery team will continue to promote ERAS.
Spirit of craftsmanship & initial goal—become an all-round doctor excelling in “practicing, learning, and research”
“A man’s energy is limited, but the key is how to concentrate the limited energy to complete indefinite things”, said Prof. Li about the relationship between clinical practices and scientific research.
He believed that clinical practices and scientific research are not competitive but complementary. If a doctor focuses only on performing surgeries and neglects scientific research, he can only be called a man of surgery; similarly, a doctor without practical experience cannot go further down the path of research. “To become a first-rate doctor, one should be good at both medical skills and scientific research. But our ultimate goal of research is to find a better treatment from another point of view,” said Prof. Li.
Prof. Li aimed to become a research-oriented clinician since the beginning of medical study (Figures 5,6). He reckoned that a surgeon should pay more attention to research topics related to clinical science and translational research (Figure 7). The combination of clinical practices and scientific research and the performing of clinical studies kill two birds with one stone. “It is important to relieve patients from pains and cure their diseases, but doctors should also engage in scientific research, and it is significant to better combine clinical practices and research! Put aside medical records and brainstorm solutions to problems identified in cases to make breakthroughs. It is the charm of combing clinical practices with research”. This is Prof. Li’s understanding about the role of doctor.

Interview
JTD: As of March 2018, Ruijin Hospital’s thoracic surgery team had performed more than 600 robot-assisted surgeries. Could you tell us what is the driving force behind your commitment to promoting robot-assisted surgeries? Does the big jump from the first surgery to the 600th surgery have any influence on you?
Prof. Li: We had performed about 600 robot-assisted surgeries as of March 2018, and the figure was 330 in 2017 alone. We have only one goal - bring more benefits to patients. Robot-assisted surgery is a modern and advanced minimally invasive surgery. It has advantages over traditional endoscopic surgery in terms of both the perioperative effectiveness and the operating experiences of operators, so the primary driving force behind our efforts to promote robot-assisted surgery is to benefit both patients and operators.
Whatever we do, we take some time to master it. Robot-assisted surgery is no exception. In effect, I was confident about the advantages of da Vinci robot-assisted surgery when performing the first case. However, as a beginner at the time, I had mixed feelings about it. On one hand, I was excited to learn a new technology conducive to patients; on the other hand, I was a bit nervous because it was completely new to me. Now the number of robot-assisted surgeries has reached 600, and my mental state has changed completely. The learning curve of robot-assisted surgery is relatively short, and we accumulated considerable experience until we performed the 100th one. Now we believe that robot-assisted surgery has become a mature form of surgery that we have well mastered.
JTD: Have you ever planned to conduct some multi-center clinical studies based on robot-assisted surgery cases?
Prof. Li: For now, we conduct clinical studies in a stepwise manner. First, we conducted Meta analyses and retrospective analyses to see the prospect of a technology. For example, some published Meta analyses have shown that robot-assisted surgery has advantages over traditional endoscopic surgeries. Thus, we carried out retrospective analyses and compared the merits and demerits of traditional endoscopes and da Vinci system in lung surgeries. Coincident with the previous studies, the results also suggested robot-assisted surgery as a better solution. After Meta analyses and retrospective analyses, we decided to perform prospective studies in the second stage.
We have started three prospective studies on robot-assisted surgery. They include a randomized controlled clinical trial about robotic vs. thoracoscopic lobectomy, a trial about middle lobe management in lung segmentectomy, and a trial about esophageal cancer surgery. These clinical trials proceed smoothly, but they are limited by the single-center designs. We plan to launch multi-center randomized controlled trials as the next step.
JTD: Are there many domestic hospitals using the da Vinci system in thoracic tumor surgeries? What are the advantages or features of the robot-assisted surgery team at the Thoracic Surgery Department of your hospital as compared with other hospitals?
