Diagnosis of the cause of chronic dyspnoea in primary and tertiary care: characterizing diagnostic confidence
Introduction
Chronic dyspnoea (breathlessness) is an important and common symptom in primary and tertiary care. Dyspnoea is defined by the American Thoracic Society as “a subjective experience of breathing discomfort that consists of qualitatively distinct sensations that vary in intensity” (1) and is classified as chronic when present for at least eight weeks. The estimated prevalence of chronic dyspnoea ranges from 15% to 60% in patients presenting to general practice (GP), depending on study parameters and population characteristics (2).
The complexity of diagnostic work-up of chronic dyspnoea is a barrier to timely and accurate diagnosis (3,4). Chronic dyspnoea is largely due to respiratory or cardiac causes. However, other causes include metabolic and neurogenic conditions, anaemia and deconditioning (5,6), and multiple aetiologies can coexist in an individual (5,7). In primary care surveys, up to 12% of patients with chronic dyspnoea had no definitive aetiology identified, even with comprehensive evaluation (8-10). A number of clinical diagnostic algorithms—comprising history taking, physical examination, simple investigations (e.g., spirometry, ECG, chest X-ray, blood tests) and more complex investigations—have been piloted but not yet extensively validated in clinical practice (5,7,10-13).
To address these gaps, we studied the diagnostic process experienced by patients with chronic dyspnoea, who were referred from GP and other settings to either cardiology or respiratory specialist clinics at our tertiary referral hospital. The primary aims were to: (I) determine the proportion of patients who had a cause of chronic dyspnoea that was initially clearly evident to the referring doctor; (II) determine the proportion of patients referred with chronic dyspnoea who ultimately received a final diagnosis in the cardiology or respiratory specialist clinics at 6 months after referral; and (III) determine the consistency between the referring doctor’s diagnosis and the specialist diagnosis clinic diagnosis at 6 months after referral. Secondary aims were to: (I) determine whether multifactorial causes of chronic dyspnoea were more difficult to diagnose; (II) observe the effect of initially clearly evident diagnoses on the number of investigations performed, diagnostic concordance and other parameters; and (III) test the accuracy of diagnosis based on body system affected (cardiovascular versus respiratory systems) rather than specific presenting complaints.
Methods
Study design
We conducted a retrospective, observational study which screened patient referrals to specialist outpatient cardiology and respiratory clinics at The Prince Charles Hospital (TPCH), a major tertiary referral hospital in Brisbane. Low/negligible risk institutional ethics approval was granted by the TPCH HREC (HREC/15/QPCH/197) and UQ MREC (2016000222), with Public Health Act approval RD006005.
Study population
Referral letters for patients with chronic dyspnoea, received during May and June 2015 from GPs and other specialist clinics, were screened. Inclusion criteria were adult patients with either (I) chronic dyspnoea as a primary symptom (with chronic defined as greater than eight weeks duration); (II) a condition where chronic dyspnoea is likely to occur and is stated as the primary cause of concern [e.g., chronic obstructive pulmonary disease (COPD), asthma, congestive cardiac failure (CCF) and bronchiectasis]; or (III) new onset or worsening chronic dyspnoea as the primary presenting complaint, with new onset chronic dyspnoea defined as previously undiagnosed or recently diagnosed (defined as within eight months).
Exclusion criteria were: other symptoms as the primary presenting complaint, even if dyspnoea was present but a secondary concern; if the presentation was of an acute or emergent nature; explicit statements suggesting dyspnoea was not present; patients with insufficient documentation in the referral letter for adequate categorization or being an existing patient of a cardiology or respiratory clinic at TPCH or another centre.
Data collection
Data were collected from each patient’s initial referral letter and from the subsequent specialist clinic letters during the 6-month period after the referral date. Data were securely stored in a custom-designed FileMakerPro database. The following variables were extracted: demographics, presenting complaint to primary care, medical history, physical examination findings, results of relevant investigations performed, additional referrals made to other specialists, and provisional and differential diagnoses.
