The Six-Minute-Walk Test in assessing respiratory function after tumor surgery of the lung: a cohort study
Introduction
Various functional test procedures are available for the assessment of cardio-pulmonary function and physical capacity. Many of these diagnostic procedures include complex evaluations of both cardiac and pulmonary function, require expensive equipment and are time-consuming. Frequently used functional diagnostic tests include spirometry, spiroergometry, whole-body plethysmography, Shuttle-Walk-Test, Cardiac-Stress-Test and Cardiopulmonary Exercise Test (1,2). Due to limited personal and technical resources in outpatient care as well as in community hospitals and rehabilitation facilities, simple patient surveys of lung function are more likely to be conducted; whereas complex diagnostic tests of cardio-pulmonary are often not feasible.
In 1963 Balke developed an easy to perform test of cardio-pulmonary function: measuring the walking distance in a defined time period (3). The 12-Minute Walking Test has been developed subsequently, which was used to measure the physical capacity in healthy individuals (4). This test has proven unsuitable in subjects with respiratory diseases due to its duration and physical strain. Subsequently the Six-Minute-Walk Test (6-MWT) was developed (5). The 6-MWT is similar to physical activity in daily life, is easier to perform, better tolerated by subjects and represents lung function similar as other more complex cardio-pulmonary tests (6). Moreover, the 6-MWT is potent a predictor of morbidity and mortality in subjects with chronic-obstructive pulmonary disease (COPD) (7). The 6-MWT is an established instrument to assess cardio-pulmonary status and has been used to assess subjects following surgical resections of benign tumors (8-11).
The significance of 6-MWT to determine respiratory function in subjects after surgical resections of malignant tumors is unclear. Moreover, it has no cohort been defined, if in this patient group a correlation between 6-MWT walking distance and lung function parameters such as the forced expiratory volume in one second (FEV1) exists. The aim of the present study is to analyze in a large cohort of subjects, who underwent surgical pulmonary resection of malignant tumors, the 6-MWT walking distance at the beginning and at the end of inpatient rehabilitation and to assess its correlation with concomitantly measured FEV1.
Materials and methods
Subjects
This is a retrospective study of subjects, who received oncological rehabilitation after lung surgery at a single center from April 2010 to July 2010. Inclusion criteria were malignant diseases in the form of non-small cell lung cancer (NSCLC), other histology of primary lung cancer or lung metastases. Exclusion criteria were: subjects’ malignant mesothelioma, subjects’ inability to perform spirometry or the 6-MWT subjects.
Inpatient rehabilitation
The study was designed as a retrospective analysis. All examinations and therapy measures were standard components of oncological rehabilitation. The rehabilitation included aerobics training, breath-therapeutic and physiotherapeutic exercises for the lungs and the muscles of the upper and the lower limb as well as of the auxiliary respiratory muscles. Rehabilitation therapies occurred daily from Monday to Saturday. The participation in the therapies was monitored by using attendance lists. Moreover, subjects were trained with regard to breathing technique and encouraged to perform breathing exercises independently. There was no additional intervention outside of the clinical routine. Both spirometry and 6-MWT were performed at the beginning (T1) as well as at the end (T2) of oncological rehabilitation.
Spirometry
Lung function was examined by measurement of the forced vital capacity FVC (FVC as a percentage of the predicted value) and FEV1 (FEV1 as a percentage of the predicted value), with a commercial spirometer (SpiroPerfect®, Welch Allyn, 4341 State Street Road, PO Box 220, Skaneateles, NY, USA). Spirometry was performed according to the American Thoracic Society recommendations (12). In order to obtain optimal measured values, measurements were done by well-trained technicians and were repeated on each examination. The subjects were coached to optimal performance in a standardized fashion. To assess for and to improve the reproducibility several measurements were carried out by each subject. All spirometric measurements were obtained as pre-bronchodilator tests and no additional broncholytic or other medications with effects on the respiratory system were administered and the examination was performed in conditions of rest.
