Seasonal and meteorological impacts on primary spontaneous pneumothorax
Introduction
Clustering of primary spontaneous pneumothorax (PSP) is suggested by several studies and now mentioned in the European Respiratory Society guidelines (1-7). However, there is a discrepancy regarding its seasonality; only a few studies have found seasonal variations in the occurrence of PSP (5,8-10). It needs to be taken into account that studies showing no associations between seasons and PSP were conducted for short periods (1,2,6), or in regions with little climatic seasonality (11,12), which might result in underestimating seasonal effects on PSP. Some weather variations, such as decrease in atmospheric pressure and air temperature, increase in wind speed and humidity, and rainfalls, can be risk factors for PSP (1,2,4,6,8-11); however, their effects on the onset of PSP are still controversial (5,11-14). This may be owing to climatic and environmental diversity among study areas.
Based on these considerations, the aims of our study were as follows: (I) to evaluate seasonal differences in the occurrence of PSP, and (II) to assess meteorological risk factors for PSP. We conducted 6-year survey in southern Japan, which has four distinct seasons with appreciable weather changes.
Methods
This study was conducted using a retrospective design. Fukuoka is the capital city of Fukuoka Prefecture, situated on the northern shore of the Japanese island of Kyushu. The age distribution has been almost identical to that of Japan as a whole, and the industrial structure mainly centers on the tertiary industry (15,16). The air quality is relatively low, with a mean particulate matter less than 2.5 microns in diameter (PM2.5) concentration of 20.3×10−6 g/m3, influenced by trans-boundary air pollutants and local emissions (17,18). There are 17 emergency hospitals including department of respiratory medicine in this city, serving about 1.5 million residents (16,19). Kyushu Central Hospital of the Mutual Aid Association of Public School Teachers is one of these hospitals, serving residents of the southern area of Fukuoka. From April 2007 through March 2013 (2,192 days), 188 patients with spontaneous pneumothorax (SP) were admitted to this hospital. PSP cases who were diagnosed without radiological findings, traumatic pneumothorax and secondary SP cases were excluded. PSP rarely occurs in persons over the age of 40 (20), and there seems to be about 10% of the whole population in Japan aged ≥40 years at risk for secondary SP [e.g., subjects with chronic obstructive pulmonary disease (COPD)] rather than PSP (21,22); thus 78 patients aged ≥40 years were excluded, and the remaining 110 patients were analyzed for the present study. Pulmonary physicians reviewed the patients’ medical records and radiographic images and evaluated the onset of PSP. They also confirmed that none of the patients suffered from traumatic or secondary SP. The demographic and clinical characteristics of the patients are summarized in Table 1. Compatible with the known epidemiology of PSP, the study population was likely to be male and twenties. There was no significant difference between the frequencies of smokers and non-smokers. PSP events (110 cases) were assembled in a single time series, and the number of PSP days and non-PSP days during the observation period were 105 (4.8%) and 2,087 (95.2%), respectively.
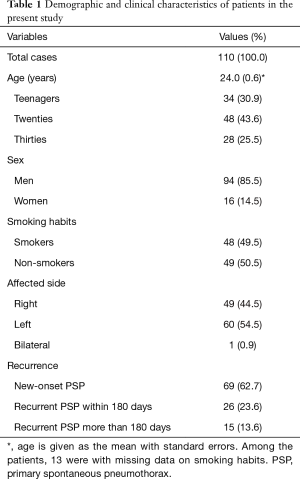
Full table
Daily meteorological parameters, including the mean, maximum, and minimum temperature; mean atmospheric pressure; mean vapor pressure; mean and minimum relative humidity; mean and maximum wind speed; maximum wind gust speed; and precipitation, were obtained from the Japan Meteorological Agency (JMA) (23). A rainy day was defined as a day with >0 mm of precipitation. Table 2 summarizes the meteorological characteristics during the observation period and compares them by season. Significant seasonal variations were found in temperature, atmospheric pressure, vapor pressure, humidity, wind speed, and rainfalls, indicating considerable seasonality in our survey area as we premised. These data were recorded in Fukuoka Regional Headquarters of JMA, located within 5 km of Kyushu Central Hospital of the Mutual Aid Association of Public School Teachers. Daily changes (Δ) in the climatic variables were calculated. Taking into account that exposure to environmental changes such as diving or flying can result in pneumothorax instantly (24,25), intervals between weather changes and PSP occurrence are likely to be short; thus, we assessed the relationship between each meteorological factor and PSP on the same day.
