Right ventricular outflow tract obstruction caused by a foreign body granuloma originating from a Dacron® graft 30 years after transannular patching
Case presentation
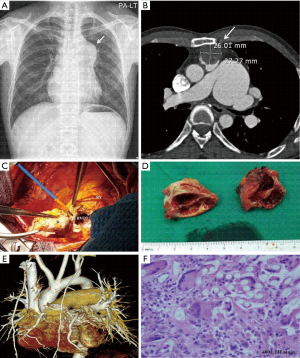
A 43-year-old man with a surgical history of atrial septal defect (ASD) patch closure and transannular right ventricular outflow tract (RVOT) reconstruction using a Dacron® patch 30 years ago visited our hospital due to dyspnea on exertion (NYHA class II), which started 4 months prior to presentation. Imaging studies revealed a mass obstructing the RVOT, causing severe poststenotic pulmonary artery dilation (Figure 1A,B). The initial diagnosis was suspected intrapulmonary malignancy, such as an angiosarcoma. Prompt surgery was performed for diagnosis and treatment. After establishing standard cardiopulmonary bypass, the mass was completely excised including the native pulmonary valve and the previous Dacron® graft. On gross examination, the mass was fully covered by neo-intima internally and fibrotic tissue externally (Figure 1C). However, ingrowth of the mass to the lumen caused near complete obstruction of the RVOT. Transection of the mass revealed hyperproliferation of granulation tissue under the pseudointimal layer fused with the Dacron® patch (Figure 1D). After removing the mass, pulmonary valve replacement and RVOT hood formation with a Gore-Tex® membrane was performed followed by additional main pulmonary artery reduction angioplasty (Figure 1E). The operation and postoperative course were uneventful. Final tissue diagnosis of the mass indicated a foreign body granuloma consisting of multiple giant cells with lymphocyte infiltration (Figure 1F).
Discussion
After implanting vascular prostheses, complex reactions occur to integrate these foreign materials into the body forming neointima to cover the prostheses. The acute phase of this process is mediated by type II (cytotoxic) hypersensitivity reactions and type III (immune) reactions (1). However, this process can sometimes be exaggerated by hypersensitivity reactions, as these prostheses continually act as “non-self” substances and type IV late hypersensitivity reactions occur with transformation of T-lymphocytes and macrophages into multinucleated giant cells resulting in foreign body granuloma formation. The duration and severity of these reactions are not known and are affected by multiple factors, including host factors and types of synthetic polymers used in the prostheses.
Dacron® (polyethylene terephthalate) grafts are widely used as substitutes for the arterial wall because of the well-known long-term durability (2). However, these grafts also have high degrees of immunogenicity and porosity, which can lead to an exaggerated hypersensitivity reaction. There have been many reports regarding delayed foreign body reactions after Dacron® graft implantation in other surgical fields, including abdominal surgery and orthopedic surgery (3,4). However, granulomas originating from Dacron® grafts in cardiac RVOT have rarely been reported. This may be due to the low-pressure characteristics of the right side of the heart with low hemodynamic stress. Although the incidence is low, foreign body granulomas after cardiac patching can be problematic because of their hemodynamic role, as in our case, interrupting blood flow and inducing severe hemodynamic stenosis.
In addition to the well-known late complications such as pulmonary insufficiency and pulmonary stenosis after transannular RVOT reconstruction, it is necessary to note that overactive immunological reactions to Dacron® grafts can also be problematic. In addition, this case demonstrates the importance of longitudinal lifetime follow-up in patients after cardiac surgery.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Russu E, Mureșan AV, Cordoș BA, et al. Morpho-Pathological Review on the Healing of Synthetic Vascular Grafts. Acta Medica Marisiensis 2016;62. [Crossref]
- Nagano N, Cartier R, Zigras T, et al. Mechanical properties and microscopic findings of a Dacron graft explanted 27 years after coarctation repair. J Thorac Cardiovasc Surg 2007;134:1577-8. [Crossref] [PubMed]
- Veleirinho B, Coelho DS, Dias PF, et al. Foreign body reaction associated with PET and PET/chitosan electrospun nanofibrous abdominal meshes. PLoS One 2014;9. [Crossref] [PubMed]
- Pushpasekaran N, Muthulingam M, Marimuthu C, et al. Unusual Presentation of Foreign Body Granuloma of the Foot After Sharp Injury Mimicking a Malignant Lesion: A Case Report. J Foot Ankle Surg 2017;56:1276-8. [Crossref] [PubMed]