Six-Minute-Walk Test (6-MWT)
6-MWT was performed according to the guidelines of the American Thoracic Society (12). The test was conducted along a 30-meter flat, straight surface at the clinic and subjects were requested to walk the maximum possible distance within six minutes, which was documented in meters. At T1 and T2 the test was carried out only once for each patient. Subjects were encouraged to walk as fast as possible and repeatedly asked to keep their walking speed. Heart rate, arterial blood pressure and peripheral oxygen saturation (pO2) were measured with commercial available devices (LCD Pulsoxymeter, Quirumed, 46113 Valencia, Spain) both at the beginning and at the end of the test. When respiratory or muscular fatigue occurred during 6-MWT, walking speed was reduced to a tolerable maximum and in case of severe exhaustion or cardio-pulmonary symptoms, the test was discontinued.
Statistical analysis
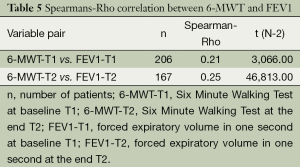
Statistical analysis was performed with the help of the statistics software Statistika Basis® (StatSoft GmbH, Hoheluftchaussee 112, D-20253 Hamburg, Germany). In order to demonstrate “Before (T1) and After (T2)” differences, the Wilcoxon signed-rank test was chosen as a non-parametric test for dependent and not normally distributed data with constant measurement level. A P-value <0.05 was considered statistically significant. To determine a correlation between the results of 6-MWT and FEV1 at points T1 and T2, the Spearman’s rho rang correlation coefficient was calculated and represented in relation to the severity of the respiratory functional impairment. A rho value of 0.2 to 0.29 was interpreted as a low correlation. Pre-specified subgroup analysis were performed by stratifying subjects according surgical procedure (Lobectomy, Pneumonectomy and Wedge-/segment resection) and severity FEV1 reduction [normal function FEV1 >80% predicted, slight dysfunction (70-80%), moderate dysfunction (50-69%), severe dysfunction <50%].
Results
Patient characteristics
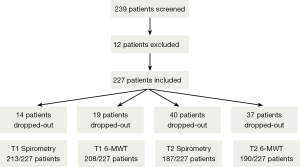
There were 239 subjects, who underwent rehabilitation after lung surgery from April 2010 to July 2010. Twelve subjects had exclusion criteria and the study cohort consisted of 227 subjects (Figure 1). Median age was 67 years (range, 33-87 years). With 120/227 (53%) subjects, male gender was slightly prevalent. On average, subjects were admitted to inpatient rehabilitation 25 days (range, 16-35 days) after lung operation and remained hospitalized for a median of 21 days (range, 8-42 days). The most frequently performed surgical technique was lobectomy in 108/227 subjects (47%) followed by wedge- and segment resection in 97/227 subjects (43%) and pneumonectomy 22/227 subjects (10%). The most common tumor diagnosis was NSCLC with 166/227 subjects (73%), followed by lung cancer of other histology in 26/227 subjects (12%) as well as pulmonary metastasis due to a solid extrapulmonary primary tumor (35/227 subjects, 15%). In the latter group there were 11 subjects with urothelial-/renal cell carcinoma, 8 subjects with colorectal carcinoma, 5 subjects with malignant melanomas and another 10 subjects with lung metastases of various other solid tumors. Depending on the tumor diagnosis, the selected surgical technique was lobectomy or pneumonectomy in subjects with primary lung cancer, each with systematic lymphadenectomy. Whereas wedge- and segment resection was used in metastasis surgery.