Data analysis
Evident or non-evident diagnosis at time of referral
Each referred patient was categorized as having an evident diagnosis or non-evident diagnosis of chronic dyspnoea, based on the initial referral letter. A patient was considered to have a diagnosis that was evident (i.e., definite or clear) when the referring doctor, in their opinion, confidently stated a provisional diagnosis (e.g., ‘please see for dyspnoea due to COPD’), provided a detailed description of a definite diagnosis with strong aetiological association and/or determined by two investigators to confidently suggest a provisional diagnosis. All other referred patients were considered to have diagnoses that were non-evident. This included when a provisional diagnosis was not stated, or when a possible or list of possible differential diagnosis was provided but an actual diagnosis was not confidently stated. For internal validity, two investigators independently reviewed and classified patients using these criteria.
Concordance between provisional diagnosis and final diagnosis
An analysis was made comparing concordance between the provisional (initial) diagnosis made by the referring doctor and the final diagnosis made by the specialist clinic at 6 months after referral. For each patient, the level of concordance was categorized as: (I) fully concordant: the final diagnosis completely agreed with the provisional diagnosis, (II) partially concordant: incomplete agreement between final diagnosis and the provisional diagnosis, or (III) non-concordant: no agreement between the final and provisional diagnosis. If multiple provisional or final diagnoses contributed to the patient’s presentation, these were each compared individually, and only categorized as fully concordant if either all diagnoses matched (e.g., a patient referred with CCF and COPD and diagnosed by the specialist with CCF and COPD) or if no diagnosis was reached (e.g., a patient referred with no diagnosis, and then no diagnosis was reached by the specialist). Partial concordance was reserved for situations where multiple diagnoses were recognised by one service, whilst fewer, more or a mismatch of diagnoses were identified by the other (e.g., a patient referred with only CCF and diagnosed by the specialist to have CCF and COPD).
Additional comparisons
The categorization of a diagnosis as evident or non-evident (at referral level), referred to as diagnostic confidence, was compared to the level of concordance between the provisional and final diagnoses. Final diagnoses (at specialist level) were categorized as certain, uncertain or no diagnosis, and this was referred to as diagnostic certainty. Evident diagnosis/non-evident diagnosis and concordance were also compared with the variety of investigations performed, abnormalities identified in investigations, the clinic to which the patient was referred (cardiology or respiratory), number of clinic visits attended and whether multiple final diagnoses were present (and if so, number of diagnoses).
Referral appropriateness was ascertained, based on whether the patient’s final diagnosis (or at least one of the final diagnoses) was appropriate for the clinic (cardiology or respiratory) to which the patient had been referred. A patient’s referral was classified as appropriate when the patient’s final diagnoses matched the clinics to which they were referred (e.g., a patient with COPD referred to respiratory and not to cardiology. If they had both CCF and COPD, then a referral to both cardiology and respiratory would be required). Referral was categorized as partially appropriate where at least one appropriate referral had been made but insufficiently covered any other condition the patient may have had (e.g., a patient with COPD and CCF referred only to respiratory). Referrals were classified as inappropriate when there was no match between patient’s final diagnoses and the clinic referred.
Statistical analysis was undertaken using SPSS Version 22 (IBM Corporation, New York, USA). Pearson chi-squared tests were used for univariate analysis of categorical data and Fisher’s exact test was used if data had an expected count less than five. Independent samples t-tests were used for analysis of continuous variables, incorporating Levene’s test for equality of variance. A one-way analysis of variance (ANOVA) test was conducted for three or more independent groups, together with post-hoc tests. A P value of less than 0.05 (two-tailed) was considered statistically significant.
Results
Patients
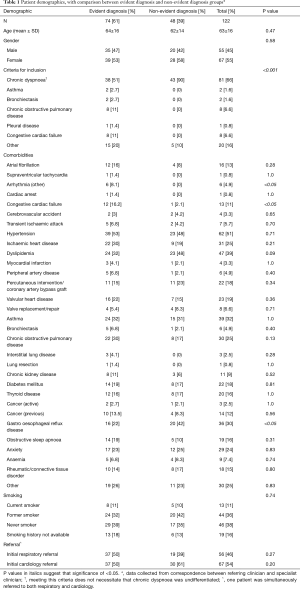
Of 1,370 patients referred to the cardiology and respiratory specialist clinics during the study timeframe, 122 patients who were referred with chronic dyspnoea met the inclusion criteria and were analysed further (Table 1). The patients were primarily from an older population with multiple comorbidities. One hundred and five (86%) were referred from primary care and 17 (14%) were from other specialist clinics in the hospital (cardiology, thoracic medicine, cardiothoracic surgery and internal medicine). Fifty-four percent of patients were initially referred to cardiology clinics and 46% to respiratory clinics. In the majority of referrals (66%), chronic dyspnoea was stated as a presenting issue, with the next most common presentation being COPD (7%) and CCF (7%) (Table 1).
