Large left main coronary artery aneurysm with fistula to the right atrium
Introduction
Coronary artery fistula can present as a rare congenital anomaly or can be formed after chest trauma, repeated insult to the heart by coronary angiography, endomyocardial biopsy (iatrogenic), or may be idiopathic in nature. Left main coronary artery (LMCA) aneurysm combined with LMCA fistulous connection to the right atrium (RA) is an extremely rare finding. Once symptomatic, prompt diagnosis and treatment of this condition is important as undiagnosed condition is associated with serious complications and poor prognosis. Herein we present a case of a large symptomatic LMCA aneurysm with fistulous connection to the RA that was managed surgically.
Case presentation
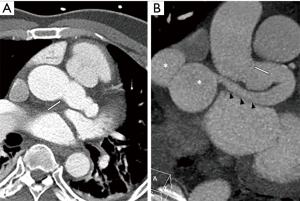
A 54-year-old male with hypertension, type 2 diabetes mellitus, and atrial flutter was referred in 2013 for incidentally found LMCA aneurysm with fistulous connection to the RA. CT angiogram at that time showed a 23 mm LMCA aneurysm with fistulous tract that coursed in the retroaortic region, extending into the interatrial septum and opening into the RA (Figure 1A,B). Cardiac catheterization confirmed the diagnosis (Figure 2). At that time, the patient declined an intervention, was noncompliant with medication, and eventually was lost to follow up. He did have multiple emergency room visits for symptoms of recurrent atrial flutter and evolving heart failure. CT scan in 2017 showed stable LMCA aneurysm. On transthoracic echocardiogram he was noted to have severely decreased systolic left ventricular function (ejection fraction <20%) with global hypokinesis, severe right ventricular (RV) dilatation and dysfunction, and severely dilated RA. Left heart catheterization revealed no obstructive coronary artery disease and a large left to right shunt through the coronary artery fistula. Right heart catheterization revealed moderate-severe elevation of pulmonary capillary wedge pressure (28 mmHg), moderate-severe elevation of RV end-diastolic pressure (20 mmHg), and elevated right atrial pressure (18 mmHg), as well as significant left to right shunt (Qp/Qs =2, right atrial saturation =86%). Magnetic resonance imaging showed viable myocardium and marked left to right shunt with pulmonary-systemic flow ratio (Qp/Qs =2.8). The patient was deemed not a suitable candidate for percutaneous intervention. As part of the operative planning, the anatomic pathology was reconstructed in three dimensions (3D) (Figure 3) and 3D printed.

Intraoperatively, median sternotomy, systemic heparinization, bicaval cannulation, and both antegrade and retrograde cardioplegia was utilized. To be able to administer antegrade cardioplegia, we first opened the RA and occluded the distal fistula opening using 4-0 polypropylene with a tourniquet (Figure 4A). Then, the aorta was cross clamped and cardiac arrest was achieved using cold antegrade cardioplegia followed by retrograde cardioplegia. The LMCA was dissected out to the bifurcation into the circumflex and left anterior descending artery, the origins of which were involved in the aneurysm. Aortotomy was performed and LMCA was opened longitudinally to visualize the origin of the fistula. Three mm coronary probes were used to identify the left coronary orifices and the fistula tract (Figure 4B). The proximal fistula opening was then closed in two layers of 5-0 polypropylene sutures (Figure 4C), and aneurysmorrhaphy was performed with two layers of running 5-0 polypropylene sutures (Figure 4D). A 3 mm coronary probe was passed from the aortotomy to ensure the patency of repaired LMCA. The distal fistula opening in the RA was then closed using multiple pledgetted 4-0 polypropylene sutures. At the conclusion of the surgery, Qp/Qs was 1.07 and no step-up of partial pressure of oxygen (pO2) was noted in the superior vena cava, RA, inferior vena cava and pulmonary artery.

Postoperatively the patient developed sinus node dysfunction with severe left ventricular dysfunction (EF =20–25%) leading to placement of automatic implantable cardioverter-defibrillator on postoperative day 9. Rest of his recovery was unremarkable and he was dismissed on postoperative day 16.
Discussion
LMCA fistula to the RA is a rare finding. Less than 50% of the fistulae originate from the left coronary artery and >90% of them drain into the venous system, the two most common drainage sites being RV and RA (3). In one study that reviewed 10,340 coronary angiograms, 0.18% of patients had coronary artery fistula and 0.02% were found to have left coronary artery to right atrial fistula (4). Coronary fistula coupled with coronary aneurysm is extremely rare, and those with openings more proximal to the main coronary arteries tend to develop more sizeable aneurysms (5). Roughly half of the patients are asymptomatic, however serious complications such as spontaneous rupture, congestive heart failure, bacterial endocarditis or myocardial ischemia may develop (6). Left-to-right shunt through the fistula may cause a “steal” phenomenon manifesting as myocardial ischemia. While general consensus points towards conservative management in asymptomatic patients, large (>4 cm), rapidly growing, or symptomatic coronary artery aneurysm/fistulas require surgical repair and closure (7). Surgical management includes resection of the aneurysm, reconstruction of the coronary artery and repair of fistula (7).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Abbas Rizvi SS, Choi JH, Tchantchaleishvili V, et al. Cardiac catheterization showing the LMCA aneurysm and fistula tract. Asvide 2018;5:588. Available online: http://www.asvide.com/article/view/25565
- Abbas Rizvi SS, Choi JH, Tchantchaleishvili V, et al. 3D reconstruction of the heart and the LMCA aneurysm with fistula tract using 3D Slicer. Asvide 2018;5:589. Available online: http://www.asvide.com/article/view/25566
- Levin DC, Fellows KE, Abrams HL. Hemodynamically significant primary anomalies of the coronary arteries. Angiographic aspects. Circulation 1978;58:25-34. [Crossref] [PubMed]
- Davidavičius G, Šubkovas E, Abraitis V, et al. Coronary anomalies : single centre experience. Semin Cardiol 2004;10:208-13.
- Qureshi SA. Coronary arterial fistulas. Orphanet J Rare Dis 2006;1:51. [Crossref] [PubMed]
- Liberthson RR, Sagar K, Berkoben JP, et al. Congenital coronary arteriovenous fistula. Report of 13 patients, review of the literature and delineation of management. Circulation 1979;59:849-54. [Crossref] [PubMed]
- Zhu Z, Wang Y, Xu R, et al. Giant aneurysm of the left main coronary artery with fistulous communication to the right atrium. J Cardiothorac Surg 2015;10:117. [Crossref] [PubMed]