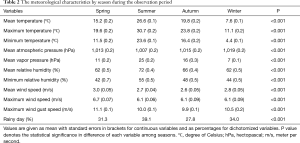
Full table
With regard to calendar variables, holidays were defined as weekends or national holidays in Japan. According to JMA’s classifications, each season was defined as follows: spring, March to May; summer, June to August; autumn, September to November; winter, December to February (26).
Statistical analysis
The SAS software package version 9.3 (SAS Institute, Cary, NC, USA) was used to perform all statistical analyses. A two-sided P<0.05 was considered to indicate statistical significance. Because of the skewed distribution of the maximum wind gust speed and mean and maximum wind speed, these values were log transformed for statistical analysis. Meteorological characteristics were summarized by seasons. Data were compared among seasons using an analysis of covariance (ANCOVA) for continuous variables or a Chi-square test. We calculated the incidence rates of PSP among residents in southern Fukuoka aged <40 years by sex using the person-year method, and adjusted them for the age distribution of the world standard population aged <40 years (27) using the direct method. The frequency of PSP days was estimated separately for each season. The heterogeneity of frequencies among seasons was assessed using a Chi-square test. The heterogeneity was also estimated using a multivariable-adjusted logistic regression model, wherein adjustment was made for other calendar variables, including seasons, months, fiscal years, days of the week, and holidays. In the same way, frequencies and their heterogeneity were also estimated for each month, fiscal year, and day of the week, as well as for business days and holidays. The association of each meteorological factor with PSP days was estimated separately as an odds ratio (OR) with 95% confidence intervals (95% CIs) in a logistic regression model. We also performed multivariate logistic regression analyses to control for previously mentioned risk factors, with adjustments for mean atmospheric pressure (2,4,6,9), mean temperature (1,8,9,11), mean wind speed (6,8), mean relative humidity (11), and rainy days (11). In sensitivity analyses, we limited the PSP case pool to (I) PSP events that were not recurrent on the same side within 180 days, (II) new-onset PSP events to exclude recurrent PSP episodes that might occur due to insufficient recovery from previous events, (III) PSP events in smokers, and (IV) PSP events in non-smokers. In addition, we assessed the relationships between the meteorological factors or their daily changes and PSP on the next day using logistic regression models.
Ethical considerations
The study was approved by the Kyushu Central Hospital of the Mutual Aid Association of Public School Teachers Institutional Review Board for Clinical Research (#270317-76).
Results
Table 3 summarizes the meteorological characteristics during the observation period and compares them between PSP and non-PSP days. Significant variations were found in Δmean wind speed and Δmaximum wind speed. There was no significant difference in other variables.
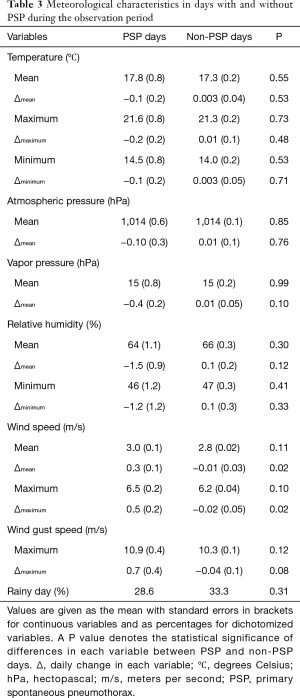
Full table
The incidence rates of PSP were 16.7 per 100,000 person-years in men and 2.1 per 100,000 person-years in women, and the age-adjusted ones were 15.9 and 2.2 per 100,000 person-years in men and women, respectively.
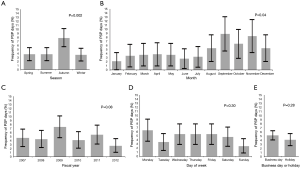
The frequency of PSP days was significantly different among months and seasons with a peak in September and autumn, respectively (Figure 1). After adjusting for other calendar factors, the significant associations of seasons with PSP remained (P=0.03), whereas those of months disappeared (P=0.06). There was no statistical difference in the frequency of PSP days among fiscal years or days of the week, or between business days and holidays.