Full table
Evident and non-evident diagnoses at time of referral
Review of referral letters found that 74 (61%) patients had an evident diagnosis from their referring doctor, whereas 48 (39%) had a non-evident diagnosis (Table 1). There were no significant differences in age or gender between these categories. The vast majority (90%) of non-evident diagnoses met inclusion criteria (I) where chronic dyspnoea was the stated reason for referral. However, only 51% of evident diagnoses mentioned chronic dyspnoea (P<0.001). There were no significant differences in prevalence of coexisting medical conditions demonstrated between non-evident diagnoses and evident diagnoses, except for the presence of arrhythmias, CCF or gastro-oesophageal reflux disease (Table 1). There were no significant differences in smoking history nor the initial referral clinic (cardiology or respiratory) between non-evident diagnoses and evident diagnoses.
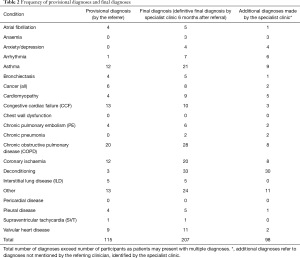
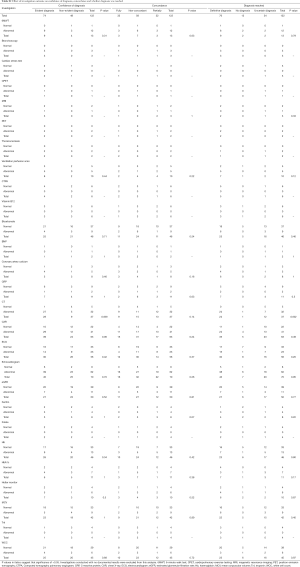
Final diagnoses
A definitive final diagnosis, at 6 months after referral to the specialist clinic, was reached in 62% of patients presenting with chronic dyspnoea, whereas no diagnosis or an uncertain diagnosis remained in 38% of patients at that point in time (Table 2). No significant association was found between the referral confidence of a diagnosis (evident diagnosis versus non-evident diagnosis) and whether a final diagnosis was reached. Table 3 shows the frequency of provisional diagnoses provided by the referring clinician, compared to the frequency of final diagnoses provided by the specialist clinic. There were 92 additional diagnoses identified by specialists compared to the referring clinician, 30 being related to deconditioning. At the time of analysis of specialist clinic letters (6 months after referral), 19 patients were awaiting investigations, 43 were awaiting further review in the specialist clinic, and 10 had been referred to other specialties.
Full table
Full table
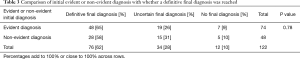
Concordance between provisional and final diagnosis
When comparing the provisional referral diagnosis and final specialist clinic diagnosis at 6 months after referral, 26% of patients had fully concordant diagnoses, 26% partially concordant and 48% non-concordant (Table 4). Evident diagnoses were more likely than non-evident diagnoses to show concordance between provisional and final diagnoses (P<0.001), with 35% of evident diagnoses being fully concordant compared to the 13% of non-evident diagnoses. Conversely, 85% of non-evident diagnoses were non-concordant, compared to 23% of evident diagnoses.

Full table
Appropriateness of referral to a cardiology or respiratory clinic
Appropriate referral to a respiratory or cardiology clinic was assessed by observing the match between the patient’s final diagnoses and the clinic to which the patient was referred. Fifty-one percent of patients were appropriately referred, 39% partially appropriately referred and 11% of patients were referred to an inappropriate specialist clinic (Table 5). There was no significant association between the referring confidence of a diagnosis and appropriateness of referral.

