Using the scoring schemes in the right way: the dynamic assessment of stroke and bleeding risk in patients with atrial fibrillation
Atrial fibrillation (AF) is an important risk factor of ischemic stroke (1), and stroke prevention is the cornerstone for the AF management. The decision about the prescriptions of oral anticoagulants (OACs) should be based on the stroke risk of each AF patients. Also, the bleeding risk of anticoagulated patients should be evaluated, so that closer follow-up could be arranged for those who are potentially at risk, and modifiable bleeding risk factors could be corrected. The CHA2DS2-VASc and HAS-BLED scores were commonly used to assess the risk of ischemic stroke and major bleeding of AF patients, respectively (2,3). However, these risk scores are usually calculated according to the baseline characteristics of patients, and the outcomes are determined after several years. Since patients would become older and get more comorbidities, the estimations of the stroke and bleeding risks based on the baseline risk scores could be inaccurate.
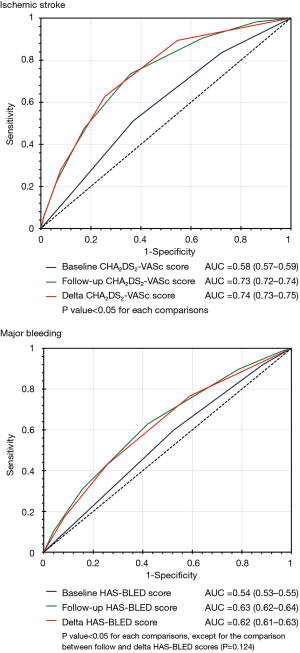
We thank Yoon et al. (4) for their comments on our recently published manuscript demonstrating that the delta CHA2DS2-VASc score (the increase in score between baseline and follow-up) was useful in predicting the occurrence of ischemic stroke among AF patients (5). In our analysis which focused on AF patients without comorbidities of the CHA2DS2-VASc scheme at baseline, the area under the receiver operating characteristic curve (AUC) of the delta CHA2DS2-VASc in the prediction of ischemic stroke was significantly higher than that of the baseline CHA2DS2-VASc score (0.74 vs. 0.58, P<0.05) (Figure 1). Interestingly, the AUC of the baseline CHA2DS2-VASc score in predicting ischemic stroke seems to be lower among patients without comorbidities at baseline (AUC =0.58) than among those with comorbidities having a full-range of the CHA2DS2-VASc score (AUC =0.698) reported in previous studies (7,8). Since nearly 90% of AF patients without comorbidities at baseline would develop at least one new stroke risk factor before they experienced ischemic stroke (5), it could be expected that the predictive accuracy of the baseline CHA2DS2-VASc score in predicting ischemic stroke is suboptimal among initially low-risk patients.
Not only stroke, but the bleeding risk of AF patients were dynamic. Among 19,566 AF patients with a baseline HAS-BLED score of 0–2 receiving warfarin for stroke prevention, the mean HAS-BLED score increased from 1.43 to 2.45 during the follow up of 93,783 person-years (6). The AUC of the follow-up or delta HAS-BLED score in the prediction of major bleeding was significantly higher than that of the baseline HAS-BLED score (Figure 1). Most importantly, the risk of major bleeding is especially higher within the 3 months after the HAS-BLED score changed (6), and therefore, clinical physicians should be highly alert to correct any modifiable bleeding risk factors once the patient got it to minimize the subsequent risk of major bleeding.
The concept of delta CHA2DS2-VASc and delta HAS-BLED scores we proposed clearly highlighted the importance of regular reassessment of the stroke and bleeding risks of AF patients which has been mentioned in the previous AF guideline (9). The right way to use the scoring schemes is to reassess the risk regularly, correct the modifiable risk factors appropriately and prescribe OACs timely.
Acknowledgements
Funding: This work was supported in part by grants from the Ministry of Science and Technology (MOST 104-2314-B-075-024-MY3) and Taipei Veterans General Hospital (V107B-001, V107B-022, V107C-200), Taipei.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Chao TF, Liu CJ, Tuan TC, et al. Lifetime Risks, Projected Numbers, and Adverse Outcomes in Asian Patients With Atrial Fibrillation: A Report From the Taiwan Nationwide AF Cohort Study. Chest 2018;153:453-66. [Crossref] [PubMed]
- Lip GY, Nieuwlaat R, Pisters R, et al. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest 2010;137:263-72. [Crossref] [PubMed]
- Pisters R, Lane DA, Nieuwlaat R, et al. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest 2010;138:1093-100. [Crossref] [PubMed]
- Yoon M, Joung B. Dynamic stroke risk scores of atrial fibrillation. J Thorac Dis 2018;10:1332-4. [Crossref] [PubMed]
- Chao TF, Lip GYH, Liu CJ, et al. Relationship of Aging and Incident Comorbidities to Stroke Risk in Patients With Atrial Fibrillation. J Am Coll Cardiol 2018;71:122-32. [Crossref] [PubMed]
- Chao TF, Lip GY, Lin YJ, et al. Incident Risk Factors and Major Bleeding in Patients with Atrial Fibrillation Treated with Oral Anticoagulants: A Comparison of Baseline, Follow-up and Delta HAS-BLED Scores with an Approach Focused on Modifiable Bleeding Risk Factors. Thromb Haemost 2018;118:768-77. [PubMed]
- Chao TF, Liu CJ, Wang KL, et al. Using the CHA2DS2-VASc score for refining stroke risk stratification in 'low-risk' Asian patients with atrial fibrillation. J Am Coll Cardiol 2014;64:1658-65. [Crossref] [PubMed]
- Chao TF, Liu CJ, Tuan TC, et al. Comparisons of CHADS2 and CHA2DS2-VASc scores for stroke risk stratification in atrial fibrillation: Which scoring system should be used for Asians? Heart Rhythm 2016;13:46-53. [Crossref] [PubMed]
- European Heart Rhythm Association, Heart Rhythm Society, Fuster V, et al. ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation--executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation). J Am Coll Cardiol 2006;48:854-906. [Crossref] [PubMed]