In univariate analyses, there were significant positive associations of the Δmean wind speed and Δmaximum wind speed with PSP days [crude OR =1.20 (95% CI: 1.02–1.39) per 1 m/s, P=0.02, and crude OR =1.11 (95% CI: 1.02–1.21) per 1 m/s, P=0.02, respectively]. The Δmaximum wind speed was marginally associated with PSP even after adjustment for other meteorological variables [adjusted OR =1.11 (95% CI: 1.00–1.23) per 1 m/s, P=0.05], whereas the association between the Δmean wind speed and PSP did not reach statistical significance after adjustment [adjusted OR =1.19 (95% CI: 0.98–1.46) per 1 m/s, P=0.09]. It should be noted that PSP days were not significantly associated with any wind speed variables or their daily changes on the previous day. There were no associations of other factors with PSP days (Table 4). Similar results were obtained when sensitivity analyses were performed that excluded early recurrent PSP episodes or included only new-onset ones. The results were also similar in analyses using PSP events only in smokers; meanwhile, the associations between changes in wind speed and PSP diminished among PSP in non-smokers.

Full table
Discussion
In the present study, the frequency of days with PSP was 4.8% during the observation period, and the age-adjusted incidence rates of PSP were 15.9 and 2.2 per 100,000 person-years in men and women, respectively. Significant seasonal variations with a peak in autumn were observed in the frequency of PSP days. There was a significant positive association between the Δmaximum wind speed and PSP days. Similar results were obtained when excluding early recurrent PSP episodes or including only new-onset ones.
In the current study, PSP was found to be most likely to occur in autumn, despite sparse earlier evidence showing seasonality in PSP occurrence (5,8,9). As previous studies have mentioned, seasonal differences in PSP occurrence might be related somewhat to climate change (3,28) and/or the recrudescence of respiratory infections (2,29). The inconsistency of PSP seasonality across studies may be due to meteorological, environmental, and geographic differences among studies.
There has been no survey evaluating the incidence of PSP in a general Japanese population using the person-year method. Outside Japan, the incidence rates of PSP were reported as 7.4–24 per 100,000 person-years in men and 1.2–9.8 per 100,000 person-years in women (30-32). These data were in accord with the present results, suggesting that there was little difference in the incidence of PSP among races.
To the best of our knowledge, only two studies showed a positive association between wind speed and PSP occurrence (6,8). This positive relationship was considered to be due to instability of atmospheric pressure in the previous studies (6,33). However, the association of atmospheric pressure with PSP was not substantiated in the current study, as in several reports (1,5,8-11,13,34). Atmospheric pressure change seems too small to cause PSP and likely not a relevant factor triggering PSP (35). Rather, increase in wind speed can induce increase in inhalational exposure to pollen, allergens and air pollutants (36), leading to bronchiolar spasms and air trapping inside the blebs or bullae with a check valve mechanism (3,6,33). Perturbations in wind speed, rather than wind speed itself, cause dispersion of aerosol and drive atmospheric instability (37-39); this may be why variations in wind speed were associated with PSP in the present study. The relationship between changes in wind speed and PSP remained significant when including PSP events in smokers, whereas it diminished among PSP in non-smokers. This heterogeneity is likely because smokers are more sensitive to the effects of variations in wind speed on PSP than non-smokers, since smoking causes bullous diseases (7). On the other hand, there was no relationship between other meteorological factors and PSP occurrence. These associations warrant further evaluation, since previous epidemiologic studies showed that climatic variation is a risk factor for developing PSP (3,5,7).
The present study has several strengths, including the high accuracy of PSP diagnoses achieved by scrutinizing medical records and radiographic images of each patient and the use of huge amounts of meteorological data with various factors obtained from JMA to assess detailed local climatic variations. However, there are some limitations to be considered. First, since the study was designed as a single-center analysis, the present outcomes might lack external validity and generalizability. However, the participating hospital is available 24/7/365 for patients. Supporting this, there was neither heterogeneity in PSP occurrence among fiscal years or days of the week, nor did holidays affect PSP occurrences. Hence, we have no reason to believe that the sample design of the present survey created substantial bias. Second, the number of PSP days in our study was relatively small. It was not large enough to adjust all the meteorological factors in multivariable logistic regression analyses, although the association of the Δmaximum wind speed with PSP days was robust after adjusting for potentially confounding factors. To overcome these limitations and verify the present findings, planning a multicenter prospective cohort study is underway.