Full table
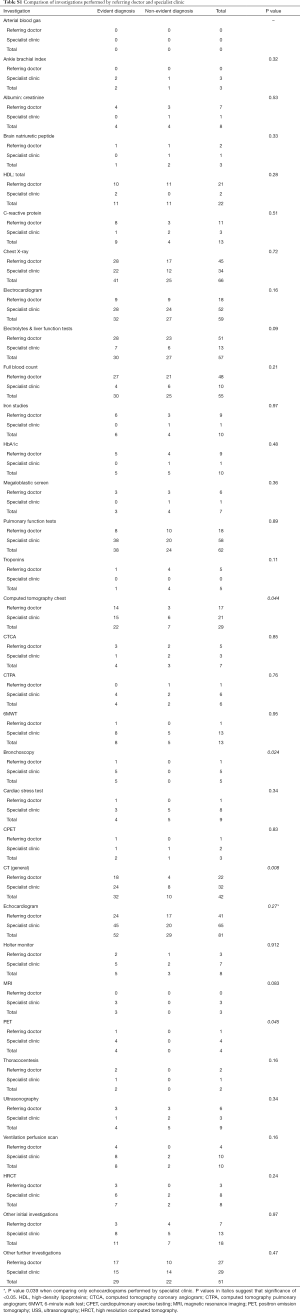
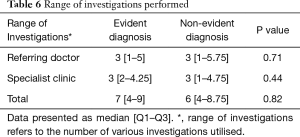
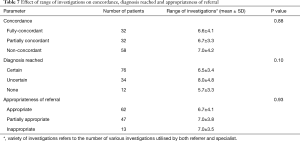
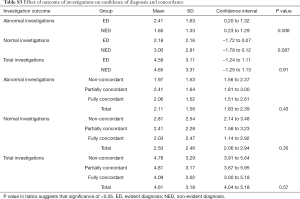
Investigations
The list of investigations performed is shown in Table S1. No statistically significant differences were observed between evident diagnoses and non-evident diagnoses, for the range of investigations performed for the workup of chronic dyspnoea (Table 6), concordance rates, referral to the appropriate clinic or whether a final diagnosis was reached (Table 7). The majority of chest CT scans were performed in patients with evident diagnoses and of these, nearly all were found to be abnormal, leading to a greater chance of reaching a final diagnosis. For other investigations, there was no significant correlation between whether an abnormal investigation was found and the confidence of a diagnosis or whether a diagnosis was reached (Tables S1-S3).
Full table
Full table
Full table
Full table
Full table
Number of diagnoses and multifactorial causes of chronic dyspnoea
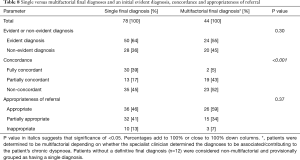
A single final diagnosis of chronic dyspnoea was more common than multifactorial final diagnoses (Table 8). There were no statistically significant differences in frequency of single or multifactorial causes between evident diagnoses and non-evident diagnoses (Table 8). The mean number of diagnoses for patients with partially-concordant diagnoses was significantly higher than for patients with fully concordant and non-concordant diagnoses (P<0.001) (Table 9). A significant association was found between concordance and whether there was a multifactorial diagnosis (P<0.001). Single final diagnoses were more likely to be concordant, although there was still a high prevalence of partial or non-concordance (Table 8). Few of the patients with multifactorial causes for their chronic dyspnoea demonstrated concordance. No significant association was found between the presence of a multifactorial diagnosis and appropriateness of referral (Table 8).
Full table

Full table
Clinic visits
There was no statistically significant difference in concordance, evident diagnosis versus non-evident diagnosis status, or whether a final diagnosis was reached, based on the number of clinic visits attended during the study period (data not shown).
Discussion
Main findings
The primary outcome of this study was to determine the degree of difficulty in the diagnosis of the cause of chronic dyspnoea in patients referred from primary care to cardiac or respiratory specialist clinics in tertiary care. Thirty-nine percent of patients did not have an evident diagnosis of the cause of the chronic dyspnoea stated in the referral letter, indicating a high degree of diagnostic difficulty in this referred cohort. Full concordance between the initial diagnosis stated by the referrer and the final specialist clinic diagnosis at 6 months after referral was present in only 26% of patients. However, full or partial concordance was found in 52%. At 6 months after referral to a specialist clinic, a definitive final diagnosis had been reached in only 62% of patients, whilst 28% still had an uncertain diagnosis, and 10% had no final diagnosis reached. The range of investigations ordered was not associated with diagnostic confidence, concordance between provisional and final diagnoses, or appropriateness of referral to cardiology or respiratory clinics. These results demonstrate the considerable complexities that occur in the diagnosis of the aetiology of chronic dyspnoea in both primary care and tertiary care.