Prof. Li: An increasing number of hospitals in China have introduced the da Vinci system and performed robot-assisted thoracic surgeries since the first introduction of robotic system in 2006. Only several surgical robots were available in China in 2009, but nearly 70 up to now, driving the growing volume of robotic surgeries. From 2006 to 2017, the number of such surgeries almost doubled every year.
Our department did not perform robot-assisted surgery until May 2015. Today, both the quality and quantity of robotic surgery in our department have reached a high level. Our advantage is that we have an outstanding and cooperative team. Besides, our hospital has two da Vinci systems to ensure reasonable surgery assignment between different departments. There are two days a week that we could spend using the da Vinci system, contributing to the rapid increase in robot-assisted thoracic surgeries in our department. In 2017 alone, our team conducted 330 such surgeries.
JTD: From the perspective of the perioperative effectiveness, is robot-assisted surgery comparable to or better than traditional endoscopic surgery?
Prof. Li: We know that the biggest advantage of robot-assisted surgery is precision and minimal invasion, which means it inflicts very small traumas and thus improves the perioperative effectiveness. Some perioperative indicators are proved more satisfying, including the amount of bleeding, the proportion of thoracotomy, and the duration of hospitalization. Data from our center has shown that the perioperative effectiveness of robot-assisted surgery is equal to or even better than that of traditional endoscopic surgery. Besides, robot-assisted surgery achieves more than traditional endoscopic surgery in lymph node dissection. However, whether these advantages in the perioperative period will be translated into survival benefit has yet to be proven via follow-up and prospective clinical trials.
JTD: As we know, the Thoracic Surgery Department of Ruijin Hospital has established an ERAS system. Could you share your department’s experience in this regard? How do you help patients realize quick recovery?
Prof. Li: ERAS is a new trend in the development of surgery. It can not only enable patients to recover more rapidly but also optimize the utilization of medical resources in the whole society. Our department works closely with the rehabilitation department. Everyday, rehabilitation physicians join thoracic surgeons in ward rounds to learn about patient conditions.
Patients’ recovery involves both physical and mental conditions, so we coordinate with psychologists and rehabilitation physicians to maintain the physical and mental health of patients. Besides, we have set up a preoperative education team, which conducts regular education on patients before surgery to increase their knowledge about preoperative, intra-operative, and postoperative issues and facilitate enhanced recovery. Moreover, we are carrying out a prospective clinical trial about enhanced lung recovery. All above are what our department has done for ERAS, showing our better care for patients.
JTD: ERAS is a foreign concept, and you have been trained in the MD Anderson Cancer Center and Duke University. Could you share your experiences?
Prof. Li: ERAS was first practiced overseas. In 2011, I noticed the difference between domestic and foreign medical institutions regarding the duration of hospitalization during my study abroad. In a foreign center, patients usually do not stay long in hospital. They make an appointment at the outpatient department and arrive at the hospital on the day of surgery. Many patients can get out of bed on the second day after surgery, and some even can walk around with chest bottles. However, it is quite a different story in China. Patients must stay in bed for a long period of time after surgery and are unwilling to have rehabilitation exercises early. Meanwhile, few doctors encourage patients to do so.
After getting familiar with the ERAS concept during my stay overseas, I realized that ERAS is not just about theoretical promotion. It is highly practicable. Generally speaking, the introduction of ERAS into China’s medical system is suitable and feasible, and is favorable to both patients and hospitals.
JTD: When did your department introduce the concept of ERAS? What motivated you to establish the ERAS system?
Prof. Li: The concept of ERAS actually comprises many parts. Ruijin Hospital had made efforts in this direction, but it was not until 2015, when I joined the hospital, that the concept was applied in a large scale. Since then, we have publicized the concept, conducted clinical trials, and partnered with the rehabilitation department to practice it.
I witnessed the implementation of ERAS concept at Ruijin Hospital. I believed ERAS would eventually become a mega-trend. Most Chinese hospitals are in short of resources, and our hospital also faces a bed shortage. Therefore, the implementation of ERAS at the time was to optimize the utilization of limited medical resources to offer better services to patients.
