Outcomes of patients undergoing surgery for thymic carcinoma: a single-center experience
Introduction
Thymic carcinoma is rare (10–15% of thymic epithelial tumors), typically presents locally at an advanced stage, behaves aggressively, and lymphatic or distant metastases are frequent (1-3). Complete surgical resection is not always possible for patients with advanced-stage thymic carcinoma because of local regional invasion. Limited data are available concerning the outcomes of unusual patients after resection of thymic carcinoma judged potentially resectable, with or without neoadjuvant treatment. We therefore retrospectively reviewed our institutions’ experience with patients with thymic carcinoma.
Methods
Patients
Six patients with thymic carcinoma underwent surgical resection at our hospital from 2006 to 2016. We evaluated the association of outcomes with sex, age, histological classification, Masaoka staging, postoperative treatment, and recurrence. Perioperative death was defined as occurring within 30 days after resection. A complete resection, classified as R0, was defined as the pathological demonstration of negative tissue margins and assessment by the surgeon that all detectable disease was removed. Our institution’s ethics committee approved this study.
Patient follow-up
Patients’ records were reviewed for preoperative symptoms, surgical procedures, and postoperative complications. The patients were examined at 1- or 3-month intervals for ≥5 years. To detect recurrence, we performed physical examinations, routine hematological analyses, chest radiography, computed tomography (CT) of the chest and upper abdomen, magnetic resonance imaging of the brain, and bone scintigraphy.
Results
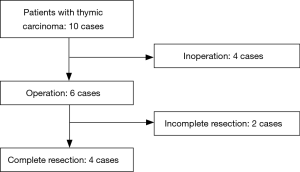
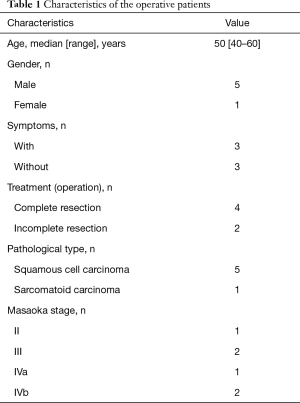
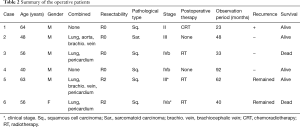
Ten patients with thymic carcinoma underwent total thymectomy, four underwent curative resection, and none received preoperative induction therapy (Figure 1). The clinical characteristics of the six patients with thymic carcinoma (median age, 56 years; five men and one woman) were as follows: squamous cell carcinoma (n=5); sarcomatoid carcinoma (n=1); and Masaoka stages II (n=1), III (n=2), IVa (n=1), and IVb (n=2) (Table 1). A summary of the patients who underwent surgery is shown in Table 2. There was no perioperative death. Four patients underwent combined pulmonary resection (66.7%) as a component of en bloc resection due to suspicion of pulmonary invasion. Four patients (66.7%) received postoperative therapy, and complete resection was achieved for four patients. There were no perioperative deaths. One patient experienced a recurrence. We previously reported patient number 2 (4).
Full table
Full table
We performed complete resection of the thymic sarcomatoid carcinoma, which is extremely rare, through a total aortic arch replacement and left upper lobectomy. Our aggressive surgical procedure was very effective, and the patient remains recurrence-free 4 years after surgery.
Discussion
Thymic carcinoma is uncommon, presents locally at an advanced stage, and behaves aggressively. The optimum treatment for advanced thymic carcinoma is controversial. There are few reports of improved survival of patients who underwent complete resection to treat thymic carcinoma (1). For example, median survival is 24.9 months, and the 5-year survival rate is 42.3%, similar to the respective survival data for 30–50% of patients with thymic carcinomas (5).
Complete resection is useful for treating thymic carcinoma, given the lack of efficacy of chemotherapy and radiotherapy. In present analysis, no patient who underwent complete resection died, and three of four patients remain recurrence-free. Although an inherent limitation of any study of thymic carcinoma is the small number of patients, our findings should nevertheless persuade oncologists to seriously consider offering their patients the option of complete resection.