Confidence of initial diagnoses
To our knowledge, this is the first study to critically analyse the patient referral letter, in order to ascertain the degree of diagnostic confidence of the referrer. Our study revealed a relatively high frequency of patients referred with chronic dyspnoea in which the diagnosis was not initially clearly evident to the referrer (non-evident diagnosis). This reflects the considerable proportion of patients referred to specialist clinics with a diagnostic problem of determining the actual cause of the dyspnoea, where a diagnosis is required before definitive management can be implemented based on the underlying pathophysiology of the specific condition (14,15). Nevertheless, there were also some patients referred who already had a diagnosis made by the referrer (evident diagnosis), for whom management advice was being sought. As this study retrospectively classified the level of confidence of the referrer in their provisional diagnosis, future prospective validation of diagnostic confidence would be worthwhile.
Success at reaching a final diagnosis
Reaching a timely final diagnosis of the cause of chronic dyspnoea is a complex pathway in some patients. We selected a 6-month timeframe for review of the status of the diagnosis, to allow sufficient time for at least one specialist clinic attendance to have occurred. At that point in time, we observed that the specialist clinic was uncertain of the diagnosis in 38% of patients, and could not identify a final diagnosis in 10% of patients. This is similar to rates found in primary audits (8-10). There was no significant association between the confidence of the provisional diagnosis and the ability of the specialist clinic to reach a definitive diagnosis, indicating that high perceived confidence in the referring diagnosis does not necessarily guarantee that a definitive diagnosis will be reached within 6 months, and vice versa. Although insufficient number of clinic visits attended to make a diagnosis could conceivably be a factor (e.g., with longer waiting times to be seen in the first clinic visit), the number of clinic visits during the study period was not statistically associated with whether a final diagnosis was reached. Another potential reason for the lack of definitive diagnosis is the intrinsic difficulty in patients with multifactorial causes. It would be informative to explore these issues in future studies, extending the follow up time and determining the time required to work up an undifferentiated and/or multifactorial presentation of chronic dyspnoea.
Diagnostic concordance
Improving diagnostic concordance between the referrer and the specialist clinic would enhance timeliness and accuracy of diagnosis, to allow treatment to commence earlier. Our study found a high degree of non-concordance between the provisional (referrer) diagnosis and the final diagnosis by the specialist clinic at 6 months, with over 70% of patients not having a fully concordant diagnosis, including 48% of patients with completely non-concordant diagnoses. A high degree of non-concordance between initial and final diagnoses was reported in a previous study, in which over 60% of patients eventually had a non-concordant diagnosis (7). In our study, patients with evident diagnoses made by the referrer demonstrated a significantly higher proportion of fully and partially-concordant diagnoses (77%) compared to non-evident diagnoses (15%), suggesting that the higher the certainty of the initial provisional diagnosis, the more likely that the diagnosis is accurate. However, this is not an absolute relationship, since diagnostic non-concordance was frequent even among those referred with high diagnostic confidence. Factors that may increase the diagnostic accuracy of the provisional diagnosis by referrers include classical clinical presentations of typical and common causes of chronic dyspnoea, clear-cut physical findings that indicate a diagnosis, and simple or accessible investigations that lead directly to a single diagnosis. Optimising diagnostic pathways based on these factors should be undertaken in future diagnostic studies.
Appropriateness of referral
Appropriate referral destination would enhance efficiency and reduce time to final diagnosis for patients to chronic dyspnoea. In this study, appropriate or partially appropriate referral was observed in 90% of patients, which was higher than the 64% found in a previous study (7). Referral to the appropriate speciality clinic was not associated with evident diagnosis made by the referrer, indicating that although a specific diagnosis may not be evident, there is still often sufficient information available to the referrer to make a reasonable choice about referral to the appropriate cardiology or respiratory clinic (16). Future studies should determine whether clinical algorithms differentiating cardiac or respiratory features would lead to more efficient diagnostic processes.
Impact of investigations performed
Investigations are helpful for ruling in or ruling out diagnoses suspected after a thorough history and physical examination (16). We hypothesised that an undifferentiated presentation of chronic dyspnoea would lead to a broader diagnostic workup with increased need for specialised investigations. However, no statistically significant association was found between the variety of investigations conducted, compared to diagnostic concordance, appropriateness of referral or ability to reach a final diagnosis. Although these findings may be related to small sample size, our study does suggest that the number of investigations was not found to affect diagnostic ability.
