Easy clinical-ECG criteria to suspect total occlusion of left main in acute coronary syndrome
Clinical vignette
A 48-year-old man with a history of smoking, high blood pressure, moderate alcoholism, occasional cocaine consumer, sleep apnea syndrome and family history of ischemic heart disease.
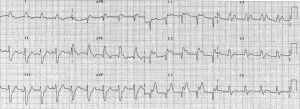
At 4 o’clock, while working, he presented an intense, oppressive precordial pain radiating on his shoulders; He went to his clinic center where the first diagnostic ECG was performed at 5:10 PM (Figure 1). Two hundred and fifty mg of aspirin, 600 mg of clopidogrel and sublingual nitroglycerin were administered. The reference hospital for emergent primary angioplasty was contacted
It was accessed via the right radial approach with the following findings: Right Coronary artery dominant without significant lesions, left main trunk (LMT) occluded distally with TIMI 0 flow and no collateral hetero-coronary circulation. Aortic counterpulsation balloon was placed and dobutamine was started at a dose of 3 mcg/kg/min. Primary PCI was performed on the LMT with thrombus aspiration catheter obtaining a TIMI 3 flow in left circumflex coronary artery (LCx), and TIMI 2 flow in left coronary descending coronary artery (LAD) and first diagonal branch. The patient was admitted to the Coronary Care Unit in a situation of cardiogenic shock
ECG description and discussion
It is very important to clarify and describe the term of sub-occlusion and occlusion of the LMT because the ECG pattern, treatment and prognosis are totally different. Usually, acute coronary syndrome due to involvement of the LMT, as a culprit artery, presents with either sub-total occlusion or total occlusion with good collateral circulation. In this case, the ECG shows non-STEMI pattern with 7 or more leads with ST depression and a reciprocal ST elevation in aVR and often in V1 (1,2). Acute complete occlusion of LMT rapidly triggers cardiogenic shock and ventricular fibrillation, and the patient usually dies before reaching the emergency department (3). However, new treatments and logistic systems of care have enabled prompt arrival to the emergency department, and consequently more patients with complete occlusion of the LMT are seen in clinical practice. Nevertheless, in-hospital mortality remains high.
The most important characteristic of this ECG pattern is that it may be similar to that of proximal occlusion of the LAD without ST elevation in V1 and aVR but, with ST elevation in V2 to V4–6 leads and in I and aVL leads, as well as ST depression in the inferior leads (3,4) and often, with right bundle branch block and left anterior hemiblock. In complete occlusion of the LMT the ischemic vector is directed forward and little upward because is the result of the cancellation of the vectors of the proximal LCx and LAD occlusions. This causes the lack of ST changes in V1 and aVR that are frequently found in complete proximal LAD occlusion. ST elevation is not always present in V1 despite proximal LAD occlusion to first septal if exists a large conal branch from the RCA (5) that perfuses the high septum together with the first septal branch, but patients with LMT occlusion who survive usually present a poor hemodynamic state when compared to those with LAD proximal occlusion: cardiogenic shock/cardiac arrest, high hospital mortality, Right Bundle Branch Block and Left anterior hemiblock.
Points to ponder
We must suspect complete LMT occlusion when the patient presents cardiogenic shock, proximal LAD occlusion pattern without ST-segment elevation in aVR and V1 and severe intraventricular conduction disturbances.
Acknowledgements
The authors would like to thank Physicians of the Cat lab, Hospital Son Espases, Palma, Mallorca.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Kosuge M, Kimura K, Ishikawa T, et al. Predictors of left main or three-vessel disease in patients who have acute coronary syndromes with non-ST-segment elevation. Am J Cardiol 2005;95:1366-9. [Crossref] [PubMed]
- Nikus K, Pahlm O, Wagner G, et al. Electrocardiographic classification of acute coronary syndromes: a review by a committee of the International Society for Holter and Non-Invasive Electrocardiology. J Electrocardiol 2010;43:91-103. [Crossref] [PubMed]
- Fiol M, Carrillo A, Rodríguez A, et al. Electrocardiographic changes of ST-elevation myocardial infarction in patients with complete occlusion of the left main trunk without collateral circulation: differential diagnosis and clinical considerations. J Electrocardiol 2012;45:487-90. [Crossref] [PubMed]
- Jong GP, Ma T, Chou P, et al. Reciprocal changes in 12-lead electrocardiography can predict left main coronary artery lesion in patients with acute myocardial infarction. Int Heart J 2006;47:13-20. [Crossref] [PubMed]
- Ben-Gal T, Herz I, Solodky A, et al. Acute anterior wall myocardial infarction entailing ST-segment elevation in lead V1: electrocardiographic and angiographic correlations. Clin Cardiol 1998;21:399-404. [Crossref] [PubMed]