JTD: As a thoracic surgeon, how do you think about ERAS? What benefits can it bring to patients?
Prof. Li: As a thoracic surgeon, I have seen the direct benefits brought by ERAS programs to patients. Before the introduction of ERAS, patients widely held that thoracic surgery was a big surgery and they would have to stay in bed for a week or even longer. But actually, it is painful for patients to stay in bed for a long period of time, which is unfavorable to their recovery. After we introduced the ERAS system, we adopted various measures to reduce trauma and shorten the duration of rehabilitation. Now, most patients can get out of bed one day after thoracic surgery. Their pains are mitigated and the recovery process is accelerated. Patients can recover at a faster pace both physically and mentally. This is a direct benefit brought by ERAS to patients.
JTD: What may be the problems in the implementation of ERAS in thoracic surgery department?
Prof. Li: Though the implementation of ERAS system is going smoothly, there are some problems as well. Doctors have adopted some measures, such as analgesia, minimally invasive surgery, early activities out of bed, and recovery of lung, which indeed speed up the physical recovery. However, some patients and even some doctors stick to traditional views, such as “injured sinews and bones take one hundred days to recover”. The patients want to stay in the hospital for some time even though they can be discharged, but longer stay is not beneficial to patients. Some patients suffer cross-infection during hospitalization. So I think it is important to publicize the ERAS concept and this is also one of the reasons for our promotion of preoperative education.
JTD: We know that airway management during perioperative period is an important part of ERAS. Does your department have a special way of airway management? How do you practice it?
Prof. Li: We attach high importance to airway management during perioperative period, as it is directly linked to the recovery of patients and the complication rate after a thoracic surgery. Airway management is particularly important to patients with chronic obstructive pulmonary disease and pulmonary emphysema. Many thoracic surgery patients more or less have airway problems, especially in face of serious air pollution; therefore, we pay special attention to the airway health of patients during the perioperative period.
We are conducting a clinical trial targeting patients with lung dysfunctions, which enhances preoperative airway management and observes whether postoperative complications and recovery of patients improve. The preliminary results of this randomized controlled trial have shown that intensive airway care during perioperative period is favorable to the improvement of lung function and the postoperative recovery.
JTD: Do you think there are special issues in airway management during perioperative period before, during, and after surgery, respectively?
Prof. Li: Airway management is indeed a systematic process, and preoperative, intra-operative, and postoperative care is important. Before the surgery, there are usually some physical therapies and medical treatments, such as the use of bronchodilators to reduce secretions and improve lung function. Preoperative care is especially important for smoking patients or patients with chronic obstructive pulmonary disease. Some patients who are not qualified to receive surgery due to poor lung function may be able to have surgery after receiving preoperative airway management. Our clinical experience and relevant studies indicate that preoperative airway management can pave the way for surgery, which is conducive to patients.
Intra-operative airway management is of equal importance, and this process involves the cooperation between anesthetists and surgeons. For instance, the use of tubes for anesthesia or the approaches of intubation can affect the recovery of airways. Postoperative airway management is closely related to enhanced recovery. We encourage patients for early activities and early coughing and expectoration. Also, we use aerosolized agents and bronchodilators to accelerate the recovery.
JTD: In view of the status quo of thoracic surgery, do you think there are drawbacks/difficulties in perioperative airway management and ERAS? How can we improve them?
Prof. Li: EARS still lacks evidences from randomized controlled clinical trials. Most clinicians still do not have a clear picture of the concept of ERAS, such as its content. Besides, different measures are used to implement it. Although some guidelines on perioperative airway management have been released, relevant standards and criteria have yet to be unified, which should be improved via clinical practices. I hope to see more clinical studies and data to support the concept of ERAS, so that ERAS can be accepted by more people.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
(Science Editor: Elaine Xu, JTD, jtd@amepc.org)