Nevertheless, the relevance of each investigation performed needs to be considered. Spirometry is useful for diagnosing chronic airflow obstruction [and is the defining feature in COPD (17)]; however, abnormal spirometry does not always correlate with the presence of respiratory symptoms, and vice versa (18). Other simple initial diagnostic tests are useful and are commonly performed in chronic and acute dyspnoea [including chest X-ray (19), ECG, blood tests]. In our study, CT chest scans were more often abnormal for evident diagnoses than non-evident diagnoses, especially in GP. Overall, we found abnormal investigation results increased confidence in specific diagnoses, whilst relevant negative findings were less influential. Whilst some clinical algorithms already exist (5,7,10-13), further work needs to be done to formulate a stepwise guideline to the selection of relevant investigations in the diagnostic pathway, and then to overcome barriers to implementation of these clinical guidelines to clinical practice (20).
Multifactorial causes of chronic dyspnoea
Although respiratory and cardiovascular conditions are the most common causes of chronic dyspnoea, multifactorial aetiologies have been reported in up to 40% of patients (7), with similar rates replicated in our study (36%). Multiple causes of chronic dyspnoea in a patient complicated the diagnostic workup, with single diagnoses more likely to be concordant between referrer and specialist clinic in our present study. The number of diagnoses identified was higher in patients with partially concordant diagnoses than those with fully or non-concordant patients, which is understandable since multiple diagnoses increase the difficulty of achieving full concordance. Deconditioning was more frequently identified by the specialist clinic as an additional diagnosis, potentially indicating under-diagnosis of deconditioning in primary care. Consequently, our study demonstrates that the multifactorial nature of the chronic dyspnoea in some patients increases the level of diagnostic complexity, as highlighted by others (21).
Potential limitations
Several potential limitations should be considered. Firstly, we utilized a retrospective method of data collection with data extracted from referral letters, which may not always accurately reflect the referring doctor’s views, depending on how much detail was included in the letter. Nevertheless, this was the level of detail available to the specialist clinic, and the letter is a written indication of the opinions of the referring doctor at the point of referral. Secondly, a proportion of patients were still awaiting investigations or further specialist review at the selected timepoint of 6 months after referral. These patients could have received a definitive final diagnosis given longer follow-up time, and consequently the proportion of patients assigned a final diagnosis may have been underestimated. However, patients and referring clinicians would generally expect that the majority of diagnoses would ideally be made within 6 months of referral. Thirdly, although two independent reviewers assessed the levels of diagnostic confidence and diagnostic concordance, there is potentially a small risk of observer bias. Hence, a prospective observational study, with data collected directly from clinicians, is recommended to confirm our findings, and subsequently develop diagnostic algorithms based on the most efficient and effective pathways to single and multiple diagnoses of the cause(s) of chronic dyspnoea.
Conclusions
This study has identified a considerable degree of difficulty in diagnosing the cause of chronic dyspnoea in adults seen in primary care and tertiary care settings. Over one-third of adult patients referred with chronic dyspnoea to the cardiology or respiratory specialist clinics had diagnoses that were considered uncertain by their referrer. At 6 months after referral, only one-quarter of patients had diagnoses that were fully concordant between referrer and specialist clinic, and one-third of patients still did not have a final definitive diagnosis. Multiple diagnoses were more difficult to definitively diagnose than single diagnoses causing chronic dyspnoea. The number of investigations was not associated with an initial evident diagnosis by the referrer, or concordance of diagnoses between referrer and specialist clinic.
Our findings demonstrate diagnostic complexity of chronic breathlessness in adults, both in primary care and tertiary care. Clinicians should aim to make a diagnosis of the cause of chronic dyspnoea based on history, examination and standard investigations. If this approach does not yield a single evident diagnosis, then referral to the specialty clinic that is considered most appropriate (cardiology or respiratory) should be made, based on the best judgment of the referring clinician. Given the demonstrated complexity of diagnosis of the cause of chronic dyspnoea, the development of an effective and comprehensive diagnostic algorithm for chronic dyspnoea is recommended, to improve current standards of care.
Acknowledgements
We thank the patients and staff of The Prince Charles Hospital, and the referring doctors, for their contribution to this study. We appreciate the statistical advice from Dr. Karen Hay, QIMR Berghofer biostatistician.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Low/negligible risk institutional ethics approval was granted by the TPCH HREC (HREC/15/QPCH/197) and UQ MREC (2016000222), with Public Health Act approval RD006005.