In conclusion, PSP tends to cluster seasonally. Increasing wind speeds may play a role, at least in part, in the development of PSP. When wind speeds are higher than the day before, clinicians should be aware of the potential for emerging PSP clusters and be ready to accept PSP patients. The present analysis may contribute to better cost effectiveness of PSP management, although prospective studies are needed to clarify the etiology of rupture of blebs or bullae that cause PSP.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the institutional review board of Kyushu Central Hospital of the Mutual Aid Association of Public School Teachers (#270317-76) and informed consent was not obtained because it was a survey-based retrospective study.
References
- Smit HJ, Devillé WL, Schramel FM, et al. Atmospheric pressure changes and outdoor temperature changes in relation to spontaneous pneumothorax. Chest 1999;116:676-81. [Crossref] [PubMed]
- Alifano M, Parri SNF, Bonfanti B, et al. Atmospheric pressure influences the risk of pneumothorax: beware of the storm! Chest 2007;131:1877-82. [Crossref] [PubMed]
- Smit HJ, Devillé WL, Schramel FM, et al. Spontaneous pneumothorax: predictable mini-epidemics? Lancet 1997;350:1450. [Crossref] [PubMed]
- Scott GC, Berger R, McKean HE. The role of atmospheric pressure variation in the development of spontaneous pneumothoraces. Am Rev Respir Dis 1989;139:659-62. [Crossref] [PubMed]
- Suarez-Varel MM, Martinez-Selva MI, Llopis-Gonzalez A, et al. Spontaneous pneumothorax related with climatic characteristics in the Valencia area (Spain). Eur J Epidemiol 2000;16:193-8. [Crossref] [PubMed]
- Schieman C, Graham A, Gelfand G, et al. Weather and chinook winds in relation to spontaneous pneumothoraces. Can J Surg 2009;52:E151-5. [PubMed]
- Tschopp JM, Bintcliffe O, Astoul P, et al. ERS task force statement: diagnosis and treatment of primary spontaneous pneumothorax. Eur Respir J 2015;46:321-35. [Crossref] [PubMed]
- Bertolaccini L, Alemanno L, Rocco G, et al. Air pollution, weather variations and primary spontaneous pneumothorax. J Thorac Dis 2010;2:9-15. [PubMed]
- Zhang GJ, Gao R, Fu JK, et al. Climatic conditions and the onset of primary spontaneous pneumothorax: an investigation of the influence of solar terms. Med Princ Pract 2012;21:345-9. [Crossref] [PubMed]
- Abul Y, Karakurt S, Bostanci K, et al. Spontaneous pneumothorax and ozone levels: is there a relation? Multidiscip Respir Med 2011;6:16-9. [Crossref] [PubMed]
- Chen CH, Kou YR, Chen CS, et al. Seasonal variation in the incidence of spontaneous pneumothorax and its association with climate: a nationwide population-based study. Respirology 2010;15:296-302. [Crossref] [PubMed]
- Ayed AK, Bazerbashi S, Ben-Nakhi M, et al. Risk factors of spontaneous pneumothorax in Kuwait. Med Princ Pract 2006;15:338-42. [Crossref] [PubMed]
- Bulajich B, Subotich D, Mandarich D, et al. Influence of atmospheric pressure, outdoor temperature, and weather phases on the onset of spontaneous pneumothorax. Ann Epidemiol 2005;15:185-90. [Crossref] [PubMed]
- Haga T, Kurihara M, Kataoka H, et al. Influence of weather conditions on the onset of primary spontaneous pneumothorax: positive association with decreased atmospheric pressure. Ann Thorac Cardiovasc Surg 2013;19:212-5. [Crossref] [PubMed]
- Current Population Estimates. Tokyo: Statistics Bureau, Ministry of Internal Affairs and Communications. Available online: http://www.stat.go.jp/english/data/jinsui/2.htm
- Fukuoka City. Fukuoka: Fukuoka City Government. Available online: http://www.city.fukuoka.lg.jp/english/index.html
