MitraClip procedure prior to left ventricular assist device implantation
Introduction
Functional mitral valve regurgitation is a frequent consequence of left ventricular dysfunction in patients with severe heart failure and is associated with a poor prognosis (1). It is anticipated that in this patient group the mitral valve repair, respectively replacement, improves hemodynamics and clinical symptoms (2). As operative interventions with the help of heart-lung-machine are high risk procedures in these cases, the transcatheter mitral repair with MitraClip® (Abbott Vascular, IL, USA) has recently become frequently used. The MitraClip procedure is safe with high procedural success rate and low procedural mortality (3,4). Most of these cases lead to left ventricular dysfunction, which finally ends in an implantation of a left ventricular assist device, the fastest developing treatment option in cardiac surgery (5-15).
In this report, we describe six cases in which patients with end-stage heart failure and consecutive functional mitral valve regurgitation were supported with a left ventricular assist device after MitraClip implantation.
Methods
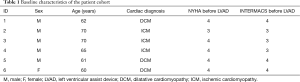
This case series includes 6 patients (5 males, 1 female). The mean age at MitraClip procedure was 64.6 years, mean age at time of LVAD implantation was 65.5 years. All patients had functional mitral regurgitation (MR). The description of each case is provided in this section.
Case 1
The first case was a 62-year-old male with dilated cardiomyopathy and accompanying grade three to four MR. At that time the ejection fraction (EF) was 10% (Simpson), New York Heart Association (NYHA) classification was grade four, left ventricular end-diastolic diameter (LVEDD) was 64 mm and cardiac index (CI) was 2.5 L/min/m2. A MitraClip device was successfully implanted in May 2014 which led to a reduction of the MR to grade one to two. The EF increased to 20%, NYHA classification remained unchanged, the LVEDD increased to 70 mm and the CI decreased to 2.01 L/min/m2. In October 2015 he presented with recurrent cardiac decompensations, NYHA IV symptoms, pulmonary hypertension, moderately right heart failure and INTERMACS 3 graduation. A centrifugal third generation left ventricular assist device (LVAD) (HeartMate 3, Abbott) was implanted urgently in October 2015. Due to a previously implanted Paracor® HeartNet device (Paracor Medical, Sunnyvale, CA, USA), the operation was a high-risk procedure. Right heart failure occurred postoperatively and required inotropic support and mechanical ventilation for 21 days. Other postoperative complications included atrial fibrillation, bleeding with the need of redo thoracotomy and a septiformal hemodynamic situation requiring vasoconstrictive medical support. Unfortunately, the patient died on postoperative day 21 due to multi-organ failure.
Case 2
A 70-year-old male with ischemic cardiomyopathy, consecutive grade three MR and grade three tricuspid regurgitation (TR) presented with NYHA grade four symptoms and pulmonary hypertension. The EF at that time was 25%, LVEDD 68 mm and CI 2.6 L/min/m2. In March 2010 a MitraClip implantation was successfully performed. The MR was reduced to grade two as well as the TR. The EF decreased to 15%, the LVEDD increases to 71 mm and the CI to 1.92 L/min/m2. In October 2010 there was a readmission with signs of NYHA III decompensation and consisting grade two secondary MR. On October 12, 2010 an HVAD (Medtronic, Minnesota, MN, USA) centrifugal pump was implanted and supported the patient for 41 days until the patient died because of a hypoxic brain damage.
Case 3
A 70-year-old male was diagnosed with ischemic cardiomyopathy presented with decompensated heart failure NYHA class IV, MR grade three to four and TR grade two. There was a mitral and tricuspidal regurgitation grade two. At hospital admission the patient was at INTERMACS grade 3. Echocardiographic assessment revealed an EF of 20% with a LVEDD of 60 mm. The CI was evaluated at 2.3 L/min/m2. A MitraClip was implanted on July, 2013. Within one year after the procedure MR decreased to grade one to two and TR remain unchanged. The EF decreased to 15%, LVEDD increased to 66 mm and CI was evaluated with 1.94 L/min/m2. On July, 2014 the patient was readmitted with NYHA grade four for LVAD implantation. A HVAD (Medtronic, Minnesota, MN, USA) centrifugal pump and a biological tricuspid valve were successfully implanted.
Case 4
A 65-year-old male with ischemic cardiomyopathy and NYHA class III heart failure symptoms was diagnosed with a MR II to III and an EF of 26%. The echocardiography presented a LVEDD of 79 mm, CI was 2.89 L/min/m2. A MitraClip procedure was performed with no intraoperative complications. After the procedure the MR decreased to grade I. There has been no change in the value of the EF after intervention. The LVEDD increased to 86 mm. After 20 months the patient exhibited heart failure symptoms NYHA IV. The INTERMACS classification at hospital readmission was stage 3. The MR was mild with first degree. The echocardiography showed an EF of still 25% and an increased LVEDD of 86 mm. In a right heart catheter the CI was 1.97 L/min/m2 and the PCWP was 11 mmHg. An HVAD centrifugal left ventricular assist device was implanted at this time. There were no postoperative complications. After LVAD implantation the heart failure symptoms decreased to NYHA 2.