References
- American Thoracic Society. Dyspnea. Am J Respir Crit Care Med 1999;159:321-40. [Crossref] [PubMed]
- Johnson MJ, Currow DC, Booth S. Prevalence and assessment of breathlessness in the clinical setting. Expert Rev Respir Med 2014;8:151-61. [Crossref] [PubMed]
- Schmitt BP, Kushner MS, Wiener SL. The diagnostic usefulness of the history of the patient with dyspnea. J Gen Intern Med 1986;1:386-93. [Crossref] [PubMed]
- Kjellström B, van der Wal MH. Old and new tools to assess dyspnea in the hospitalized patient. Curr Heart Fail Rep 2013;10:204-11. [Crossref] [PubMed]
- Pratter MR, Abouzgheib W, Akers S, et al. An algorithmic approach to chronic dyspnea. Respir Med 2011;105:1014-21. [Crossref] [PubMed]
- Wahls SA. Causes and evaluation of chronic dyspnea. Am Fam Physician 2012;86:173-82. [PubMed]
- Nielsen LS, Svanegaard J, Wiggers P, et al. The yield of a diagnostic hospital dyspnoea clinic for the primary health care section. J Intern Med 2001;250:422-8. [Crossref] [PubMed]
- Currow DC, Clark K, Mitchell GK, et al. Prospectively collected characteristics of adult patients, their consultations and outcomes as they report breathlessness when presenting to general practice in Australia. PLoS One 2013;8. [Crossref] [PubMed]
- Charles J, Ng A, Britt H. Presentations of shortness of breath in Australian general practice. Aust Fam Physician 2005;34:520-1. [PubMed]
- Pedersen F, Mehlsen J, Raymond I, et al. Evaluation of dyspnoea in a sample of elderly subjects recruited from general practice. Int J Clin Pract 2007;61:1481-91. [Crossref] [PubMed]
- Karnani NG, Reisfield GM, Wilson GR. Evaluation of chronic dyspnea. Am Fam Physician 2005;71:1529-37. [PubMed]
- DePaso WJ, Winterbauer RH, Lusk JA, et al. Chronic dyspnea unexplained by history, physical examination, chest roentgenogram, and spirometry. Analysis of a seven-year experience. Chest 1991;100:1293-9. [Crossref] [PubMed]
- Martinez FJ, Stanopoulos I, Acero R, et al. Graded comprehensive cardiopulmonary exercise testing in the evaluation of dyspnea unexplained by routine evaluation. Chest 1994;105:168-74. [Crossref] [PubMed]
- Laviolette L, Laveneziana P. ERS Research Seminar Faculty. Dyspnoea: a multidimensional and multidisciplinary approach. Eur Respir J 2014;43:1750-62. [Crossref] [PubMed]
- Mahler DA, O'Donnell DE. Recent advances in dyspnea. Chest 2015;147:232-41. [Crossref] [PubMed]
- Kaplan A, Gruffydd-Jones K, van Gemert F, et al. A woman with breathlessness: a practical approach to diagnosis and management. Prim Care Respir J 2013;22:468-76. [Crossref] [PubMed]
- Yang IA, Brown JL, George J, et al. COPD-X Australian and New Zealand guidelines for the diagnosis and management of chronic obstructive pulmonary disease: 2017 update. Med J Aust 2017;207:436-42. [Crossref] [PubMed]
- Marcus BS, McAvay G, Gill TM, et al. Respiratory symptoms, spirometric respiratory impairment, and respiratory disease in middle-aged and older persons. J Am Geriatr Soc 2015;63:251-7. [Crossref] [PubMed]
- Cardinale L, Volpicelli G, Lamorte A, et al. Revisiting signs, strengths and weaknesses of Standard Chest Radiography in patients of Acute Dyspnea in the Emergency Department. J Thorac Dis 2012;4:398-407. [PubMed]
- Overington JD, Huang YC, Abramson MJ, et al. Implementing clinical guidelines for chronic obstructive pulmonary disease: barriers and solutions. J Thorac Dis 2014;6:1586-96. [PubMed]
- Berliner D, Schneider N, Welte T, et al. The Differential Diagnosis of Dyspnea. Dtsch Arztebl Int 2016;113:834-45. [PubMed]