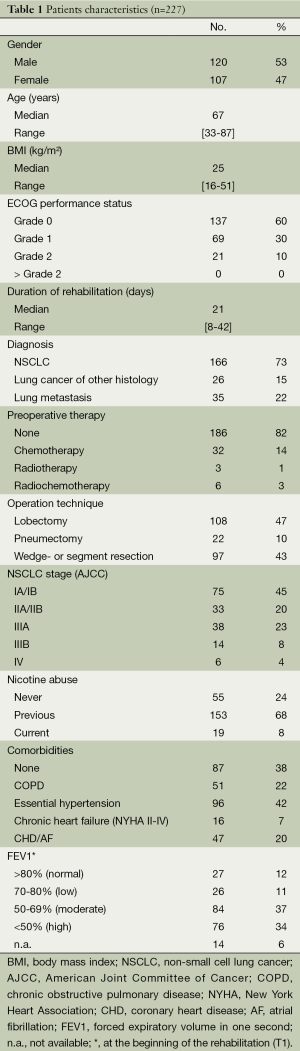
As expected, a history of smoking or active smoking was present in a large percentage (76%) of all lung cancer subjects. Clinically relevant comorbidities were found in 62% of the subjects, in particular COPD (22%), arterial hypertension (42%), compensated chronic heart failure (7%) and coronary heart disease (CHD) as well as chronic atrial fibrillation (20%). Patient characteristics are shown in Table 1.
Full table
Lung function parameters in spirometry
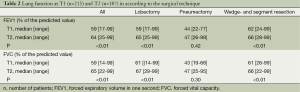
At T1, 213/227 subjects (94%) and at T2, 187/227 subjects (82%) could be evaluated with regard to spirometry parameters or delivered plausible values, respectively. The median time interval between T1 and T2 spirometry was 20 days (range, 17 to 23 days). In the overall cohort, when comparing parameters, there was a statistically significant improvement of the respiratory function from T1 to T2. Both FEV1 and FVC improved from median 59% to 64% and from 59% to 65% (P<0.01), respectively. This effect was observed after both lobectomy and wedge- and segment resection. There was no statistically significant improvement of the lung function parameters in the subgroup of subjects after pneumonectomy (Table 2). Improvements were not affected by co-morbidities such as COPD, arterial hypertension and CHD/chronic atrial fibrillation. In the subgroup of subjects with chronic compensated heart failure, there were no significant differences between FEV1 and FVC at T1 and T2 (data not shown).
Full table
Measurement parameters of 6-MWT
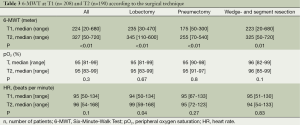
At T1, 208/227 subjects (92%) and at T2, 190/227 subjects (84%) could complete 6-MWT. For the overall cohort as well as for each of the three subgroups with regard to surgical technique (lobectomy, pneumonectomy, wedge- and segment resection) a significant improvement of the distance walked was observed in 6-MWT (P<0.01). Except for a borderline significant improvement of heart rate in subjects who underwent lobectomy (P=0.04), there was no relevant change. Measurement of pO2 did not show any significant difference in the comparison between T1 and T2 either (Table 3).
Full table
Within the scope of further subgroup analyses, a statistically significant improvement of the distance walked was found in 6-MWT with regard to comorbidities (COPD, arterial hypertension, chronic compensated heart failure, CHD/chronic atrial fibrillation) and to smoking behavior (data not shown). Chemotherapy performed prior to lung surgery did not influence 6-MWT and a statistically significant improvement of the walking distance at T1 and at T2 was observed in this subgroup as well (data not shown). Most likely due to the low number of subjects in the subgroups of radio- or radiochemotherapy, respectively (cf. Table 1), there was no significant difference between the distances walked at T1 and at T2 (data not shown).
Correlation of the walking distance with FEV1
With regard to their lung function at T1, subjects were divided into four groups according to their FEV1-value. The group without clinically relevant restriction (FEV1 >80%) counted 27/227 subjects (12%). The same number of subjects (26/227, 11%) were in the group with slight respiratory dysfunction (FEV1, 70-80%). Moderate (FEV1, 50-69%) and severe respiratory dysfunction (FEV1 <50%) was found in the majority of subjects (160/227, 71%) (Table 1). In all four groups, a statistically significant improvement of the walking distance was observed in 6-MWT in comparison between T1 and T2 with P<0.001 (Table 4). However, the correlations between the values of the walking distance in 6-MWT and the FEV1 within the scope of spirometry at T1 (rho value =0.21) and at T2 (rho value =0.25) are low (Table 5).