Case 5
A 61-year old male was diagnosed with dilated cardiomyopathy, secondary MR grade three and TR grade two. At first hospital admission NYHA classification was three, INTERMACS classification was stage four. The EF was evaluated with 10%, LVEDD was 92 mm and CI was 2.1 L/min/m2. In July 2014 a MitraClip procedure was performed. After five months the MR was reduced to grade two and TR remained unchanged. The EF remained nearly unchanged (13%). The LVEDD decreased to 73 mm and the CI increased to 2.5 L/min/m2. In December, 2014 the patient was readmitted in our hospital with NYHA grade four symptoms and recurrent signs of cardiac decompensation. An LVAD implantation (HeartWare, Medtronic) was successfully performed.
Case 6
A 60-year-old female exhibited dilated cardiomyopathy and grade three MR as well as tricuspid regurgitation. At first hospital admission the NYHA classification was grade three. The EF was 24%, LVEDD was 60 mm and CI was 2.98 L/min/m2. She underwent MitraClip procedure, after which the MR (grade one) and the LVEDD improved (55 mm). The EF decreased to 15%. The TI did not change after MitraClip procedure. After 49 days NYHA classification changed to grade four with recurrent symptoms of cardiac decompensation. An LVAD (Medtronic) and tricuspid ring was successfully implanted.
Results
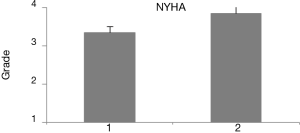
Six patients (5 males, 1 female) with a mean age of 64.6 years at MitraClip procedure, and mean age at time of 65.5 years at LVAD implantation, were treated as part of this study. All patients had functional MR and demonstrated successfully reduced severity of MR after treatment. All patients were discharged with MR I-II and NYHA functional class III or IV after MitraClip-procedure (Table 1).
Full table
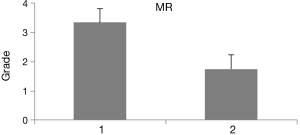
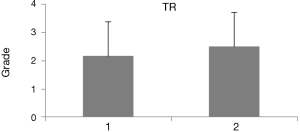
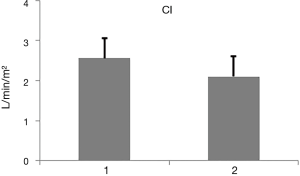
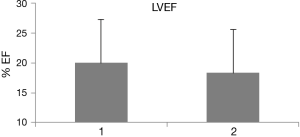
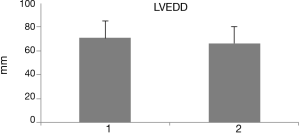
The mean CI was 2.93 before MitraClip-procedure and 2.36 before LVAD-Implantation. Mean LVEDD was 71 mm before MitraClip, mean LVEDD was 70.6 mm before LVAD, and 63.2 mm after LVAD implantation respectively. The mean PCWP was 21.5 mmHg before MitraClip and 19.8 mmHg before LVAD implantation respectively. The mean LVEF was 19.2% before MitraClip, the mean LVEF was 17.6% before LVAD and 15% after LVAD implantation (Figures 1-6). Two of the LVAD implanted patients died due to postoperative complications. There were no complications after MitraClip procedure. Furthermore there were no adverse events and complications caused by the interventional approach regarding the iatrogenic atrioseptal defect.
Discussion
Although the MitraClip procedure improves hemodynamic parameters and therefore symptoms of patients with high grade mitral regurgitation and is frequently used as the implantation can be easily done via transcatheter technique, little is known of the outcome in patients with end-stage heart failure (16-18). In the presented case series, we have reported on six patients who underwent left ventricular assist device implantation in our clinic after a MitraClip procedure due to secondary mitral valve regurgitation.
As expected, there was a significant improvement of the mitral regurgitation in all patients (Figure 2), which led to an improvement of clinical symptoms (dyspnea, edema, physical capacity). However, no other cardiac parameter improved as for example the EF or LVEDD. There was even an overall worsening of tricuspidal regurgitation (Figure 4), which could be due to the combination of the left ventricular failure, which has adapted to the MR. An improvement of the MR with the MitraClip procedure could lead to a functional (or relative) stenosis with an increased pressure load of the right ventricle with an increase of the tricuspidal annulus.
The presented cases demonstrate that the percutaneous interventional MitraClip procedure leads not to surgical-technical problems regarding the subsequent implantation of the LVAD.
The validity of the results in this case series is limited by the selection of the patients. All the patients were heart failure patients who were refractory to the percutaneous mitral valve repair therapy.
