The history of lung transplantation in Hong Kong
The first attempt at human lung transplantation was made in 1963 by Hardy in the USA, but the donor survived only 18 days. In 1983, the first successful human lung transplantation was achieved in Toronto by Joel Cooper and Alec Patterson—this was a single lung transplant for pulmonary fibrosis. Three years later, Cooper and Patterson achieved the first double lung transplant for emphysema. Since those days, lung transplantation has been established as an accepted treatment for patients suffering from end stage lung failure. According to the registry data from the International Society for Heart and Lung Transplantation (ISHLT), over 4,000 cases of lung transplantation are performed each year worldwide (1).
In Hong Kong, the first single lung transplant was performed in the Grantham Hospital in 1995 by Dr. Clement S. W. Chiu for a young female patient suffering from lymphangioleiomyomatosis (LAM). In the same year, Dr. Chiu also performed the first case of heart-lung transplantation in Hong Kong. Two years later in 1997, Dr. Chiu performed the first case of double lung transplant in form of sequential lung transplant in Hong Kong.
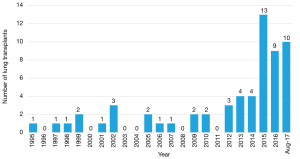
Like all the lung transplant centers in the world, the volume of lung transplant in Hong Kong has been limited by the scarcity of suitable donor lungs. The number of referrals for consideration for lung transplants were also small in the initial years. The average number of transplants performed in the first 15 years of the program were 1.2 cases per year. With the increasing acceptance of organ donation by the Hong Kong general public, as well as an increase in the number of patients being referred for consideration for lung transplant, there has been a marked increase in lung transplant since 2014, with the current average number of lung transplant being about 12 per year (Figure 1).
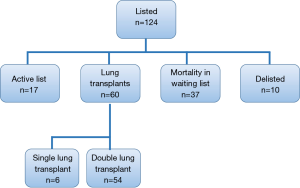
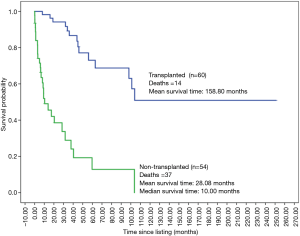
Since the start of the lung transplant program in Hong Kong, a total of 124 patients were listed for lung transplant. Out of these, 60 were transplanted, of whom 54 were double lung transplants, and 6 were single lung transplants. At the time of writing, 17 of the listed patients are on the active waiting list. Thirty-seven patients died while on the waiting list, and ten patients were delisted (Figure 2). Please refer to Table 1 for the demographic characteristics of the patients who were listed for lung transplant.
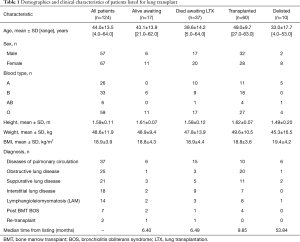
Full table
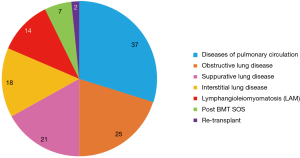
The underlying pathology of the patients listed for lung transplant in Hong Kong is very different from that reported in the ISHLT Registry. With the extremely low prevalence of cystic fibrosis and alpha-1-antitrypsin deficiency in the local population, there were no patients with such diagnoses in our lung transplant waiting list. Patients with diseases of the pulmonary circulation make up the largest percentage of the waiting list at 42%. Patients with obstructive lung disease is the second largest category at 25%, followed by suppurative lung disease at 21%, and interstitial lung diseases at 18%. Interestingly, patients with LAM consist of 14% of all the patients on the lung transplant waiting list (Figure 3).
As expected, the survival outcome is significantly better for listed patients who received a lung transplant versus those who did not receive a lung transplant (Figure 4).
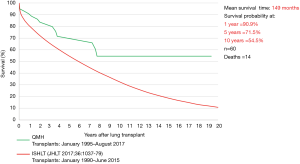
Although the Hong Kong lung transplant program has a very small volume, the results compare quite favorably with the ISHLT Registry database (1). The 1-year Kaplan-Meier survival in the Hong Kong lung transplant program is 90.9% vs. 82.0% of the ISHLT (for double lung transplants). The 5-year survival in Hong Kong program is 71.5% vs. 59.0% of the ISHLT. The 10-year survival in Hong Kong is 54.5% vs. 41% in the ISHLT (Figure 5).
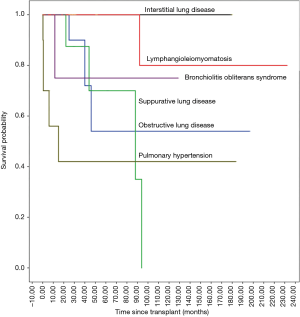
In terms of patient survival after lung transplant by disease category, patients with LAM, Bronchiolitis Obliterans and interstitial lung diseases fare best. The worst outcomes are seen in patients with diseases of the pulmonary circulation, which is in line with the reported literature (Figure 6). There is no significant survival difference between patients with double lung transplant vs. single lung transplant.
In the early days of the Hong Kong lung transplant program, the age limits of recipients were more restrictive than the ISHLT guidelines, and they were set at 60 years for single lung transplant, 55 years for double lung transplant, and 50 years for heart lung transplant. These have been revised in the early 2010s. Currently, all patients below the age of 65 will be routinely accepted for assessment for lung transplant, with the final decision based on the biological age, performance and/or other relative contraindications.
In conclusion, the lung transplant program in Hong Kong has been established since the 1990s with the volume of activity being very low in the early years. There has been a clear trend of increasing volume in the past few years. The recipient pathology is very different from the ISHLT database, with complete absence of cystic fibrosis and alpha-1-antitrypsin deficiency, and a predominance of diseases of the pulmonary circulation. LAM has a much higher representation on the waiting list than the ISHLT. The survival of patients who received a lung transplant in Hong Kong compares favorably with international data.
Future strategies that may increase the lung transplant volume in Hong Kong include the implement of ex vivo lung perfusion to increase the utilization of available cadaveric donor lungs, the introduction of living donor lobar lung transplant, and the use of donor lung organs after circulatory death as an alternative means of deceased organ donation.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Chambers DC, Yusen RD, Cherikh WS, et al. The Registry of the International Society for Heart and Lung Transplantation: Thirty-fourth Adult Lung And Heart-Lung Transplantation Report-2017; Focus Theme: Allograft ischemic time. J Heart Lung Transplant 2017;36:1047-59. [Crossref] [PubMed]