Full table
Full table
Discussion
The 6-MWT is an established diagnostic procedure and well-validated across various age groups, in healthy subjects and in subjects with various cardiac and pulmonary diseases (13). The 6-MWT is used in particular in pulmonary hypertension, COPD exacerbations and chronic heart failure. In healthy subjects and in subjects with COPD, the 6-MWT closely correlates with FEV1 and the partial pressure of oxygen measured on a blood gas analysis (14,15). To the best of our knowledge this is the first study investigating the 6-MWT before and after inpatient rehabilitation in subjects, who had undergone lung surgery related to a malignant disease. In this study we identified a statistically significant improvement of the walking distance measured during 6-MWTs as well as of FEV1 and FVC after inpatient rehabilitation.
However, no improvement with regard to FEV1 and FVC was detected in subjects, who underwent pneumonectomy. Despite the absence of improved FEV1 and FVC in pneumonectoy group the 6-MWT showed a significant improvement after rehabilitation cohort. This finding is likely explained by the multi-dimensional effect of inpatient rehabilitation, which, however, can affect the performance during a 6-MWT. Apart from subjects after pneumonectomy, improvement of the walking distance in 6-MWT as well as lung function parameters (FEV1 and FVC) was not affected by the surgical technique (Tables 2 and 3). Moreover, the improvement of both walking distance and lung function values was also not affected by pretreatment. This, however, needs to be interpreted with caution due to the low number of individuals in this subgroup. Irrespective of the severity of the pulmonary dysfunction, graduated by FEV1 at the beginning of rehabilitation (T1), significant improvement of the walking distance was observed. In particular the subgroups with moderate and severe pulmonary dysfunction counted a sufficient number of subjects, so that walking distance has proven to be a reliable parameter at least in these subgroups (Table 4).
Regarding the relationship of the walking distance on 6-MWT with FEV1 at T1 and T2 respectively, at both time points a low correlation of the two parameters (spearman’s rho for T1 =0.21 and for T2 =0.25) was observed. Thus, it can be postulated that besides FEV1 and FVC also the 6-MWT walking distance can be considered a clinical relevant parameter representing aspects of respiratory function. However, the rho values must be interpreted with caution. The patient cohort examined here is a very heterogeneous one with various tumor diseases. The largest group was composed of subjects with NSCLC, even though there were also subjects with pulmonary metastases of other solid tumor diseases. Even 26 subjects with lung cancer of other histology were included, who did undergo also functionally effective lobectomy or pneumonectomy. In the parameters of both 6-MWT and FEV1 and FVC, there are very large ranges, which suggest a highly inhomogeneous patient cohort with regard to pulmonary function. In particular the very low values in 6-MWT as well as in spirometry were due to subjects who underwent pneumonectomy and to partly very old subjects with multiple co-morbidities. Twenty-two percent of the subjects had a previously known COPD already at baseline, which has possibly affected the lung function parameters in a negative way as well. In literature it is well described that a preoperative restriction of lung function with low FEV1 can only account for a slight improvement of the postoperative walking distance (16,17). Unfortunately in our analysis no data are available on preoperative pulmonary function and diffusing capacity.
An improvement of the pO2 values as well as of heart rate, measured within the scope of 6-MWT, could not be shown. This negative result in our study was most likely due to the high median oxygen saturation values, which existed already at T1, and which have not improved any further in the remaining course of the study. Moreover, it is mentioned in literature that in particular pO2 does not represent an exact measurement method for lung function or a patient’s capacity (18).