Conclusions
Our presented patient cohort presented little hemodynamic improvement of hemodynamic after the MitraClip procedure. There was no clinical benefit for the patients after MitraClip procedure, progressing left ventricular dysfunction could not be prevented and resulted in subsequent LVAD implantation.
Acknowledgements
This manuscript was kindly supported by a grant of the German Research Foundation (Deutsche Forschungsgemeinschaft, DFG) through the project “KFO 311” (Principal Investigators: Prof. Johann Bauersachs, Prof. Marius Hoeper, Prof. Jan D. Schmitto).
Footnote
Conflicts of Interest: JD Schmitto and G Dogan are consultants for Abbott and Medtronic. The other authors have no conflicts of interest to declare.
Ethical Statement: Ethics committee approval was not required for this study as it was a retrospective analysis falling under the general patient consent given with stationary admission or implantation at the Hannover Medical School. Written informed consent was obtained from the patients for publication of this manuscript and any accompanying images.
References
- Park SJ, Milano CA, Tatooles AJ, et al. Outcomes in advanced heart failure patients with left ventricular assist devices for destination therapy. Circ Heart Fail 2012;5:241-8. [Crossref] [PubMed]
- Asgar AW, Mack MJ, Stone GW. Secondary mitral regurgitation in heart failure: pathophysiology, prognosis, and therapeutic considerations. J Am Coll Cardiol 2015;65:1231-48. [Crossref] [PubMed]
- Vakil K, Roukoz H, Sarraf M, et al. Safety and efficacy of the MitraClip® system for severe mitral regurgitation: a systematic review. Catheter Cardiovasc Interv 2014;84:129-36. [Crossref] [PubMed]
- Feldman T, Foster E, Glower DD, et al. Percutaneous repair or surgery for mitral regurgitation. N Engl J Med 2011;364:1395-406. [Crossref] [PubMed]
- Kirklin JK, Naftel DC, Pagani FD, et al. Seventh INTERMACS annual report: 15,000 patients and counting. J Heart Lung Transplant 2015;34:1495-504. [Crossref] [PubMed]
- Schmitto JD, Hanke JS, Rojas SV, et al. First implantation in man of a new magnetically levitated left ventricular assist device (HeartMate III). J Heart Lung Transplant 2015;34:858-60. [Crossref] [PubMed]
- Feldmann C, Chatterjee A, Hanke JS, et al. Novel centrifugal pump for heart failure patients: initial success and future challenges. J Thorac Dis 2017;9:1429-31. [Crossref] [PubMed]
- Feldmann C, Chatterjee A, Haverich A, et al. Left Ventricular Assist Devices - A State of the Art Review. Adv Exp Med Biol 2018;1067:287-94. [Crossref] [PubMed]
- Schmitto JD, Molitoris U, Haverich A, et al. Implantation of a centrifugal pump as a left ventricular assist device through a novel, minimized approach: upper hemisternotomy combined with anterolateral thoracotomy. J Thorac Cardiovasc Surg 2012;143:511-3. [Crossref] [PubMed]
- Schmitto JD, Rojas SV, Haverich A. Left Ventricular Assist Devices for Advanced Heart Failure. N Engl J Med 2017;376:1894. [PubMed]
- Schmitto JD, Mokashi SA, Cohn LH. Past, present, and future of minimally invasive mitral valve surgery. J Heart Valve Dis 2011;20:493-8. [PubMed]
- Schmitto JD, Lee LS, Mokashi SA, et al. Functional mitral regurgitation. Cardiol Rev 2010;18:285-91. [Crossref] [PubMed]
- Hanke JS, Rojas SV, Avsar M, et al. HeartWare left ventricular assist device for the treatment of advanced heart failure. Future Cardiol 2016;12:17-26. [Crossref] [PubMed]
- Hanke JS, Rojas SV, Avsar M, et al. Minimally-invasive LVAD Implantation: State of the Art. Curr Cardiol Rev 2015;11:246-51. [Crossref] [PubMed]
- Ricklefs M, Hanke JS, Dogan G, et al. Less Invasive Surgical Approaches for Left Ventricular Assist Device Implantation. Semin Thorac Cardiovasc Surg 2018;30:1-6. [Crossref]
- Taramasso M, Maisano F, Latib A, et al. Clinical outcomes of MitraClip for the treatment of functional mitral regurgitation. EuroIntervention 2014;10:746-52. [Crossref] [PubMed]
- Parikh KS, Mehrotra AK, Russo MJ, et al. Percutaneous transcatheter aortic valve closure successfully treats left ventricular assist device-associated aortic insufficiency and improves cardiac hemodynamics. JACC Cardiovasc Interv 2013;6:84-9. [Crossref] [PubMed]
- Kitada S, Kato TS, Thomas SS, et al. Pre-operative echocardiographic features associated with persistent mitral regurgitation after left ventricular assist device implantation. J Heart Lung Transplant 2013;32:897-904. [Crossref] [PubMed]