- Takami A, Miyoshi T, Irei S, et al. Analysis of organic aerosol in Fukuoka, Japan using a PMF method. Aerosol Air Qual Res 2016;16:314-22. [Crossref]
- Michikawa T, Ueda K, Takeuchi A, et al. Coarse particulate matter and emergency ambulance dispatches in Fukuoka, Japan: a time-stratified case-crossover study. Environ Health Prev Med 2015;20:130-6. [Crossref] [PubMed]
- Emergency information. Fukuoka: Fukuoka Fire Prevention Bureau. Available online: http://119.city.fukuoka.lg.jp/kyukyu/taisei/byouin.html
- Sahn SA, Heffner JE. Spontaneous pneumothorax. N Engl J Med 2000;342:868-74. [Crossref] [PubMed]
- Fukuchi Y, Nishimura M, Ichinose M, et al. COPD in Japan: the Nippon COPD Epidemiology study. Respirology 2004;9:458-65. [Crossref] [PubMed]
- Matsumoto K, Seki N, Fukuyama S, et al. Prevalence of asthma with airflow limitation, COPD, and COPD with variable airflow limitation in older subjects in a general Japanese population: the Hisayama Study. Respir Investig 2015;53:22-9. [Crossref] [PubMed]
- National climate database. Tokyo: Japan Meteorological Agency. Available online: http://www.data.jma.go.jp/gmd/risk/obsdl/index.php
- Raymond LW. Pulmonary barotrauma and related events in divers. Chest 1995;107:1648-52. [Crossref] [PubMed]
- Dermksian G, Lamb LE. Spontaneous pneumothorax in apparently healthy flying personnel. Ann Intern Med 1959;51:39-51. [Crossref] [PubMed]
- Overview of Japan’s climate. Tokyo: Japan Meteorological Agency. Available online: http://www.data.jma.go.jp/gmd/cpd/longfcst/en/tourist_japan.html
- Ahmad OB, Boschi-Pinto C, Lopez AD, et al. Age standardization of rates: a new WHO standard. Geneva: World Health Organization, 2001.
- Ozpolat B. Is the onset of spontaneous pneumothorax influenced by air pollution meteorological changes, or both? J Thorac Dis 2010;2:1-4. [PubMed]
- Bobbio A, Dechartres A, Bouam S, et al. Epidemiology of spontaneous pneumothorax: gender-related differences. Thorax 2015;70:653-8. [Crossref] [PubMed]
- Melton LJ, Hepper NG, Offord KP. Incidence of spontaneous pneumothorax in Olmsted County, Minnesota: 1950 to 1974. Am Rev Respir Dis 1979;120:1379-82. [PubMed]
- Bense L, Eklund G, Wiman LG. Smoking and the increased risk of contracting spontaneous pneumothorax. Chest 1987;92:1009-12. [Crossref] [PubMed]
- Gupta D, Hansell A, Nichols T, et al. Epidemiology of pneumothorax in England. Thorax 2000;55:666-71. [Crossref] [PubMed]
- Bertolaccini L, Viti A, Boschetto L, et al. Analysis of spontaneous pneumothorax in the city of Cuneo: environmental correlations with meteorological and air pollutant variables. Surg Today 2015;45:625-9. [Crossref] [PubMed]
- Obuchi T, Miyoshi T, Miyahara S, et al. Does pneumothorax occurrence correlate with a change in the weather? Surg Today 2011;41:1380-4. [Crossref] [PubMed]
- Bertolaccini L, Cassardo C, Viti A, et al. The relationship between meteorological variations and the onset of spontaneous pneumothorax. Surg Today 2013;43:345-6. [Crossref] [PubMed]
- D’Amato G, Pawankar R, Vitale C, et al. Climate change and air pollution: effects on respiratory allergy. Allergy Asthma Immunol Res 2016;8:391-5. [Crossref] [PubMed]
- Megaritis AG, Fountoukis C, Charalampidis PE, et al. Linking climate and air quality over Europe: effects of meteorology on PM2.5 concentrations. Atmos Chem Phys 2014;14:10283-98. [Crossref]
- Jacob DJ, Winner DA. Effect of climate change on air quality. Atmos Environ 2009;43:51-63. [Crossref]
- Aksoyoglu S, Keller J, Barmpadimos I, et al. Aerosol modelling in Europe with a focus on Switzerland during summer and winter episodes. Atmos Chem Phys 2011;11:7355-73. [Crossref]