Heart rate measurement in 6-MWT at T1 and T2 has not shown any significant change either, while the range was rather large. In particular this large range can be put down to heterogeneous training conditions, comorbidities, postoperative morbidity and subjects’ age.
In conclusion, it can be stated based on the available data that walking distance in 6-MWT has a low correlation with the values measured by spirometry, such as FEV1. Measuring the walking distance could be a suitable parameter to assess the respiratory function in patients after lung surgery related to pulmonary tumor manifestations. Measuring the pO2 or heart rate in 6-MWT is not suitable for this purpose. As a simple and cost-effective test, 6-MWT should therefore be firmly established in functional diagnostics in tumor patients after lung surgery.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Wasserman K, Hansen JE, Sue DY, et al. eds. Principles of Exercise Testing & Interpretation: Including Pathophysiology and Clinical Applications. Lippincott Williams & Wilkins, 1999.
- Weisman IM, Zeballos RJ. An integrated approach to the interpretation of cardiopulmonary exercise testing. Clin Chest Med 1994;15:421-45. [PubMed]
- Balke B. A simple field test for the assessment of physical fitness. REP 63-6. Rep Civ Aeromed Res Inst US 1963:1-8.
- Cooper KH. A means of assessing maximal oxygen intake. Correlation between field and treadmill testing. JAMA 1968;203:201-4. [PubMed]
- Butland RJ, Pang J, Gross ER, et al. Two-, six-, and 12-minute walking tests in respiratory disease. Br Med J (Clin Res Ed) 1982;284:1607-8. [PubMed]
- Solway S, Brooks D, Lacasse Y, et al. A qualitative systematic overview of the measurement properties of functional walk tests used in the cardiorespiratory domain. Chest 2001;119:256-70. [PubMed]
- Kessler R, Faller M, Fourgaut G, et al. Predictive factors of hospitalization for acute exacerbation in a series of 64 patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1999;159:158-64. [PubMed]
- Bernstein ML, Despars JA, Singh NP, et al. Reanalysis of the 12-minute walk in patients with chronic obstructive pulmonary disease. Chest 1994;105:163-7. [PubMed]
- Holden DA, Rice TW, Stelmach K, et al. Exercise testing, 6-min walk, and stair climb in the evaluation of patients at high risk for pulmonary resection. Chest 1992;102:1774-9. [PubMed]
- Sinclair DJ, Ingram CG. Controlled trial of supervised exercise training in chronic bronchitis. Br Med J 1980;280:519-21. [PubMed]
- Roomi J, Johnson MM, Waters K, et al. Respiratory rehabilitation, exercise capacity and quality of life in chronic airways disease in old age. Age Ageing 1996;25:12-6. [PubMed]
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 2002;166:111-7. [PubMed]
- Morales-Blanhir JE, Palafox Vidal CD, Rosas Romero Mde J, et al. Six-minute walk test: a valuable tool for assessing pulmonary impairment. J Bras Pneumol 2011;37:110-7. [PubMed]
- Leite Rodrigues S, Mendes HF, Viegas CA, et al. Six minutes walk test: study of the effect of learning in chronic obstructive pulmonary disease patients. J bras pneumol 2004;30.
- Camarri B, Eastwood PR, Cecins NM, et al. Six minute walk distance in healthy subjects aged 55-75 years. Respir Med 2006;100:658-65. [PubMed]
- Nomori H, Watanabe K, Ohtsuka T, et al. Six-minute walking and pulmonary function test outcomes during the early period after lung cancer surgery with special reference to patients with chronic obstructive pulmonary disease. Jpn J Thorac Cardiovasc Surg 2004;52:113-9. [PubMed]
- Pompili C, Brunelli A, Refai M, et al. Does chronic obstructive pulmonary disease affect postoperative quality of life in patients undergoing lobectomy for lung cancer? A case-matched study. Eur J Cardiothorac Surg 2010;37:525-30. [PubMed]
- Enright PL. The six-minute walk test. Respir Care 2003;48:783-5. [PubMed]