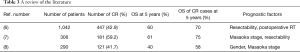
Our review of the literature about the prognosis of thymic carcinoma is shown in Table 3. Ahmad et al. reported that postoperative radiotherapy for patients with thymic carcinoma improves survival (6). The four patients (66.7%) studied here who underwent radiotherapy after surgery did not experience recurrence or regrowth. Moreover, patient number 5 is alive without regrowth more than 5 years after incomplete resection (R2).
Full table
One patient with Masaoka stage III underwent total thymectomy comprising resection of the lung, pericardium, and the left brachiocephalic vein. When postoperative radiotherapy was administered, regrowth was not observed. Therefore, postoperative radiotherapy may be effective when resection is incomplete.
The Masaoka stage has significant prognostic implications (6-8). Patients with advanced thymic carcinoma classified as Masaoka stages II–IV who undergo surgery are offered postoperative radiotherapy Moreover, patients with thymic carcinoma who undergo incomplete resection are offered postoperative chemoradiotherapy. Here, our patient with Masaoka stage II thymic carcinoma underwent postoperative radiotherapy. Some studies report that incomplete surgical resection does not adversely affect long-term survival of patients who are administered postoperative cisplatin-based chemotherapy (9). Furthermore, other studies report that complete resection of a thymic carcinoma significantly increases survival (1,6,7,10,11). The present analyses demonstrate that complete resection achieved improved outcomes.
Conclusions
We conclude that complete resection of thymic carcinoma improved survival outcomes and that oncologists should offer this treatment option to patients, particularly those with advanced disease.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the ethics committee of University of Occupational and Environmental Health (No. H26-15).
References
- Kondo K, Monden Y. Therapy for thymic epithelial tumors: a clinical study of 1,320 patients from Japan. Ann Thorac Surg. 2003;76:878-84; discussion 884-5. [Crossref] [PubMed]
- Marx A, Rieker R, Toker A, et al. Thymic carcinoma: is it a separate entity? From molecular to clinical evidence. Thorac Surg Clin 2011;21:25-31. v-vi. [Crossref] [PubMed]
- Ruffini E, Detterbeck F, Van Raemdonck D, et al. Thymic carcinoma: a cohort study of patients from the European society of thoracic surgeons database. J Thorac Oncol 2014;9:541-8. [Crossref] [PubMed]
- Oka S, Taira A, Shinohara S, et al. Complete Resection of Thymic Sarcomatoid Carcinoma Through Total Aortic Arch Replacement. Ann Thorac Surg 2016;102:e557-9. [Crossref] [PubMed]
- Eng TY, Fuller CD, Jagirdar J, et al. Thymic carcinoma: state of the art review. Int J Radiat Oncol Biol Phys 2004;59:654-64. [Crossref] [PubMed]
- Ahmad U, Yao X, Detterbeck F, et al. Thymic carcinoma outcomes and prognosis: results of an international analysis. J Thorac Cardiovasc Surg 2015;149:95-100, 101.e1-2.
- Hishida T, Nomura S, Yano M, et al. Long-term outcome and prognostic factors of surgically treated thymic carcinoma: results of 306 cases from a Japanese Nationwide Database Study. Eur J Cardiothorac Surg 2016;49:835-41. [Crossref] [PubMed]
- Weksler B, Dhupar R, Parikh V, et al. Thymic carcinoma: a multivariate analysis of factors predictive of survival in 290 patients. Ann Thorac Surg 2013;95:299-303. [Crossref] [PubMed]
- Hernandez-Ilizaliturri FJ, Tan D, Cipolla D, et al. Multimodality therapy for thymic carcinoma (TCA): results of a 30-year single-institution experience. Am J Clin Oncol 2004;27:68-72. [Crossref] [PubMed]
- Tseng YL, Wang ST, Wu MH, et al. Thymic carcinoma: involvement of great vessels indicates poor prognosis. Ann Thorac Surg 2003;76:1041-5. [Crossref] [PubMed]
- Yano M, Sasaki H, Yokoyama T, et al. Thymic carcinoma: 30 cases at a single institution. J Thorac Oncol 2008;3:265-9. [Crossref] [PubMed]